Abstract
Background
To evaluate the effect of lumbar microdiscectomy (LM) in pain, disability and quality of life in a 5-year period and to identify potential demographic and clinical risk factors.
Methods
One hundred patients who underwent LM by the same surgeon participated in this prospective study. Clinical assessment was made with validated questionnaires preoperatively and up to 5 years postoperatively. Subsequently, associations between clinical outcomes and demographic data were recorded.
Results
In every assessment questionnaire, there was a significant improvement in the first postoperative month, which lasted up to 1 year post-discectomy. After that, improvement was statistically significant (p < 0.05) but without clinical importance. Women reported more pain preoperatively and 1 month after surgery. Urban residents also presented more pain preoperatively. Older patients had more pain, disability and worse quality of life 1–5 years postoperatively. Similarly, patients with lower education presented the worst scores in every questionnaire at the same time. Smokers reported less pain 1.5–4 postoperative years. Higher alcohol consumption and obesity were associated with lower levels of preoperative pain. However, obese patients had worse SF-36 and ODI scores after the 6th postoperative month. Patients with heavy jobs presented the worst preoperative ODI scores.
Conclusion
Significant clinical improvement was recorded from the first postoperative month to the first postoperative year; stabilization was noticed later on. Feminine gender, urban residency, older age, low level of education, obesity and heavy physical occupation were negative prognostic factors. Oddly smoking and alcohol were correlated with less pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation (LDH) is a common spinal disorder with an estimated 1-year incidence of 0.1–0.5% [1]. It has a lifetime incidence of approximately 1–2% and is the most commonly operated spinal diagnosis [2]. Microdiscectomy is generally considered a common procedure for removing the herniated portion of a disc that is pressing on a nerve, as it has a long history and many spine surgeons have extensive expertise in this approach. Satisfactory results after lumbar discectomy have been reported in about 60–80% of the patients [3]. In this study, the effect of LM in pain, disability and quality of life was recorded for 5 years after surgery and associations between clinical parameters and demographic data were assessed.
Materials and methods
This prospective study was conducted from January 2005 to June 2017 and approved by the University of Ioannina Medical School ethics committee, and each patient’s written informed consent was obtained. It is a continuation of a study that recorded magnetic resonance imaging (MRI) changes in lumbar spine 5 years after microdiscectomy. One hundred patients who underwent LM for an MRI-verified single-level LDH between January 2005 and June 2012 were initially enrolled. All participants had medical indication for surgical treatment, since the majority of them were symptomatic with chronic pain or required emergency surgery due to neurological symptoms.
Ninety-one patients with a mean age of 45.26 (SD ± 12.33) at the time of surgery participated in the study. The majority of patients (52 patients, 57.1%) were females. They were mainly urban residents (49 patients, 53.8%). Twenty-nine patients (31.9%) were rural, and 13 (14.3%) were semi-rural residents. Most participants (n = 51, 56%) received secondary education, 23 (25.3%) received primary education, and 17 patients (18.7%) had a university degree. Preoperatively, 43 patients (47.3%) were overweight (BMI = 25.00–29.99) according to World Health Organization body mass index (BMI) classification, 36 (39.6%) patients’ BMI was within the normal range (18.50–24.99), and 12 patients (13.2%) were classified as obese class I (BMI = 30.00–34.99). Thirty-five patients (38.5%) had a heavy physical job before the operation, 30 (33.0%) classified as having moderate work intensity, 16 patients (17.5%) had a sedentary work, 5 patients (5.5%) had a job with minimal physical activity, and 5 patients were not working preoperatively.
Lumbar microdiscectomy was performed in all patients by the same experienced orthopaedic spine surgeon using identical surgical protocol. Patients had needles as a preoperative marker of localization [4]; the appropriate level was confirmed by intraoperative X-ray. The technique used was limited discectomy, and it included the removal of the LDH through a limited surgical approach while permitting adequate nerve root decompression. A small incision (less than 2.5 cm) was made in the skin. Muscles then were gradually retracted from the lamina to gain access to the interlaminar space, and the yellow ligament was removed; meticulous attention was paid to minimize the disruption of epidural soft tissues. Only the ruptured portion of the disc was removed to decompress the spinal nerve root. Excessive disc removal and formal laminectomy were avoided. All operations were performed under general anaesthesia.
