Abstract
The objective of this study is to describe a series of cranio-cervical dissociation victims and evaluate their outcomes as well as discuss the clinical dilemmas we faced in the context of current literature evidence. This is a retrospective cohort study of traumatic occipito-cervical dissociation in five patients (three males and two females) encountered between 2010 and 2016 at a tertiary care facility in the Middle East region. All patients underwent occipito-cervical fusion using screws and rods system with mean postoperative follow-up period of 2.5 years. All patients survived, and four were independently mobile and one wheel chair bound. Most had some degree of neurological sequelae, often due to associated injuries and all complained of limited neck range of motion. Contemporary literature review shows that CT scan with MRI is often the best diagnostic modality. Surgery is usually indicated though rare cases treated conservatively have been reported. The commonest predictor of mortality is missed injury, associated head injury and wide separation between the skull base and C1 on imaging studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic occipito-cervical dislocation (OCD), atlanto-occipital dislocation (AOD) and cranio-cervical dissociation (CCD) all describe a catastrophic traumatic injury of the ligaments binding the base of the skull to the upper cervical spine. These lesions are typically due to high-velocity accidents in particular motor vehicle injuries. Blackwood [18] is credited with the first published report of this injury in 1908. Most of the series that have followed in subsequent decades consists of small numbers of patients and report high mortality rates. The literature from 1966 to 2001 has reported only 135 survivors globally [15]. Survivorship has progressively improved over the years, and Meuller reported 60% mortality in 2013 [23]. In the last 110 years or so, the near 100% mortality for this injury has been substantially reduced to almost 100% survival (in at least few reports by Blellbarba and Ben Ghalim) [1, 2]. This reduction in mortality has been attributed to the improving trauma salvage services, enhanced imaging protocols leading to the early detection of these injuries, the high index of clinical suspicion entertained by the trauma team and the newer surgical strategies for managing these complex injuries [18]. Additionally, it must also be recognized that the exact criteria for diagnosis as well as the timing of diagnosis also might be different in the various series.
The present work is a case series of all the patients treated in a level 1 trauma center in the Middle East, from 2010 to 2016. The five cases detected and treated once they arrived at the hospital; all survived with varying degrees of residual neurological impairments.
Materials and methods
This is a retrospective observational study based on the documents retrieved from the electronic database maintained at a tertiary care and level 1 trauma center in the Sultanate of Oman. All patients admitted with OCD with the orthopedic, neurosurgical and general surgical services were retrieved. The electronic hospital information system was also analyzed to identify occipito-cervical fusion surgeries for any reason to identify potential traumatic CCD cases. The CT scans were individually reviewed by the senior author to confirm the diagnosis. The demographic features of all the cases are presented in Table 1. Radiological parameters are recorded in Table 2. Four patients were followed up from the time of discharge to a minimum 12 months, and their neurological status documented at the last visit. One patient who was an expatriate in Oman had stayed on as in-patient for over 12 months for neuro-rehabilitation and was lost to follow-up after discharge. No statistical tools were employed since the numbers studied were small. The institutional review board does not mandate ethics committee approval since the study is retrospective, informed consent obtained and the data de-identified.
Results
All the five cases we received were road traffic accidents. There were two women and three men in this cohort aged between 23 and 33. There were no children in our series. All patients had thin slice CT scans, but only one had an MRI scans as well. OCD without fracture was diagnosed in four, and condyle fracture with OCD was diagnosed in one. One patient had an additional C1 fracture (Fig. 1). Three patients had associated chest and abdominal injuries, three had limb injuries, and three had pelvic injuries. There were three patients with head injuries with GCS ranging from 3 to 5 on admission. All the patients underwent occiput to C3 instrumented fusion through the posterior approach except case number 3 who had C0–C4 fusion (Fig. 2). The mean timing to surgery was 2.5 days from admission, mean hospitalization duration was 115 days, and ICU stay was 16 days. All the cases were operated by the senior author, and the axon occipito-cervical stabilization system (DePuy-Synthes, CA, USA) was the instrumentation used.
