Abstract
Purpose
To investigate whether obesity is associated with worse patient-reported outcomes following surgery for degenerative lumbar conditions.
Methods
We evaluated consecutive patients undergoing elective lumbar laminectomy or laminectomy with fusion for degenerative lumbar conditions. The Oswestry Disability Index (ODI), EuroQol-5D (EQ-5D), Short-Form 12 (SF-12), and NASS patient satisfaction were utilized. Chi-square tests and student t test assessed the association of obesity with PROs. Multivariate regression controlled for age, sex, smoking status, anxiety, depression, revision, preoperative narcotic use, payer status, and diabetes.
Results
A total of 602 patients were included. All PROs improved significantly in both groups. BMI ≥35 was associated with increased ODI at baseline (50.6 vs. 47.2 %, p = 0.012) and 12 months (30.5 vs. 25.7 %, p = 0.005). There was no difference in ODI change scores (21.2 vs. 19.4 %, p = 0.32). With multivariate analysis, BMI ≥35 was not predictive of worse ODI at 12 months (correlation coefficient 1.23, 95 % CI −0.225 to 2.676.) There was no significant difference between groups in percentage of patients achieving the minimum clinically important difference for ODI (59.6 vs. 64 %, p = 0.46) or patient satisfaction (80.5 vs. 78.9 %, p = 0.63).
Conclusions
Body mass index ≥35 is associated with worse baseline and 12-month PROs, however, there was no difference in change scores across BMI groups. Controlling for important co-variables, BMI greater than 35 was not an independent predictor of worse PROs at 12 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2002 there were 315 million people worldwide classified as obese by the World Health Organization [1]. As of 2012, 34.9 % of adults in the United States were reported to be obese [2]. Obesity is associated with disk degeneration, low back pain, and increased incidence of neurologic symptoms with concurrent lumbar disease [3–5]. Obesity is also thought to exacerbate lumbar spine disease, however, its specific impact on validated patient-reported outcomes (PROs) following lumbar surgery remains controversial [6–13]. Previous studies consist of small retrospective cohorts [10, 14] and short-term analyses utilizing administrative databases [8, 15]. A high quality post hoc analysis was performed utilizing data from the Spine Patient Outcomes Research Trial (SPORT) [16] that showed the potentially negative impact of obesity on outcomes [7, 17, 18]. However, there remains a paucity of information on the precise long-term impact of obesity on patient-reported outcome following elective surgery for degenerative lumbar conditions.
The purpose of this study was to investigate the impact of obesity on patient-reported outcomes following elective degenerative lumbar spine surgery using a prospective longitudinal registry at a high-volume academic center. We hypothesized that obesity would have no impact on PROs after surgery for degenerative lumbar conditions when controlling for clinically relevant co-variables.
Methods
Patients
A prospective longitudinal spine registry database was used to evaluate consecutive patients undergoing elective lumbar laminectomy or laminectomy with fusion for spinal stenosis, disk herniation, or spondylolisthesis from October 2010 to November 2014 at a single academic institution. Enrollment into this registry received institutional review board exemption. The overall follow-up rates for the outcomes registry at our institution is 86 % at 3 months and 78 % at 12 months. Inclusion criteria for the present analysis were: age 18 years or greater, failure of 3 months of conservative care or progressive neurological deficit, history and physical exam with correlative imaging, and a minimum follow-up of 12 months. Exclusion criteria were cases of trauma, tumor, infection, urgent/emergent surgery, deformity, and pseudarthrosis. We did not include patients undergoing an anterior lumbar fusion or microdiskectomy procedures (Table 1).