Exclusion criteria included more than one operative levels, lumbar spine trauma, history of lumbar spine reoperation, spinal or other infections and primary or secondary spinal tumour. Nine out of 100 patients were lost during follow-up; consequently, 91 patients (91%) with complete data considered eligible.
All perioperative data available, such as the duration of surgery, blood transfusion, postoperative infection, complications and the length of hospitalization, were collected. Demographic data, the duration of symptoms and the type of postoperative rehabilitation programme were recorded as well.
The visual analogue scale (VAS, a 0–10 numerical rating scale with 0 = no pain and 10 = worst possible pain), the Greek versions of Oswestry Disability Index (ODI Greek version 2.1a, used under licence from Mapi Research Trust), Roland Morris Disability Questionnaire (RMDQ) [5] and the SF-36 [Short Form 36 Health Survey. The Greek version of Optum™ SF-36v2® Health Survey and the Quality Metric Health Outcomes(tm) Scoring Software 4.5, used under licence from Quality Metric Incorporated, part of Optum Insight] were used to assess pain, disability due to low back pain and quality of life preoperatively and at 1, 6, 12, 18, 24, 36, 48 and 60 months postoperatively. Each questionnaire’s score changes during the 5-year follow-up were recorded and assessed. Statistical analyses were performed using the tests (t test, sign test, Wilcoxon signed-rank test, McNemar–Bowker test, Bonferroni method, logistic regression analysis) of Statistical Package for Social Sciences (SPSS 20.0, Chicago, IL, USA). p values < 0.05 were considered statistically significant; all p values were two-tailed.
Results
Forty-six out of 91 patients participating in the study (50.5%) were smokers, with a mean time of 26.56 pack-years of tobacco exposure before surgery. Sixty-eight patients (74.7%) reported no alcohol use preoperatively, according to the Alcohol Use Disorders Identification Test of World Health Organization (AUDIT, WHO). The mean alcohol consumption of the remaining 23 patients was 12.6 alcoholic beverages per week. Forty-four patients (48.4%) were operated for L4–L5 LDH, 43 patients (47.2%) for L5–S1, 2 patients (2.2%) for L2–L3, and 2 patients for L3–L4 LDH.
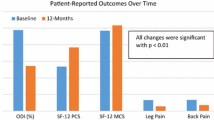
Preoperatively, the average VAS score was 9.27 (SD ± 1.15), the average ODI score was 84.86 (SD ± 13.57), the RMDQ average score was 19.93 (SD ± 3.44), and the SF-36 score was 26.34 (SD ± 2.11) for physical health and 21.82 (SD ± 7.02) for mental health. One month postoperatively the average scores in all questionnaires showed a significant clinical improvement. The VAS score was 2.26 (SD ± 2.47), ODI score was 51.17 (SD ± 18.98), RMDQ was 11.48 (SD ± 4.49), and the SF-36 score was 36.96 (SD ± 6.50) for physical and 40.87 (SD ± 5.55) for mental health. Improvement continued at 6 months (average scores for VAS = 0.97 ± 1.55, ODI = 18.11 ± 14.55, RMDQ = 2.92 ± 3.53, SF-36 = 50.66 ± 7.71 for physical and 51.24 ± 5.15 for mental health) and at 12 months post-LM (average scores for VAS = 0.74 ± 1.53, ODI = 13.82 ± 13.36, RMDQ = 1.45 ± 2.33, SF-36 = 53.04 ± 6.86 for physical and 51.47 ± 5.08 for mental health).