The median follow-up was 2.5 years, and all patients were followed up for this period save case number 2 who was a foreign national and had to be repatriated back to his home country after 12-month hospitalization in the neuro-rehabilitation service. At 12-month review, four of the five cases were ambulant independently without support but complained of limited neck movements (Table 2). Two patients had foot drop (both had associated complex pelvic fractures), while one each had slurred speech and weak hand grip. The patient with the GCS of 3 on admission was severely spastic upon 1-year review and was in a wheel chair though he could stand with support. One case also complained of urinary dysfunction.
Discussion
Evidently, there has been a significant reduction in the mortality of traumatic CCD injuries from the turn of the last century when it was first reported to the last decade [1]. Early diagnosis, advanced emergency management, meticulous and safe transport of the victim, modern imaging techniques like pan CT, aggressive trauma care for other systemic injuries have enhanced patient survival [1, 17]. Additionally, the techniques and implants for surgical stabilization of the occipito-cervical junction have improved tremendously in the last few decades [10, 16]. Nonetheless, it must be remembered that the latter series are all hospitalized patients, and clearly, only a small percentage of these injuries would actually survive to reach the hospital. Cooper et al.’s report [7] from a level 1 trauma center in the USA suggests that 47 out of 69 cases were diagnosed postmortem and of the 22 diagnosed in hospital only seven survived to discharge [7]. Bucholz and Burkhead [5] have reported that vast majority of the injuries occur in children, but their data seem to be derived from fatal CCD injuries. In our cohort, which was based on hospital data, there were no children involved.
In the clinical setting, when encountered with a suspected case of CCD there are several dilemmas that confront the physician.
-
1.
How to immobilize the cervico-cranium in the presence of head injury?
-
2.
How useful is the trauma series X-rays in detecting this injury? What CT criteria are best to confirm the diagnosis?
-
3.
How useful is MRI? Is it mandatory?
-
4.
Is angiogram useful and necessary?
-
5.
Is stress testing useful and recommended?
-
6.
How to decide on management strategy? Is it necessary to classify these lesions? Is there a role for conservative care?
-
7.
How quickly should the surgery be performed?
-
8.
What is the optimal distal fusion level? Can the implant be removed subsequently?
-
9.
What is the outcome? How to prognosticate survival?
Needless to say, OCD injuries are rare and establishing institutional guidelines for care based on personal experience therefore, difficult. Synthesizing evidence is also difficult since most publications on the subject have small numbers of patients and no form of randomization is possible in this potentially fatal injury. Given these limitations, the authors reviewed the current literature to try and best answer these questions so that we can establish clear strategies for the management of these complex injuries.
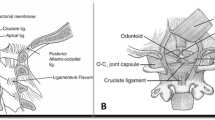
Plain X-rays are notoriously inadequate in diagnosing cranio-cervical injuries [18]. CT scans are the imaging modality of choice [5, 12, 20, 27, 28]. There is no consensus on what diagnostic criteria are best on CT scans. Different authors have reported different results in their respective series [12, 21, 28]. Dahdaleh et al. [8] studied the various radiological measures on CT scan and concluded that the modified condyle-C1 interval (CCI) was the most sensitive and reliable diagnostic parameter. This author’s work has suggested that the revised CCI (> 2.5 mm) and condylar sum (> 5 mm) might be more sensitive than the CCI measurement alone on CT (Fig. 3). Ravindra et al. [27], Bertozzi et al. [3] and Martinez-Del-Campo et al. [20] have also reaffirmed these observations in pediatric and adult patient populations, respectively. Martinez-Del-Campo and colleagues compared normal with injured cranio-cervical junctions and reported that among the various craniometric parameters studied CCI (1.5 mm) and condylar sum (3 mm) had the best sensitivity and specificity for these injuries [20]. Clearly, these parameters have different values in adults compared to children [11, 17]. Roy et al.’s [29] study demonstrated that none of the conventional craniometric measures on CT (ADI, AOI, BDI and Power’s ratio) (Figs. 4, 5) were absolutely fool proof in diagnosing these lesions though ADI appeared the most consistent. Meuller et al. [23] an associates discuss the relevance of radiological parameters to guide mortality and conclude that a BDI of > 16 mm is not compatible with life though the current consensus is that measurements on static images poorly reflect the dynamic nature of the instability and does not correlate with mortality [1].
