Abstract
Results of two methods, conventional open reduction–internal plating and minimally invasive plating osteosynthesis (MIPO), in the treatment of mid-distal humeral shaft fractures were compared. Thirty-three patients were retrospectively analysed and divided into two groups. Group A (n = 17) patients were treated by MIPO and group B (n = 16) by conventional plating. The mean operation time in group A was 92.35 ± 57.68 minutes and 103.12 ± 31.08 minutes in group B (P = 0.513). Iatrogenic radial nerve palsy in group A was 0% (0/17) and 31.3% in group B (5/16 (P = 0.012). The mean fracture union time in group A was 15.29 ± 4.01 weeks (range 8–24 weeks), and 21.25 ± 13.67 weeks (range 10–58 weeks) in group B (P = 0.095). The mean UCLA end-result score in group A was 34.76 ± 0.56 points (range 33–35), and 34.38 ± 1.41 points (range 30–35) in group B (P = 0.299). The mean MEPI in group A was 99.41 ± 2.43 points (range 90–100) and 99.69 ± 1.25 points (range 95–100) in group B ( P = 0.687). When compared to the conventional plating techniques, MIPO offers advantages in terms of reduced incidence of iatrogenic radial nerve palsies and accelerated fracture union and a similar functional outcome with respect to shoulder and elbow function.
Résumé
Les résultats de deux méthodes d’ostéosynthèse par plaques après réduction sanglante conventionnelle voie mini-invasive (MIPO) dans le traitement des fractures médio-diaphysaires de l’humérus ont été comparées. 33 patients ont été revus rétrospectivement et analysés et divisés en deux groupes : le groupe A (n = 17), traité par MIPO et le groupe B (n = 16) traité de façon conventionnelle. Le temps opératoire moyen dans le groupe A était de 92,35 +/−57,68 minutes et 103,12+/−31,08 minutes dans le groupe B (P = 0,513). Il n’a pas été observé de paralysies iatrogéniques du nerf radial dans le groupe A, par contre, dans le groupe B sont survenues 31,3% de paralysies 5/16 (p = 0,012). Le temps moyen de consolidation dans le groupe A a été de 15,29+/−4,01 semaines (8 à 24 semaines) et, dans le groupe B, de 21,25+/−13,67 semaines (10 à 58 semaines) (P = 0,095). Le score final UCLA dans le groupe A était de 34,76+/−0,56 points (33 à 35 points) et dans le groupe B de 34,38+/−1,41 points (30 à 35) (P = 0,299). Le MEPI moyen dans le groupe A a été de 99,41+/−2,43 points (de 90 à 100) et dans le groupe B de 99,69+/−1,25 points (95 à 100) (P = 0,687). Si l’on compare les deux techniques, la technique par voie mini-invasive (MIPO) permet de réduire la fréquence des paralysies du nerf radial, permet une consolidation plus rapide et une fonction similaire notamment au niveau de l’épaule et du coude.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Various methods are used to treat mid-distal third humeral shaft fractures. Most of the fractures can be effectively treated conservatively [1, 2]. Operative intervention is indicated in special circumstances including (1) failure of closed reduction, (2) intra-articular extension of fractures, (3) neurovascular compromises, (4) associated ipsilateral forearm and elbow fractures, (5) segmental fractures, (6) pathological fractures, (7) open fractures, (8) fractures in polytraumatised patients, (9) bilateral humeral shaft fractures, (10) periprosthetic fractures and (11) transverse or short oblique fractures [3]. These fractures can be surgically treated by either using a dynamic compression plate [4, 5] or intramedullary nails [5–8]. Although controversy exists over which is the better technique, most authors believe that open reduction and internal fixation with a dynamic compression plate is a more reliable method. The advantages include anatomical reduction of fractures and less interference to elbow and shoulder function [4, 9]. The major disadvantages of this technique, however, are extensive soft tissue stripping and disruption of periosteal blood supply, which increase the risk of nonunion and iatrogenic radial nerve palsies [10–12]. It has been reported that humeral shaft fractures can be successfully treated with minimally invasive plating osteosynthesis (MIPO) [13–17]. This technique has advantages of less soft tissue dissection and avoids the need to expose the radial nerve; thus, there is also low risk of iatrogenic radial nerve palsies [14]. These advantages appear to indicate that MIPO is superior to conventional plating osteosynthesis. However, there is no large series that reports advantages and disadvantages of MIPO compared to conventional plating osteosynthesis technique. The purpose of this retrospective study was to compare the clinical results of two groups of patients: those treated with MIPO and the other treated by conventional open reduction and plating osteosynthesis.