Eighteen, 24, 36 and 48 months after surgery, the average VAS score was 0.78 (SD ± 1.64), 0.92(SD ± 1.78), 0.73(SD ± 1.69) and 0.79(SD ± 1.52), respectively, ODI score was 12.33 (SD ± 12.40), 12.15 (SD ± 13.50), 11.18 (SD ± 12.86) and 12.00 (SD ± 13.05), respectively, and RMDQ score was 1.47 (SD ± 2.43), 1.78 (SD ± 3.14), 1.37 (SD ± 2.41) and 1.26 (SD ± 2.37), respectively. The average score of SF-36 was 52.88 (SD ± 7.26) for physical and 51.59 (SD ± 5.19) for mental health at 18 months, 52.62 (SD ± 7.88) for physical and 51.66 (SD ± 5.46) for mental health at 24 months, 52.91(SD ± 7.73) for physical and 51.18 (SD ± 5.86) for mental health at 36 months, 52.51(SD ± 7.76) for physical and 51.67 (SD ± 5.17) for mental health 48 months postoperatively. At the end of the 5-year follow-up period, the average VAS score was 0.81(SD ± 1.62), ODI score was 10.98 (SD ± 12.80), RMDQ was 1.13(SD ± 2.13), and the SF-36 score was 52.95(SD ± 7.48) for physical and 52.10 (SD ± 5.27) for mental health (Figs. 1, 2).
The mean operating time was 50 min, and the average duration of postoperative hospitalization was 3.4 days (SD ± 1.99). No major perioperative complications were recorded. After the discharge from hospital, two patients (2.2%) developed superficial surgical wound infection, one of whom (1.1%) had a fever and wound drainage that required hospitalization for 7 days. Three patients (3.3%) were reoperated 1, 12, 24 months after the initial surgery due to a true LDH recurrence (1 in L4–L5 and 2 in L5–S1 level), and one patient (1.1%) was reoperated 24 months after the initial surgery in order to remove fibrotic tissue pressing the S1 nerve root.
Comparing the mean score of each questionnaire with the mean score of the same questionnaire at the next follow-up assessment, a statistically significant difference (p < 0.05) was recorded every time. However, apart from the statistical significance, the clinical significance of these differences should also be assessed, especially if we take into consideration the mean scores of each questionnaire from the first postoperative year to the end of the 5-year follow-up period, as the VAS score is less than 1, ODI score ranges from 10.98 to 13.82, SF-36 score for physical health is 52.51–53.04, SF-36 score for mental health ranges from 51.18 to 52.10, and Roland Morris score is 1.13–1.78. The clinical significance of the differences between these values is not important, although in the statistical analysis they appear to be significant.
SPSS logistic regression analyses were performed to evaluate possible associations between demographic and clinical data. Women reported more pain in VAS than men preoperatively (p = 0.011, mean rank = 51.29) and 1 month after surgery (p = 0.046, mean rank = 50.53). Men reported better physical health in SF-36 for physical health than women at 36 (p = 0.014, mean rank = 53.83) and 48 months (p = 0.009, mean rank = 49.63) postoperatively. Urban residents presented more pain in VAS preoperatively than those living in rural (p = 0.042) and semi-rural (p = 0.031) areas. The older the patients were the more pain in VAS (p = 0.041–0.048), the higher disability in RMDQ (p = < 0.001–0.003) and the worse quality of life in SF-36 for physical health (p = 0.011–0.024) they reported 1–5 years postoperatively. Patients who received primary education had worse scores in VAS, ODI, RMDQ and SF-36 for physical health 1–5 years postoperatively than patients with secondary education (p = 0.003–0.049 for VAS, p < 0.001–0.023 for RMDQ, p = 0.023–0.047 for ODI, p < 0.001–0.019 for SF-36) and patients having a university degree (p = 0.001–0.009 for VAS, p < 0.001–0.03 for RMDQ, p = 0.017–0.037 for ODI, p < 0.001–0.022 for SF-36). Smokers reported less pain in VAS between 1.5 and 4th postoperative year (p = 0.008–0.04) than nonsmokers. Also drinking more alcohol was associated with lower levels of preoperative pain in VAS (p = 0.03). Obese patients (BMI > 30.00) presented less pain (VAS) preoperatively (p = 0.01) but worse quality of life (SF-36 for physical health) and ODI scores from the 6th postoperative month to the end of the follow-up period (p = 0.011–0.037 and 0.010–0.036, respectively). Finally, patients with a heavy physical job had the worst preoperative ODI scores (p = 0.045).