Patient-reported measures
PROs were collected in person or by telephone interview at baseline and at 3 and 12-month postoperatively. The Oswestry Disability Index (ODI, version 2.1a), Short-Form 12 (SF-12) physical and mental component scales (PCS and MCS), EuroQol-5D (EQ-5D), Numerical Rating Scale for pain (NRS), Zung Depression Scale (ZDS), and Modified Somatic Perception Questionnaire (MSPQ) measures were utilized. Each of these PRO measurement tools is validated and widely used in the spine literature [19–29]. In addition we utilized the NASS patient satisfaction scale to compare the rate of patient satisfaction between groups. This scale is scored 1 through 4 with 1 indicating the surgery met the patient’s expectations, 2 indicating improvement was less than desired, but the patient would still undergo the same procedure for the same result, 3 indicating some improvement, but dissatisfaction with the result and unwillingness to undergo the same procedure for the same result, and 4 indicating the patient feels their condition is the same or worse than prior to surgery [30]. Patient who scored a 1 or 2 on this scale were considered to have achieved the minimum clinically important difference in satisfaction.
Minimum clinically important difference (MCID) values used were: ODI 14.9 percentage points, BP 2.1 points, leg pain 2.8 points, and EQ-5D 0.46. These particular values for MCID were calculated by Parker et al. [21] in patients undergoing lumbar fusion procedures; we chose these MCID values because the majority (70 % or more) of patients in this study underwent a fusion procedure. Patients were defined as “obese” for BMI greater than or equal to 35 based on the World Health Organization (WHO) definition of class II obesity [31].
Statistical analysis
Descriptive statistics were used to examine mean scores, standard deviations, and frequency of demographic and clinical characteristics of the study population. Chi-square tests and student t test assessed the association of obesity with disability, as well as percent achieving MCID for ODI and satisfaction at 12 months. Multivariable step-wise linear regression analysis was performed with 12-month ODI scores as the outcome variable. The variables included in the analysis were age, sex, smoking status, preoperative narcotic use, preoperative unemployed, depression, anxiety, history of diabetes, revision surgery, duration of symptoms, presence or absence of neurogenic claudication, number of levels involved and arthrodesis performed. A subgroup analysis was also performed on patients with a BMI ≥40. A p value of 0.05 was considered statistically significant.
Results
Prospective registry data were available for 1868 patients undergoing lumbar procedures during the study period. Of these, 602 patients met the inclusion criteria and were therefore analyzed (Table 1). There was no significant difference in type of procedure performed in the obese versus non-obese groups, with 29 % of obese and 26 % of non-obese undergoing laminectomy alone, and 71 and 74 % undergoing laminectomy plus fusion. Six percent of the non-obese underwent non-instrumented fusion, none of the obese group had a non-instrumented fusion (Table 1).
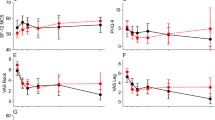
All PROs improved significantly over 12 months in both BMI groups (Fig. 1, Table 2). With univariate analysis, BMI ≥35 was associated with increased ODI at baseline (50.6 vs. 47.2 %, p = 0.01) and 12 months (30.6 vs. 25.6 %, p < 0.01). Obesity was also associated with worse EQ-5D, SF-12 PCS, and SF-12 MCS at baseline. At 12 months, obesity was associated with lower SF-12 PCS, and there was no difference seen in EQ-5D (Table 3). There was no difference in pre- to post-operative change scores in ODI (21.2 vs. 19.4, p = 0.32) (Table 4). These improvements in ODI exceeded the threshold for MCID (14.9 %) and substantial clinical benefit (18.8 %) for lumbar fusion [21, 32]. In addition, there was no significant difference in percentage of patients achieving minimum clinically important difference in ODI (59.6 vs. 64 %), NASS satisfaction score of 2 or better (78.9 vs. 80.5 %), and both leg and back pain scores (Table 4). There was no difference in rate of 90-day complications or 90-day readmission between BMI groups (Table 4). With multivariate analysis, BMI ≥35 was not predictive of worse disability at 12 months as measured by ODI (correlation coefficient 1.23, 95 % confidence interval −0.225 to 2.676) (Table 5). In a subgroup analysis with groups separated into BMI <25, 25–30, 30–40, and over 40, there were no significant differences in ODI change scores between all BMI groups (22.8, 21.75, 20.11, 21.61 %, respectively, p = 0.6). Additionally there were no differences in change scores in EQ-5D, SF-12 PCS, and SF-12 MCS across WHO BMI categories (Table 6).