Patients and methods
Study group
Patients with closed displaced unstable middle or/and distal third humeral shaft fractures without radial nerve palsies who were treated by either conventional open reduction and plating osteosynthesis or by MIPO technique were included.
Exclusion criteria
The following patients were excluded:
-
(1)
Patients with mid-distal third shaft fractures associated with radial nerve injuries
-
(2)
Patients with open fractures
-
(3)
Skeletally immature patients
-
(4)
Patients with pathological fractures
-
(5)
Patients in which time lag between injury and surgical intervention exceeded three weeks
Study period and location
From March 2004 to October 2006, 43 cases (29 males, 14 females) of mid-distal third humeral shaft fractures, with average age of 39.53 years (19–62 years), were surgically stabilised by plating osteosynthesis in Shanghai Sixth People’s Hospital.
Thirty-three cases of isolated mid-distal third humeral shaft fractures were matched for inclusion criteria. The patients were divided into two groups: patients treated by the MIPO technique (group A) and patients treated by open reduction and plating internal fixation (group B).
There were 17 cases in group A (12 males, five females) with average age of 37.59 ± 9.20 years (19–60 years). The left arm was involved in ten cases and the right arm in seven. Causes of injuries were road traffic accidents in nine patients, entanglement in machines in five, and falls in three. Eight fractures involved the middle third humeral shaft and nine the distal third. Three cases had associated injuries including a pelvic fracture, which did not need operative treatment, an ipsilateral distal radial and a surgical neck fracture that was treated by open reduction and internal fixation with a plate in each case.
There were 16 cases in group B (nine males and seven females) with mean age of 36.93 ± 11.40 years (24–62 years). The left and right arms were involved in eight cases each. Six cases were caused by injury from a fall, three by entanglement in machines and six by road traffic accident. Nine fractures involved the middle third humeral shaft and seven the distal third. One case in this group was associated with lung contusion and fractures of the sixth and seventh ribs.
All humeral shafts in both groups were classified according to the OTA classification system [18].
Operative procedures
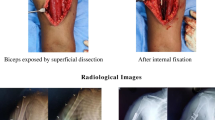
The operative techniques applied in group A were similar to that previously described in literature [14]. Obtaining closed reduction was the crucial step in the whole procedure, which was done under image guidance. Two small incisions were made on the anterior side of the arm, proximal and distal to the fracture site. A submuscular extraperiosteal tunnel was prepared between the brachial muscle and underlying periosteum with a narrow periostal elevator inserted first from the proximal incision distally and then from the distal incision proximally. Through this tunnel a straight, noncontoured, long, narrow, 4.5-mm dynamic compression plate (DCP, 10–12 holes) was inserted from the proximal incision, passing the fracture site and down to the distal incision. At least three screws and six cortices were inserted in each of the main fracture fragment. One of the screws was percutaneously inserted by an additional stab incision. The radial nerve was not exposed during the whole procedure. Wound closure was done in the standard fashion, no drain tube was used (Fig. 1).
For the patients in group B, open reduction and internal fixation with a plate were performed by conventional anterolateral or posterior approaches centred on the fracture site with patients in a supine or prone position and the arm on a radiolucent board. The radial nerve was exposed and carefully protected in both the approaches. The fracture sites were dissected and haematoma and soft tissue interposing between the fragments were removed. The fractures were reduced and a straight 4.5-mm dynamic compression plate was applied to fix the fractures with at least three screws in each end of the plate. The stability of the bone–plate construction was examined by passive motion of the shoulder and the elbow. The wound was closed after placing a drainage tube sub-muscularly. Eleven cases in this group were operated upon via a posterior approach and five by an anterolateral approach.