No association (p > 0.05) was found between sex, residential area, age, level of education, smoking, alcohol use, BMI, type of occupation, LDH level, duration of preoperative symptoms, postoperative physiotherapy or rehabilitation programme and the scores of VAS, ODI, RMDQ and SF-36 in the remaining, not already mentioned, evaluation periods. Reoperation due to real disc recurrence or due to pressure from fibrotic tissue was not statistically related to any clinical or demographic variable tested in this study (p from > 0.001–0.041).
Discussion
Except for patients with cauda equina syndrome, which is considered an indication for urgent surgery, operation is generally indicated when there is a combination of definite disc herniation shown by imaging, a corresponding syndrome of sciatic pain, a corresponding neurological deficit and a failure to respond to 6 weeks of conservative therapy [6]. It has been suggested that better outcomes come with early surgical treatment [7].
Although lumbar discectomy results in improvement in bodily pain, physical function and disability in the vast majority of patients [8, 9], same-level recurrent LDH complicates outcome for many patients and often requires revision surgery [10, 11]. Progressive degeneration and loss of height of the operative disc space [11,12,13,14,15], as well as new disc herniation at a different disc levels, arachnoiditis, foraminal stenosis and segmental instability [9, 13, 14, 16,17,18,19,20], can occur after lumbar discectomy, potentially contributing to long-term back and leg pain [9, 13, 14, 20]. Fibrosis-related complications are also causes of failed back surgery syndrome, and efforts have been made to reduce their incidence and severity [21, 22]. The rate of repeat interventions following primary discectomy ranges from 4 to 18% [14, 20, 23, 24]. In this study, we evaluated the effects of lumbar microdiscectomy in pain, disability and quality of life for a period of 5 years postoperatively and we assessed the importance of various demographic predictors in the results.
In the Maine Lumbar Spine Study [25], 70% of patients treated surgically for LDH reported initially improvement in their predominant symptom (back or leg pain); however, the relative benefit of surgery decreased over time. In the Spine Patient Outcomes Research Trial (SPORT) [8] on the other hand, the treatment effect for surgery was seen as early as 6 weeks, appeared to reach a maximum by 6 months and persisted over 8 years. In accordance with SPORT, significant clinical improvement was recorded in our study from the first postoperative month to the first postoperative year, which persisted with little to no degradation of outcomes between 1 and 5 years (Figs. 1, 2).
In the SPORT [26], patients with college education or more did very well with operative or nonoperative treatment and better than less-educated patients with nonoperative treatment, and obese patients did not benefit as much as nonobese. These findings are consistent with ours. In our study, both higher educational level and lower BMI were related to better postoperative clinical results. According to the SPORT, patients who saw more benefit from the surgical intervention for LDH include those with an upper lumbar LDH (L2–L3, L3–L4), but this was not confirmed by our study.
Huang et al. [27] in their systematic review and meta-analysis of the previous literature showed that BMI was significantly correlated with a higher incidence of recurrent LDH. On the other hand, Swartz and Trost [18], similarly to our study, found that the level of herniation, age, sex, smoking and symptom duration were not associated with recurrence. In our study, older patients and females presented worse clinical results, but smoking and alcohol use were paradoxically correlated with better scores in questionnaires at certain periods of follow-up time, although Akmal has demonstrated the toxicity of nicotine on bovine in vitro intervertebral disc cells [28].
With respect to occupational status, it is generally accepted that heavy physical labour leads to increased loading of lumbar disc, which may contribute to recurrent LDH [29]. We found that patients with a heavy physical job had worse ODI scores before surgery but they presented no postoperative differences compared to other patients. To our knowledge, regional assessment of the results after a lumbar discectomy has not been sufficiently presented in the literature. The only clinical effect of residential area we found was that urban residents presented more pain in VAS preoperatively than those living in rural and semi-rural areas. No postoperative differences were recorded.
