Abstract
Introduction
Hypertrophy of the tensor fascia lata muscle (HTFLM) is a rare complication after total hip arthroplasty (THA) and is a potential source of pain, palpable mass, or both.
Materials and methods
We retrospectively analyzed 1285 primary THAs and 482 THA revisions (THAR) performed at our center from 2008 to 2014. Among these, five patients had HTFLM (average age 68.8 years). The type of surgery and symptoms were evaluated, as were imaging studies (CT or MRI) of both hips (10 hips), and functional outcomes with the Merle d’Aubigné score.
Results
The suspected diagnosis was established at an average of 30.2 months after surgery. Four cases occurred after THA and one case after THAR. A modified Hardinge approach was used in four cases and a Röttinger approach in one case. Two cases had pain and palpable mass in the trochanteric region and three cases only pain. The asymmetric HTFLM of the THA side against the nonsurgical side was confirmed by measuring the cross section of the tensor fascia lata muscle on imaging. The sartorius muscle was measured for reference in each case. The Merle d’Aubigne scale had a mean value of 16.6 (range 13–18) at 38 months after the procedure.
Conclusions
HTFLM after THA is a benign condition that could be mistaken for a tumor when presenting as a palpable mass. We propose that it should be considered in the differential diagnosis of pain in the lateral aspect of hips that have previously undergone THA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The finding of a palpable mass in the lower limbs is common in clinical practice, with differential diagnoses that range from benign lipomas to malignancy [1, 2]. Hypertrophy of the tensor fascia lata muscle (HTFLM) is a rare cause of palpable mass, pain, or both in the hip and thigh. It should be considered in the differential diagnosis of masses at that location.
Muscle hypertrophy can be true of false. True hypertrophy is that secondary to a growth in the number of muscle fibers. In contrast, pseudohypertrophy is typically observed in muscular dystrophies and associated with a concomitant increase in adipose and connective tissue, with fewer muscle fibers [3, 4]. However, no clear etiology has been shown in previous cases of HTFLM. One postulated etiology is that there is an overload in the hip secondary to muscle gait disturbances by THA surgery. Another possibility is that it is secondary to myopathic or neuropathic causes.
In this study, we aimed to determine the incidence of HTFLM after THA surgery in the hip unit of our tertiary hospital. We also wanted to identify possible causes, the treatments performed, and the clinical evolution.
Materials and methods
We performed a retrospective study analyzing the database of the hip unit of our hospital. Data belonging to 1285 primary total hip arthroplasties (THAs) and 482 THA revisions (THAR) performed at our center from January 2008 to January 2014 were included. In total, five patients were identified with a clinical and imaging diagnosis of HTFLM, which is a diagnosis of exclusion in patients with a THA and lateral hip pain. HTFLM usually presents as a slow growing mechanic pain on lateral side of the hip (trochanteric region), with limp and occasionally associated with a local palpable mass, in a patient with a THA (also there are cases without THA) [3] after exclusion of other causes of lateral hip pain such as greater trochanteric pain syndrome(GTPS) (prolonged, intermittent peritrochanteric pain accompanied by tenderness to palpation overlying the lateral aspect of the hip, rarely accompanied by a palpable mass). GTPS commonality includes trochanteritis (lateral hip pain without a palpable mass), infection (painful HTA with symptoms of inflammation including erythema, local heat, edema, and rubor, elevation of ESR and CRP, palpable mass occasionally with fistula), lateral hip snapping (lateral hip pain with snapping sound or clicking evoked by flexion and extension of the hip), and tumors (palpable mass with pain at rest, occasionally fever and other in specific symptoms). Diagnosis of HTFLM is allowed by an integrated clinical and radiological approach (MRI or CT), to exclude other causes described of lateral hip pain, especially on cases with lateral hip pain and without palpable mass.
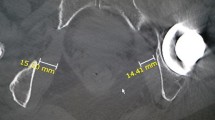
All patients provided written consent for the use of retrospective data for clinical research.