Postoperative treatments in both groups were the same except for removing the drainage tube in group B. The arms were immobilised with a collar and cuff sling and the patients were encouraged to move the shoulders and elbows early, usually three days after surgery in both groups. The stitches were removed two weeks after surgery. All patients were followed-up at four-week intervals for the first three months after the surgery and at eight-week intervals for the next three months after surgery. The range of motion of the shoulders and elbows were recorded. Radiographs of the injured arm were taken. More active exercises were started when callus appeared.
For data collection the operative time was defined as the time from the skin incision to skin closure. Also recorded were the fracture union time, perioperative complications, late complications, and shoulder and elbow function. The data regarding shoulder and elbow function were collected and assessed by one surgeon who was not associated with the surgical procedure or the care of the patients. Union was defined as the absence of pain and the presence of bridging callus in three of the four cortices seen on the anteroposterior and lateral radiographic views of the humerus. Shoulder function was assessed using the UCLA scoring system [19], the parameters including pain (10 points), motion (10 points), function (10 points), and patient satisfaction (5 points). Subjective criteria constitute 15 points of a total of 35 points, and the findings on examination comprise the remaining 20 points. The scores were further divided into excellent (34–35 points), good (29–33 points), fair (21–28 points), and poor (0–20 points) according to Ellman [20]. Elbow function was assessed using the Mayo elbow performance index (MEPI) [21], which evaluates patients on a 100-point scale regarding pain (45 points), range of motion (20 points), stability (10 points) and function (25 points). Function of the joint is classified as excellent (>90 points), good (75 to 89 points), fair (60 to 74 points) or poor (<59 points).
Statistical analysis was performed using SPSS software, version 11.0 (SPSS, Inc., Chicago, IL, USA). The patient demographics (sex, injured side, rate of associated injuries, rates of postoperative complications) and fracture characteristics of the two treatment groups were compared using the Pearson’s chi-square test or Fisher’s exact test for nonparametric categorical variables. Independent sample t test was used to compare the result of patients’ age, duration of injury, operation time, duration of follow-up, bone healing time, motion of the shoulder and elbow and score of UCLA and MEPI. The level of significance was set at p < 0.05.
Results
There was no significant difference in mean age (t = 0.181, P = 0.858), gender (χ2 = 0.732, P = 0.392), injured side (χ2 = 0.259, P = 0.611), type of the fractures (χ2 = 5.308, P = 0.070) or associated injuries (χ2 = 1.005, P = 0.316) between the two groups. The mean duration of injury for group A was 5.59 ± 1.80 days (range 3–9 days), while for group B it was 6.50 ± 3.58 days (range 2–13 days). There was no statistical significance between the two groups (t = 0.933, P = 0.358).
The mean operation time was 92.35 ± 57.68 minutes (range 70–195) in group A and 103.12 ± 31.08 minutes (range 60–160) in group B (t = 0.662, P = 0.513).
The occurrence of iatrogenic radial nerve palsy in group B, 31.3%(5/16), was significantly higher than in group A, 0% (0/17) (t = 6.261, P = 0.012).
The mean period of follow-up in group A was 25.94 ± 9.30 months (range 14–44), while in group B it was 32.88 ± 12.62 months (range 13–48) (t = 1.805, P = 0.081).
The mean fracture union time was 15.29 ± 4.01 weeks (range 8–24) in group A and 21.25 ± 13.67 weeks (range 10–58) in group B. The mean fracture union time in group B was longer than that in group A, but there was no statistically significant difference between the two groups (t = 1.722, P = 0.095). Figure 1 shows results of a typical case treated with the MIPO technique.
One case (6.3%) of delayed union occurred in group B which resulted from loosening of the screws in the proximal end of the plate. The patient was treated nonoperatively and the fracture united 17 months after operation (Fig. 2). There was no incidence of infection or implant failures in either group. All five iatrogenic radial nerve palsies spontaneously recovered with mean onset time of 22.4 weeks (range 12–52 weeks) without any surgical interference. The implants were removed in five cases in group A and three cases in group B without any complications.