Given that the displacements observed on CT scan are temporal and position dependent, it seems logical that diagnosing ligament injuries is the real key to identifying these potentially fatal injuries [5], hence the relevance of MRI scanning in suspected CCD injuries. MRI has the advantage of delineating the integrity of the ligaments injured as well as the status of the spinal cord. Roy et al. [29] and Nidecker and Shen [24] have recommended MRI scans as diagnostic. Radcliff et al. [25], in a clinical series of 18 cases, have demonstrated that the atlanto-occipital capsule injury can be identified on MRI and its injury is to be considered as critical to the stability of the CV junction. The cruciate ligaments appear less critical according to these authors. However, the same authors, based on a cadaveric study, have suggested that the transverse and alar ligaments are more critical that the capsule of the atlanto-occipital joint [26]. Debernardi et al. [9] have recommended the usage of an MR-based scoring system to determine instability and decide on surgical fusion. Roy et al. [29] also suggest that the rule of Spence intended to diagnose transverse ligament injury is often inadequate for this purpose and that MRI appeared to be the best tool to diagnose ligament injuries in this location. Needless to say MRI has been increasingly used for cranio-cervical trauma in recent years, and the optimal criteria for the diagnosis of CCD lesions are yet to evolve. Vilela et al.’s [31] study has recorded up to 50% vascular lesions picked up on angiographic studies in CCD lesions, and they recommend both MRI and angiograms in all cases.
Like the subaxial cervical spine injuries, it might seem tempting to suggest stress imaging (traction or flexion/extension images) to diagnose ongoing instability. Child et al. [6], in his study on cadaveric specimens, have demonstrated that instability manifests as 2-mm distraction can be attained by traction utilizing as less as 5–10 lbs. weight. Nonetheless, given the high morbidity and mortality of these lesions as well as the ethical issues concerning such testing in the clinical scenario, it is at best recommended in very selected situations.
Once instability has been diagnosed in a case of CCD, it would appear rational to surgically stabilize the injury [1, 18]. Nevertheless, there is a role for conservative management in selected cases. Kaplan reported excellent outcomes with conservative treatment in one patient; these authors also pointed out that current literature review demonstrates uniformly poor outcomes for such management [17]. They treated their patient in a halo vest for 6 months. Kato et al. [19] also recommend long-term halo vest immobilization and postural adjustments in the halo to maintain reduction. Halo cervical immobilization has also been reported to have successful results in children, but in adults the uniform recommendation is surgery [11]. The current role of non-operative treatment seems optimal for MRI-positive but CT-negative cases of OCD based on the experience of Horn et al. [16] with 33 patients. Vacarro et al. [30] have summarized the indications for surgical treatment based on classification systems (he and coauthors use the Anderson and Montesano schema for occipital condyle fractures and recommends fusion for type III lesions). Brotis et al. [4] have not found such approach evidence-based because they have reported 20 classifications for injuries in the cranio-vertebral junction region with 72 individual injury patterns and only two of these have been independently validated.
Cranio-cervical disjunction is routinely stabilized through the posterior approach. The extent of instrumentation depends on the associated injuries. Typically, C0–C2 is the fusion level, but this may need further downward extension based on other cervical injuries. The authors have chosen C3 instead of C2 because purchase in a single distal segment was perceived to be inadequate in all the cases in this series. Goel has described an alternate anterior approach to instrument from the clivus to the C2 vertebra, but this technique has not been uniformly popular [13]. Grob [14] has published an elegant technique of trans-articular screw fixation for the cranio-cervical junction. Clearly, the earlier the surgery is performed the better the likely outcome, though there is little evidence to actually substantiate this concept [10, 18].
As described earlier, survival has dramatically improved in many of the CCD injuries (Table 3). All the same Mendenhalls et al.’s [22] study demonstrated 26% mortality in the first 3 months. Their most important predictor of mortality was missed diagnosis. Fard et al. [10] reported that the only important prognostic indicator is associated head injury. Cooper et al. [7] have also added BDI (Basion-Dens interval) > 16 mm as a predictor of near certain mortality. Gregg, Mueller and others [15, 16, 23] have recorded survival but with significant residual neurological disabilities. Mueller et al.’s [23] study is based on the review of 2616 CT scans of the skull and cervical spine in a University Center in Germany. They had five cases (0.2%) of CCD and 31 (1.19%) patients with occipital condyle fractures without subluxation. In the former five, three patients also had a condyle fracture. They treated all their cases with halo immobilization and secondarily were converted to OC fusion. The authors report 60% mortality, all within the first fortnight, and these were attributed to concomitant head injury. These authors also suggest that an initial Glasgow Coma of < 3 is consistent with a fatal outcome in this cohort. Horn et al. [16] also conclude that traumatic brain injury is the common denominator for a fatal outcome in these patients.