Discussion
In this study we utilized prospective registry data to investigate the association between obesity and patient-reported outcomes following lumbar surgery for degenerative conditions, while controlling for important co-variables. BMI ≥35 was associated with worse absolute scores in PROs and disability both at baseline and at 12-month postoperatively; however, there was no difference in change scores for PROs between BMI groups. Importantly, there was also no difference in percentage of patients achieving MCID and satisfaction at 1 year. In addition, no difference in 90-day complications or 90-day readmission was observed. These findings suggest that obese patients may achieve equally meaningful improvement in PROs compared to non-obese patients.
Previous studies have presented varying results regarding the impact of obesity on patient-reported outcomes in lumbar surgery. A study from the Swedish Spine Registry reported that higher BMI was associated with greater dissatisfaction and inferior results on ODI and EQ-5D postoperatively in patients undergoing surgery for lumbar stenosis [6]. While absolute scores were lower, there was no direct comparison of change scores in this study, thus their findings show the negative impact of obesity on absolute PROs, but do not show how BMI directly affects surgical outcomes. Similar to the findings of the present study, Djurasovic et al. reported no significant difference in PRO improvement based on BMI in patients undergoing lumbar fusion [13]. Rihn et al. analyzed data from the Spine Patient Outcomes Research Trial (SPORT) [16] and showed that BMI ≥30 was associated with less treatment effect on PROs for those undergoing surgery for disk herniation [7]. In a separate review of spinal stenosis (SpS) and degenerative spondylolisthesis (DS) patients, Rihn et al. demonstrated that a BMI ≥30 was not associated with less improvement in PROs following surgery for these conditions [17]. Reinforcing these findings, another subgroup analysis of the SPORT data showed that BMI ≥35 did not impact the treatment effect of surgery for SpS and DS; while inferior change scores were seen in those with a BMI ≥35 undergoing surgery for disk herniation [18].
The findings presented here support the hypothesis that obesity is not associated with a lesser treatment effect following surgery for degenerative lumbar conditions. To our knowledge this is the first large scale study to utilize in-depth prospective registry data to analyze the association between obesity and the treatment effect of surgery for degenerative lumbar conditions while controlling for confounding variables. Additionally, in this analysis we found significant associations between poor PROs and the following patient characteristics: Anxiety, unemployment, depression, revision surgery, and diabetes (Table 5). These findings have also been reported elsewhere in the literature [33–35]. The strength of this study is the in-depth nature of our institution’s registry data that allowed us to carefully control for those variables that are known to have an impact on outcomes in spine: narcotic use, smoking status, payer status, depression and anxiety, diabetes, and revision surgery [34–38]. Additionally, our study is unique in the relatively high number of patients with BMI ≥35 surgically treated at a single institution. There is little dispute that obesity adds complexity to surgical care; and our findings suggest that obese patients can achieve an equally meaningful improvement in surgical outcomes when cared for at a high-volume center that is equipped to manage additional complexity.
This study is not without its limitations. The PROs reported here were obtained 12 months following surgery. Certainly longer term follow-up is needed to characterize the impact of obesity on durability. However, numerous studies have revealed that the majority of patients undergoing spine surgery achieve maximal improvement by 3–6 months; thus the benefit of surgery is likely to be realized at the 12 month follow-up [39–41]. Another potential limitation is the combining of patients undergoing decompression only with those undergoing a fusion procedure. The MCID used in our study was one calculated for patients undergoing lumbar fusions; therefore, this MCID would be overly stringent on patients undergoing less invasive procedures (i.e., decompression only) and therefore underestimate the benefit to those patients. The finding that these patients achieved MCID despite the use of this more rigorous threshold may add confidence that clinically meaningful benefit was attained. Future studies are needed to better characterize the contribution of obesity to outcomes for specific diagnoses and procedures.