At the latest visit, the mean active anterior forward flexion of affected shoulder in group A was 166.76 ± 5.57 degrees (range 150–170), while it was 165.00 ± 7.30 degrees (range 150–170) in group B (t = 0.783, P = 0.439). The mean UCLA end-result score in group A was 34.76 ± 0.56 points (range 33–35) and 34.38 ± 1.41 points (range 30–35) in group B (t = 1.056, P = 0.299).
There was no statistically significant difference in the range of motion (ROM) and MEPI between the two groups. The mean ROM was 132.94 ± 10.01 degrees (range 100–140) in group A and 136.50 ± 5.10 degrees (range 120–140) in group B (t = 1.274, P = 0.212). The mean MEPI was 99.41 ± 2.43 points (range 90–100) in group A and 99.69 ± 1.25 points (range 95–100) (t = 0.407, P = 0.687) in group B. There were no significant postoperative deformities in either group.
Discussion
In comparison with open reduction and internal fixation using a plate, one of the major theoretical advantages of MIPO with an anteriorly placed plate to treat mid-distal humeral shaft fractures is less surgical trauma to the soft tissue around the fracture site. The periosteal circulation around the fracture fragments is minimally disrupted and thus bone union is promoted and complications such as nonunion are decreased. In a study by Paris et al., the rate of nonunion after plating fixation was 5.8% (8/138 humeral shaft fractures) [11]. In this retrospective comparison study, although all the fractures treated with plating osteosynthesis finally united without secondary surgical interference, the union time of fractures treated by the MIPO technique was 15 weeks, while the fracture union time of the patients treated by the open reduction technique was 21 weeks, much longer than patients treated by MIPO. There was also a case of delayed union in the group treated by open reduction. Although there is no statistical significance between the two groups, the result is very close to threshold value and shows a definite trend. This may be due to relatively small number of cases in the study and, with larger study groups, the results may show statistical significance.
Another advantage of MIPO is that the radial nerve does not need to be dissected, although it is very important to carefully expose and protect the radial nerve during the entire procedure of open reduction and internal plating fixation. Despite the stress on meticulous radial nerve protection, the incidence of iatrogenic radial palsies following this procedure is reported to be from 5.1% [11] to 17.6% [10] in different series in the literature.
According to Apivatthakakul et al., when a plate is placed on the anterior side of humeral shaft the mean distance from the closest part of the plate to the radial nerve is 3.2 mm [13]. The brachial muscle that covers most of the anteriorly placed plate protects the radial nerve from injury when a plate is inserted sub-muscularly through two small incisions on the anterior side of the arm away from fracture site. Pospula et al. reported only one case of iatrogenic radial nerve palsy when the MIPO technique was used to treat 12 cases of humeral shaft fractures [22], while Ji et al. reported one in 23 humeral shaft fractures [17]. Livani et al. reported good results in 35 cases of mid-distal humeral shaft fractures without iatrogenic radial nerve lesions [16]. The clinical outcomes reported in this series also show low (zero) occurrence of iatrogenic radial nerve palsies, which is consistent with that of earlier series [14, 16].
The functional outcomes assessed by UCLA end-result score and Mayo elbow performance score systems in the affected shoulder and elbow in the two groups were also consistent with that previously reported in literature [4, 11, 12], showing that the anteriorly placed plates have little influence on shoulder and elbow function.
This study however has some limitations. The incidence of iatrogenic radial nerve palsies in the open reduction patients is 31.3%, higher than most series have reported. Although this may be attributed to a difference in surgical skills of surgeons in different groups, surgeons in both groups were equally competent and held equivalent posts. The fact that there was no case of radial nerve palsy occurring in the MIPO group demonstrates its superiority over the conventional technique even when compared to historical control data of pre-existing literature. As with any other retrospective study, there is scope for selection bias; however, the groups were properly matched for age, sex, injured side, OTA classification, mean duration between surgery and the occurrence of injuries and associated injuries. This study is small when considered statistically, but compared to available literature we believe that it is one of the largest comparative studies, although a greater number of patients would help to validate this method of treatment conclusively.