With the available literature evidence, a current guideline may be formulated as follows:
-
CCD lesions are best diagnosed with thin slice CT combined with MRI scans. On CT scan, the modified CCI appears to give the most consistent results. Angiograms are recommended in obvious neurological deficits and unconscious patients. Stress testing is not recommended.
-
Once diagnosed, these lesions are best treated surgically by occiput to C2 or C3 stabilization through the posterior approach.
-
Conservative treatment with halo is suitable for children and MRI-positive but CT-negative cases of CCD.
-
Residual neural dysfunction can be anticipated though substantial recovery is often expected.
-
Mortality is usually related to missed lesions and associated head injury as well as wide distraction (> 16 mm) on initial imaging studies.
The emergency management of OCD injuries is beyond the scope of this study. Nevertheless, it is evident that standard extrication collars of the cervical spine do not immobilize the cranio-cervical junction adequately. Emergency intubation, often indicated for gross hemodynamic and ventilatory instability or associated head injury, is clearly best performed under fiberoptic assistance to minimize the manipulation of the neck. Routine cervical spine lateral X-rays do not reveal the catastrophic CCD lesion, and trauma pan CT is mandatory to salvage these patients. Long-term neuro-rehabilitation is often a rule than an exception in most of the studies referred to in Table 3.
References
Bellabarba C, Mirza SK, West GA, Mann FA, Dailey AT, Newell DW, Chapman JR (2006) Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine 4(6):429–440
Ben-Galim PJ, Sibai TA, Hipp JA, Heggeness MH, Reitman CA (2008) Internal decapitation: survival after head to neck dissociation injuries. Spine 33:1744–1749
Bertozzi JC, Rojas CA, Martinez CR (2009) Evaluation of the pediatric craniocervical junction on MDCT. Am J Roentgenol 192:26–31. doi:10.2214/AJR.08.1058
Brotis AG, Paraskevi TM, Tsitsopoulos P et al (2015) An evidence-based approach towards the cranio-cervical junction injury classifications. Eur Spine J 24(5):931–939. doi:10.1007/s00586-015-3877-2
Bucholz RW, Burkhead WZ (1979) The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg Am 61(2):248–250
Child Z, Rau D, Lee MJ, Ching R, Bransford R, Chapman J, Bellabarba C (2016) The provocative radiographic traction test for diagnosing craniocervical dissociation: a cadaveric biomechanical study and reappraisal of the pathogenesis of instability. Spine J 16(9):1116–1123. doi:10.1016/j.spinee.2016.03.057
Cooper Z, Gross JA, Lacey JM et al (2010) Identifying survivors with traumatic craniocervical dissociation: a retrospective study. J Surg Res 160(1):3–8
Dahdaleh NS, Khanna R, Menezes AH et al (2016) The application of the revised condyle-C1 interval method to diagnose traumatic atlanto-occipital dissociation in adults. Glob Spine J 6:529–534
Debernardi A, Sala E, D’Aliberti G et al (2014) Acute traumatic fractures to the craniovertebral junction: preliminary experience with the “MILD” score scale. Eur J Trauma Emerg Surg 40:343. doi:10.1007/s00068-014-0387-6
Fard SA, Avila MJ, Johnstone CM, Patel AS et al (2016) Prognostic factors in traumatic atlanto-occipital dislocation. J Clin Neurosci 33:63–68
Farley FA, Graziano GP, Hensinger RN (1992) Traumatic atlanto-occipital dislocation in a child. Spine 17:1539–1541
Gire JD, Roberto RF, Bobinski M, Klineberg EO, Durbin-Johnson B (2013) The utility and accuracy of computed tomography in the diagnosis of occipitocervical dissociation. Spine J 13(5):510–519. doi:10.1016/j.spinee.2013.01.023
Goel A, Karapurkar AP (1994) Transoral plate and screw fixation of the craniovertebral region—a preliminary report. Br J Neurosurg 8(6):743–745
Grob D (2001) Transarticular screw fixation for atlanto-occipital dislocation. Spine 26:703–707