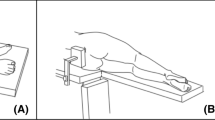
We collected data on the following variables: the type of surgery performed (THA vs. THAR), the surgical approach (Hardinge or Watson–Jones intermuscular mini-invasive, also known as the Röttinger approach), and symptoms that prompted consultation (pain, pseudotumor mass) (Fig. 1). From imaging studies, we recorded the axial height of the muscles at the same level of the femoral necks with either 5-mm interval CT (Somatom 64, Siemens, Erlangen, Germany) or SET1-weighted MRI (1.5 Tesla Symphony, Erlangen, Germany). The images were then analyzed individually by three radiologists, each with more than 15-year experience in the field of musculoskeletal imaging. Different measures were taken for the tensor fascia lata muscles and the sartorius muscles (for comparison) of both hips using a picture archiving and communication system. We measured the maximum length and width in transversal slides and also the areas at the same slice of both diameters. We used the recommendations of Sutter et al. [5] and included measurements of the sartorius at the femoral neck level as an independent reference. This is because the value of isolated muscle area of the tensor fascia lata muscle is insufficient for the diagnosis of HTFLM (Figs. 2, 3, 4). Finally, the functional results were calculated by the Merle d’Aubigné score [6] at the time of diagnosis and at the last follow-up (minimum follow was 6 months).
Results
Five patients were identified with HTFLM: three males and two females with an average age of 68.8 years. Four cases had a primary THA implanted (83.33 %) and one case had a THAR. The modified Hardinge approach was used in four cases and the Röttinger approach in one case. In two cases, the initial symptoms were pain on the lateral aspect of the hip (the trochanteric region) with clinical evidence of a palpable mass. However, three cases presented with pain without a mass. The pain was mild in three cases and moderate in 2 using a visual analog scale. The diagnosis of HTFLM was performed at 30.2 months (range 12–43) after arthroplasty. In all cases, the diagnosis was made by imaging (CT or MRI). The gluteus minimus and medius showed atrophy in all cases on the side of arthroplasty (Table 1).
HTFLM occurred on the same side as the THA in all five patients, with an average tensor fascia lata muscle area of 16.09 cm2 (range 8.42–25.09 cm2). The contralateral, nonsurgical hip had an average area of 7.47 cm2 (range 4.65–11.79 cm2). Moreover, the average areas of the sartorius muscles on the ipsilateral and contralateral sides were both 3.23 cm2 (Tables 2, 3).
Conservative treatment was indicated in all cases and consisted of physiotherapy of the pelvic and trochanteric area, and nonsteroidal anti-inflammatory analgesics on demand. Functional assessment with the Merle d’Aubigné score at diagnosis was 16.6 (range 13–18) and remained unchanged at 7.7 months (range 6.1–8.3) of follow-up.
Discussion
HTFLM is a very rare condition. In the period of this study (2008–2014), we performed 1285 THAs and 482 THAR, indicating an incidence of just 0.4 % for primary arthroplasty and 0.2 % for revision arthroplasty in our cohort. This is entirely consistent with the existing literature, with only short case series and few patient descriptions.
In the known cases of HTFLM, it has been more common in women older than 65 years [7–9]. Although the etiology is unknown, it has been postulated to be caused by overload secondary to muscle gait disturbances by hip prosthesis. It has also been suggested to be secondary to myopathies or neuropathies, such as denervation lumbar radiculopathies or Charcot–Marie–Tooth disease [10]. It has even been described as a result of compensatory hypertrophy due to iatrogenic superior gluteal nerve injury during surgery [11].
The largest series of patients with HTFLM has been presented by Sutter et al. [5] in a retrospective review of 35 patients with lateral hip pain who underwent MRI. They found a statistically significant association between abductor tendon rupture (gluteus medius or minimus) and the development of HTFLM. Therefore, it was recommended that clinicians seek abductor muscle injury in all cases of HTFLM. However, these authors focused on evaluating the presence of gluteal tendon rupture in these 35 patients regardless of whether they had undergone hip replacement. In our series, we focused on patients developing HTFLM after hip arthroplasty. In addition, we specifically looked for the presence of pain and increase in volume of the tensor fascia lata muscle compared to the nonsurgical contralateral hip, using the sartorius as a reference. Using this approach, we showed clear differences in tensor fascia lata muscle, but no differences in the sartorius muscle between ipsilateral and contralateral hips.