The surgical treatment of sciatica with discectomy is not successful in a sizable percentage of patients, and its effectiveness is difficult to be measured, especially in those cases where patients were not reoperated. Most relevant studies in the bibliography usually use one or two questionnaires for clinical evaluation. In this prospective study, four validated questionnaires with a high degree of inter- and intraobserver agreement were used, combined with a high follow-up period of 5 years at regular intervals, depicting in our opinion adequately the clinical outcomes after microdiscectomy. In addition, all patients were operated by the same surgeon and treated under the same surgical and clinical protocol and the number of participants is considered satisfying. On the other hand, there was no control group in this study, since our University Hospital is region’s reference centre and the majority of patients presented had a medical indication for surgical treatment due to chronic pain or required an emergency surgery because of neurological symptoms. The results of our study can provide clinicians and patients with valuable information for informed decision-making and lead to good outcomes in carefully selected patients.
Conclusion
Significant clinical improvement was recorded from the first postoperative month to the first postoperative year; no clinically important improvement or aggravation was noticed later on. Females, urban residents, older patients, patients with lower level of education, patients having a heavy physical job and obese patients presented worse clinical scores. Although smoking and alcohol have been associated in bibliography with disc degeneration and recurrent LDH, in our study smokers and patients with higher alcohol consumption had better scores in questionnaires at certain periods of follow-up time. LDH level, duration of preoperative symptoms, postoperative physiotherapy or rehabilitation programme had no impact on clinical results.
Abbreviations
- AUDIT:
-
Alcohol Use Disorders Identification Test
- BMI:
-
Body mass index
- LDH:
-
Lumbar disc herniation
- LM:
-
Lumbar microdiscectomy
- MC:
-
Modic changes
- MRI:
-
Magnetic resonance imaging
- ODI:
-
Oswestry Disability Index
- RMDQ:
-
Roland Morris Disability Questionnaire
- SD:
-
Standard deviation
- SPORT:
-
Spine Patient Outcomes Research Trial
- SPSS:
-
Statistical Package for Social Sciences
- VAS:
-
Visual analogue scale
- WHO:
-
World Health Organization
References
Kelsey JL, White AA (1980) Epidemiology and impact of low-back pain. Spine 5(2):133–142
Deyo RA (1991) Nonsurgical care of low back pain. Neurosurg Clin N Am 2(4):851–862
Asch HL, Lewis PJ, Moreland DB et al (2002) Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg 96(1 Suppl):34–44
Mohanlal P, Pal D, Timothy J (2006) Localisation of spinal level in lumbar microdiscectomy. Eur J Orthop Surg Traumatol 16:207. https://doi.org/10.1007/s00590-005-0059-7
Boscainos PJ, Sapkas G, Stilianessi E, Prouskas K, Papadakis SA (2003) Greek versions of the Oswestry and Roland-Morris disability questionnaires. Clin Orthop Relat Res Number 411:40–53. https://doi.org/10.1097/01.blo.0000068361.47147.79
Deyo R, Loeser J, Bigos S (1990) Herniated lumbar intervertebral disc. Αnn Intern Med 112:598
Ahmadi SA, Burkert IP, Steiger HJ et al (2018) Multidimensional long-term outcome analysis after single-level lumbar microdiscectomy: a retrospective single-centre study. Eur J Orthop Surg Traumatol 28:189. https://doi.org/10.1007/s00590-017-2043-4
Lurie J, Tosteson T, Tosteson A et al (2014) Surgical versus non-operative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial (SPORT). Spine 39(1):3–16. https://doi.org/10.1097/BRS.0000000000000088
McGirt MJ, Eustacchio S, Varga P et al (2009) A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy. Factors associated with recurrent disc herniation and disc height loss. Spine 34(19):2044–2051. https://doi.org/10.1097/BRS.0b013e3181b34a9a
Thomé C, Barth M, Scharf J, Schmiedek P (2005) Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine 2(3):271–278. https://doi.org/10.3171/spi.2005.2.3.0271