Conclusion
In this analysis of prospective data from patients undergoing elective lumbar surgery, BMI ≥ 35 is associated with worse baseline and 12-month PROs, however, no differences in PRO change scores were observed across BMI groups. Additionally, no difference in 90-day complications was seen between groups. After controlling for clinically important covariates, BMI ≥35 was not an independent predictor of worse PROs at 12 months. Obese patients may therefore achieve meaningful improvement following surgery for degenerative lumbar conditions.
References
Caterson ID, Gill TP (2002) Obesity: epidemiology and possible prevention. Best Pract Res Clin Endocrinol Metab 16(4):595–610
Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8):806–814. doi:10.1001/jama.2014.732
Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L (2008) The impact of obesity on the musculoskeletal system. Int J Obes (2005) 32(2):211–222. doi:10.1038/sj.ijo.0803715
Fanuele JC, Abdu WA, Hanscom B, Weinstein JN (2002) Association between obesity and functional status in patients with spine disease. Spine (Phila Pa 1976) 27(3):306–312
Hangai M, Kaneoka K, Kuno S, Hinotsu S, Sakane M, Mamizuka N, Sakai S, Ochiai N (2008) Factors associated with lumbar intervertebral disc degeneration in the elderly. Spine J 8(5):732–740. doi:10.1016/j.spinee.2007.07.392
Knutsson B, Michaelsson K, Sanden B (2013) Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 38(5):435–441. doi:10.1097/BRS.0b013e318270b243
Rihn JA, Kurd M, Hilibrand AS, Lurie J, Zhao W, Albert T, Weinstein J (2013) The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 95(1):1–8. doi:10.2106/jbjs.k.01558
Seicean A, Alan N, Seicean S, Worwag M, Neuhauser D, Benzel EC, Weil RJ (2014) Impact of increased body mass index on outcomes of elective spinal surgery. Spine (Phila Pa 1976) 39(18):1520–1530. doi:10.1097/brs.0000000000000435
Hanigan WC, Elwood PW, Henderson JP, Lister JR (1987) Surgical results in obese patients with sciatica. Neurosurgery 20(6):896–899
Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A (2009) Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 34(5):495–500. doi:10.1097/BRS.0b013e318198c5f2
Peng CW, Bendo JA, Goldstein JA, Nalbandian MM (2009) Perioperative outcomes of anterior lumbar surgery in obese versus non-obese patients. Spine J 9(9):715–720. doi:10.1016/j.spinee.2009.04.023
Koerner JD, Glaser J, Radcliff K (2014) Which variables are associated with patient-reported outcomes after discectomy?. Clin Orthop Relat Res, Rev SPORT Disc Herniation Studies. doi:10.1007/s11999-014-3671-1
Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY (2008) The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976) 33(16):1789–1792. doi:10.1097/BRS.0b013e31817b8f6f
Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG (2008) Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery 63(5):956–960. doi:10.1227/01.neu.0000313626.23194.3f (discussion 960)
Buerba RA, Fu MC, Gruskay JA, Long WD 3rd, Grauer JN (2014) Obese class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J 14(9):2008–2018. doi:10.1016/j.spinee.2013.11.047
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 296(20):2441–2450. doi:10.1001/jama.296.20.2441
Rihn JA, Radcliff K, Hilibrand AS, Anderson DT, Zhao W, Lurie J, Vaccaro AR, Freedman MK, Albert TJ, Weinstein JN (2012) Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 37(23):1933–1946. doi:10.1097/BRS.0b013e31825e21b2
McGuire KJ, Khaleel MA, Rihn JA, Lurie JD, Zhao W, Weinstein JN (2014) The effect of high obesity on outcomes of treatment for lumbar spinal conditions: subgroup analysis of the spine patient outcomes research trial. Spine (Phila Pa 1976) 39(23):1975–1980. doi:10.1097/brs.0000000000000577
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25(22):2940–2952 (discussion 2952)
Davidson M, Keating JL (2002) A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther 82(1):8–24
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604. doi:10.3171/2010.12.spine10472