Gregg S, Kortbeek JB, du Plessis S (2005) Atlanto-occipital dislocation: a case study of survival with partial recovery and review of the literature. J Trauma 58:168–171
Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N (2007) Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine 6(2):113–120
Kaplan NB, Molinari C, Molinari RW (2015) Nonoperative management of craniocervical ligamentous distraction injury: literature review. Glob Spine J 5(6):505–512. doi:10.1055/s-0035-1566290
Kasliwal MK, Fontes RB, Traynelis VC (2016) Occipito-cervical dissociation—incidence, evaluation and treatment. Curr Rev Musculoskelet Med 9:247–254
Kato G, Kawaguchi K, Tsukamoto N et al (2015) Recurrent dislocations of the atlantooccipital and atlantoaxial joints in a halo vest fixator are resolved by backrest elevation in an elevation angle–dependent manner. Spine J 15(10):e69–e74
Martinez-Del-Campo E, Kalb S, Soriano-Baron H et al (2016) Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine 24(4):535–545. doi:10.3171/2015.6.SPINE15226
Maziyar AK, John KR (2013) Considering the diagnosis of occipitocervical dissociation. Spine J 13(5):520–522
Mendenhall SK, Sivaganesan A, Mistry A, Sivasubramaniam P, McGirt MJ, Devin CJ (2015) Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a level 1 trauma center over 15 years. Spine J 15(11):2385–2395
Mueller FJ, Kinner B, Rosskopf M et al (2013) Incidence and outcome of atlanto-occipital dissociation at a level 1 trauma centre: a prospective study of five cases within 5 years. Eur Spine J 22:65. doi:10.1007/s00586-012-2543-1
Nidecker AE, Shen PY (2016) Magnetic resonance imaging of the craniovertebral junction ligaments: normal anatomy and traumatic injury. J Neurol Surg B 77(05):388–395. doi:10.1055/s-0036-1584230
Radcliff K, Kepler C, Reitman C et al (2012) CT and MRI-based diagnosis of craniocervical dislocations: the role of the occipitoatlantal ligament. Clin Orthop Relat Res 470(6):1602–1613
Radcliff KE, Hussain MM, Moldavsky M et al (2015) In vitro biomechanics of the craniocervical junction—a sequential sectioning of its stabilizing structures. Spine J 15(7):1618–1628
Ravindra VM, Riva-Cambrin J, Horn KP et al (2017) A 2D threshold of the condylar-C1 interval to maximize identification of patients at high risk for atlantooccipital dislocation using computed tomography. J Neurosurg Pediatr 19(4):458–463. doi:10.3171/2016.10.PEDS16459
Rojas CA, Bertozzi JC, Martinez CR, Whitlow J (2007) Reassessment of the craniocervical junction: normal values on CT. Am J Neuroradiol 28:1819–1823. doi:10.3174/ajnr.A0660
Roy AK, Miller BA, Holland CM, Fountain AJ, Pradilla G, Ahmad FU (2015) Magnetic resonance imaging of traumatic injury to the craniovertebral junction: a case-based review. Neurosurg Focus 38(4):E3
Vaccaro AR, Lim MR, Lee JY (2005) Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury 36(Suppl 2):B44–B53
Vilela MD, Kim LJ, Bellabarba C, Bransford RJ (2015) Blunt cerebrovascular injuries in association with craniocervical distraction injuries: a retrospective review of consecutive cases. Spine J 15(3):499–505
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
The institutional review board does not mandate an ethics committee approval for this study since it is retrospective, observational, with de-identified patient data and informed consent obtained from all the patients.
Informed consent
Informed consent was obtained from all the patients related to this study.
Rights and permissions
About this article
Cite this article
Menon, K.V., Al Habsi, I. & Al Ghafri, K. Traumatic occipito-cervical dissociation in adults: a Middle Eastern cohort study. Eur J Orthop Surg Traumatol 28, 381–387 (2018). https://doi.org/10.1007/s00590-017-2053-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-017-2053-2