From this retrospective comparative study, the authors concluded that mid-distal third humeral shaft fractures could be effectively treated with the MIPO technique, with advantages of shorter fracture union time and lower incidence of iatrogenic radial nerve palsies but with similar functional outcomes to the conventional open plating technique.
References
Ekholm R, Tidermark J, Törnkvist H, Adami J, Ponzer S (2006) Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 20(9):591–596
Toivanen JA, Nieminen J, Laine HJ et al (2005) Functional treatment of closed humeral shaft fractures. Int Orthop 29(1):10–13
Schemitsch EH, Bhandari M (2003) Fractures of the humeral shaft. In: Browner BD, Jupiter JB, Levine AM, Trafton PG (ed) Skeletal trauma: basic science, management, and reconstruction, 3rd edn. WB Saunders Company, pp 1487–1488
Niall DM, O’Mahony J, McElwain JP (2004) Plating of humeral shaft fractures—has the pendulum swung back? Injury 35(6):580–586
Changulani M, Jain UK, Keswani T (2007) Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop 31(3):391–395
Fernandez FF, Matschke S, Hulsenbeck A et al (2004) Five years’ clinical experience with the unreamed humeral nail in the treatment of humeral shaft fractures. Injury 35(3):264–271
Petsatodes G, Karataglis D, Papadopoulos P et al (2004) Antegrade interlocking nailing of humeral shaft fractures. J Orthop Sci 9(3):247–252
Pogliacomi F, Devecchi A, Costantino C, Vaienti E (2008) Functional long-term outcome of the shoulder after antegrade intramedullary nailing in humeral diaphyseal fractures. Chir Organi Mov 92(1):11–16
Bhandari M, Devereaux PJ, McKee MD et al (2006) Compression plating versus intramedullary nailing of humeral shaft fractures—a meta-analysis. Acta Orthop 77(2):279–284
Lim KE, Yap CK, Ong SC et al (2001) Plate osteosynthesis of the humerus shaft fracture and its association with radial nerve injury—a retrospective study in Melaka General Hospital. Med J Malaysia 56(Suppl C):8–12
Paris H, Tropiano P, Clouet D’orval B et al (2000) Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot 86(4):346–359
Jawa A, McCarty P, Doornberg J et al (2006) Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am 88(11):2343–2347
Apivatthakakul T, Arpornchayanon O, Bavornratanavech S (2005) Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury 36(4):530–538
Zhiquan A, Bingfang Z, Yeming W et al (2007) Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma 21(9):628–633
Ziran BH, Belangero W, Livani B et al (2007) Percutaneous plating of the humerus with locked plating: technique and case report. J Trauma Inj Infect Crit Care 63(1):205–210
Livani B, Belangero W, Andrade K et al (2008) Is MIPO in humeral shaft fractures really safe? Postoperative ultrasonographic evaluation. Int Orthop. doi:10.1007/s00264–008–0616-x
Ji F, Tong D, Tang H et al (2008) Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop. doi:10.1007/s00264–008–0522–2
Orthopaedic Trauma Association (1996) Fracture and dislocation compendium. J Orthop Trauma 10(Suppl 1):1–55
Ellman H, Hanker G, Bayer M (1986) Repair of the rotator cuff. J Bone Joint Surg Am 68:1136–1144
Ellman H (1987) Arthroscopic subacromial decompression: analysis of 1 to 3 year results. Arthroscopy 3:173–181
Gill DR, Morrey BF (1998) The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am 80:1327–1335
Pospula W, Abu Noor T (2006) Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital, Kuwait. Med Princ Pract 15(6):423–426
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
An, Z., Zeng, B., He, X. et al. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. International Orthopaedics (SICOT) 34, 131–135 (2010). https://doi.org/10.1007/s00264-009-0753-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-009-0753-x