Glassman SD, Copay AG, Berven SH, Polly DW, Subach BR, Carreon LY (2008) Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am 90(9):1839–1847. doi:10.2106/jbjs.g.01095
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Luo X, George ML, Kakouras I, Edwards CL, Pietrobon R, Richardson W, Hey L (2003) Reliability, validity, and responsiveness of the short form 12-item survey (SF-12) in patients with back pain. Spine (Phila Pa 1976) 28(15):1739–1745. doi:10.1097/01.brs.0000083169.58671.96
Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J (1997) A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med 19(2):179–186
McCormick JD, Werner BC, Shimer AL (2013) Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg 21(2):99–107. doi:10.5435/jaaos-21-02-99
Guilfoyle MR, Seeley H, Laing RJ (2009) The short form 36 health survey in spine disease—validation against condition-specific measures. Br J Neurosurg 23(4):401–405. doi:10.1080/02688690902730731
Solberg TK, Olsen JA, Ingebrigtsen T, Hofoss D, Nygaard OP (2005) Health-related quality of life assessment by the EuroQol-5D can provide cost-utility data in the field of low-back surgery. Eur Spine J 14(10):1000–1007. doi:10.1007/s00586-005-0898-2
Jansson KA, Nemeth G, Granath F, Jonsson B, Blomqvist P (2009) Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Joint Surg Br 91(2):210–216. doi:10.1302/0301-620x.91b2.21119
Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23(18):2003–2013 (Phila Pa 1976)
WHO | Obesity and overweight (2015) World Health Organization. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 18 Dec 2015
Glassman SD, Copay AG, Berven SH, Polly DW, Subach BR, Carreon LY (2008) Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am 90(9):1839–1847. doi:10.2106/jbjs.g.01095 (United States)
Sinikallio S, Aalto T, Airaksinen O, Lehto SM, Kroger H, Viinamaki H (2011) Depression is associated with a poorer outcome of lumbar spinal stenosis surgery: a two-year prospective follow-up study. Spine 36(8):677–682. doi:10.1097/BRS.0b013e3181dcaf4a (Phila Pa 1976)
Schade V, Semmer N, Main CJ, Hora J, Boos N (1999) The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain 80(1–2):239–249
Browne JA, Cook C, Pietrobon R, Bethel MA, Richardson WJ (2007) Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976) 32(20):2214–2219. doi:10.1097/BRS.0b013e31814b1bc0 (United States)
Lee D, Armaghani S, Archer KR, Bible J, Shau D, Kay H, Zhang C, McGirt MJ, Devin C (2014) Preoperative opioid use as a predictor of adverse postoperative self-reported outcomes in patients undergoing spine surgery. J Bone Joint Surg Am 96(11):e89. doi:10.2106/jbjs.m.00865
Andersen T, Christensen FB, Laursen M, Hoy K, Hansen ES, Bunger C (2001) Smoking as a predictor of negative outcome in lumbar spinal fusion. Spine (Phila Pa 1976) 26(23):2623–2628
Sinikallio S, Aalto T, Airaksinen O, Herno A, Kroger H, Savolainen S, Turunen V, Viinamaki H (2007) Depression is associated with poorer outcome of lumbar spinal stenosis surgery. Eur Spine J 16(7):905–912. doi:10.1007/s00586-007-0349-3
Malmivaara A, Slatis P, Heliovaara M, Sainio P, Kinnunen H, Kankare J, Dalin-Hirvonen N, Seitsalo S, Herno A, Kortekangas P, Niinimaki T, Ronty H, Tallroth K, Turunen V, Knekt P, Harkanen T, Hurri H (2007) Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine (Phila Pa 1976) 32(1):1–8. doi:10.1097/01.brs.0000251014.81875.6d
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, Birkmeyer NJ, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356(22):2257–2270. doi:10.1056/NEJMoa070302
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358(8):794–810. doi:10.1056/NEJMoa0707136
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding sources were utilized for this project.
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Sielatycki, J.A., Chotai, S., Stonko, D. et al. Is obesity associated with worse patient-reported outcomes following lumbar surgery for degenerative conditions?. Eur Spine J 25, 1627–1633 (2016). https://doi.org/10.1007/s00586-016-4460-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4460-1