Carragee EJ, Spinnickie AO, Alamin TF, Paragioudakis S (2006) A prospective controlled study of limited versus subtotal posterior discectomy: short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine 31(6):653–657. https://doi.org/10.1097/01.brs.0000203714.76250.68
Gelalis ID, Papanastasiou EI, Theodorou DJ et al (2018) Postoperative MRI findings 5 years after lumbar microdiscectomy. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-018-2338-0
Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K (2001) Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine 26(6):652–657
Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G (1999) Seven- to 20-year outcome of lumbar discectomy. Spine 24(22):2313
Barth M, Weiss C, Thomé C (2008) Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy: part 1: evaluation of clinical outcome. Spine 33(3):265–272. https://doi.org/10.1097/BRS.0b013e318162018c
Dora C, Schmid MR, Elfering A, Zanetti M, Hodler J, Boos N (2005) Lumbar disk herniation: do MR imaging findings predict recurrence after surgical discectomy? Radiology 235(2):562–567. https://doi.org/10.1148/radiol.2352040624
McGirt MJ, Ambrossi GL, Datoo G, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZLBA (2009) Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery 64(2):338–344. https://doi.org/10.1227/01.NEU.0000337574.58662.E2
Swartz KR, Trost GR (2003) Recurrent lumbar disc herniation. Neurosurg Focus 15(3):E10
Weber H (1983) Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine 8(2):131–140
Dalgic A, Yildirim AE, Okay O et al (2015) Initial discectomy associated with aging lead to adjacent disc disease and recurrence. Turk Neurosurg 26(4):595–600. https://doi.org/10.5137/1019-5149.JTN.13206-14.0
Ganzer D, Giese K, Hunfeld T et al (2002) Lumbar microdiscectomy with and without prophylaxis of perineural scar formation using ADCON-L barrier gel: 2-year results. Eur J Orthop Surg Traumatol 12:1. https://doi.org/10.1007/s00590-002-0011-z
Li T, Han D, Liu B et al (2014) Clinical assessment of reformed lumbar microdiscectomy. Eur J Orthop Surg Traumatol 24:23. https://doi.org/10.1007/s00590-012-1123-8
Cinotti G, Roysam GS, Eisenstein SM, Postacchini F (1998) Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br 80(5):825–832
Guo JJ, Yang H, Tang T (2009) Long-term outcomes of the revision open lumbar discectomy by fenestration: a follow-up study of more than 10 years. Int Orthop 33(5):1341–1345. https://doi.org/10.1007/s00264-008-0648-2
Atlas SJ, Keller RB, Chang Y et al (2001) Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the maine lumbar spine study. Spine 26:1179–1187
Koerner JD, Glaser J, Radcliff K (2015) Which variables are associated with patient-reported outcomes after discectomy? review of SPORT disc herniation studies. Clin Orthop Relat Res 473(6):2000–2006. https://doi.org/10.1007/s11999-014-3671-1
Huang W, Han Z, Liu J, Yu L, Yu X (2016) Risk factors for recurrent lumbar disc herniation. A systematic review and meta-analysis. Medicine 95(2):e2378. https://doi.org/10.1097/MD.0000000000002378
Akmal M, Kesani A, Anand B, Singh A, Wiseman M, Goodship A (2004) Effect of nicotine on spinal disc cells: a cellular mechanism for disc degeneration. Spine 29:568–575. https://doi.org/10.1097/01.BRS.0000101422.36419.D8
Schmidt H, Kettler A, Heuer F et al (2007) Intradiscal pressure, shear strain, and fiber strain in the intervertebral disc under combined loading. Spine 32:748–755. https://doi.org/10.1097/01.brs.0000259059.90430.c2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Ioannis D Gelalis, Evangelos I Papanastasiou, Emilios E Pakos, Avraam Ploumis, Dimitrios V Papadopoulos, Maria Mantzari, Ioannis S. Gkiatas, Marios D. Vekris and Anastasios V. Korompilias declare that they do not have any conflict of interest.
Rights and permissions
About this article
Cite this article
Gelalis, I.D., Papanastasiou, E.I., Pakos, E.E. et al. Clinical outcomes after lumbar spine microdiscectomy: a 5-year follow-up prospective study in 100 patients. Eur J Orthop Surg Traumatol 29, 321–327 (2019). https://doi.org/10.1007/s00590-018-2359-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2359-8