It is interesting to note that in the three patients we could assess the insertion of the gluteus tendons perfectly by MRI and we could detect rupture of the gluteus minimus tendon in all and rupture of the gluteus medius tendon in one. These data suggest that patients with painful hip arthroplasty and gluteal tendon avulsion are firm candidates to develop an ipsilateral HTFLM. Additional studies are needed to confirm this hypothesis, although we are unlikely to obtain sufficient numbers without a multicenter approach.
Although some muscle biopsies in patients with HTFLM have indicated inflammatory myopathy, others have been normal [4]. We conclude that it is not recommendable to perform biopsy and recommend that mass compatible with HTFLM be investigated by MRI [4, 11].
With regard to treatment, there is no consensus in the literature, and cases of HTFLM treated symptomatically appear to have improved without complication. Given the low frequency of the diagnosis, it will be difficult to achieve a prospective study to evaluate different treatment methods, and we recommend that treatment be considered on a case-by-case basis.
This study has several limitations. It has a retrospective design, a small number of cases (despite the extent of the initial sample), and a short follow-up period (43 months). Moreover, we did not confirm the imaging findings of HTFLM and gluteal muscle atrophy by biopsy. We consider that the avoidance of these invasive procedures is justifiable for ethical and therapeutic reasons.
Conclusion
We confirmed that HTFLM is a rare clinical entity that can mimic tumor pathology and should be considered in hips where an arthroplasty has previously been implanted. Our study benefits from meticulous study of imaging that confirmed the absence of HTFLM in the nonsurgical hip and the sartorius muscles. We also showed the benign course in our patients, without complications or the need for surgical treatment in the medium term.
Abbreviations
- HTFLM:
-
Hypertrophy of the tensor fascia lata muscle
- THA:
-
Total hip arthroplasty
- THAR:
-
THA revisions
References
Clark MA, Fisher C, Judson I, Thomas JM (2005) Soft-tissue sarcomas in adults. N Engl J Med 353:701–711
Blacksin MF, Ha D-H, Hameed M, Aisner S (2006) Superficial soft-tissue masses of the extremities. Radiographics 26(1289–3104):1
Petersilge CA, Pathria MN, Gentili A, Recht MP, Resnick D (1995) Denervation hypertrophy of muscle: MR features. J Comput Assist Tomogr 19(596):600
Ilaslan H, Wenger DE, Shives TC, Unni KK (2003) Unilateral hypertrophy of tensor fascia lata: a soft tissue tumor simulator. Skeletal Radiol 32:628–632
Sutter R, Kalberer F, Binkert CA, Graf N, Pfirrmann CWA, Gutzeit A (2013) Abductor tendon tears are associated with hypertrophy of the tensor fasciae latae muscle. SkeletalRadiol 42:627–633
Merle D’Aubigne R (1970) Cotation chiffrée de la fonction de la hanche. Rev Chir Orthop Reparatrice Appar Mot 56:481–486
Grimaldi A, Richardson C, Durbridge G, Donnelly W, Darnell R, Hides J (2009) The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia lata muscles. Man Ther 14:611–614
De Smet AA, Fisher DR, Heiner JP, Keene JS (1990) Magnetic resonance imaging of muscle tears. Skeletal Radiol 19:283–286
Flack NAMS, Meikle GR, Reddy M, Nicholson HD, Woodley SJ (2012) Hip abductor muscle volume in women with lateral hip pain: a case-controlled study. Surg Radiol Anat 34:847–855
Chang DG, Magee E, Hughes T (2008) Denervation hypertrophy in lumbosacral radiculopathy. J Neurol Neurosurg Psychiatry 79:1170
Unis DB, Hawkins EJ, Alapatt MF, Benitez CL (2013) Postoperative changes in the tensor fascia lata muscle after using the modified anterolateral approach for total hip arthroplasty. J Arthroplasty 28:663–665
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were performed in accordance with the ethical standards of the relevant institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Due to the retrospective nature of the study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Rodríguez-Roiz, J.M., Bori, G., Tomas, X. et al. Hypertrophy of the tensor fascia lata muscle as a complication of total hip arthroplasty. Eur J Orthop Surg Traumatol 27, 255–259 (2017). https://doi.org/10.1007/s00590-016-1854-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1854-z