Abstract
Introduction
The Gait Deviation Index (GDI) is a composite measure of gait abnormality derived from lower-limb joint range-of-motion which is increasingly being reported for clinical gait analysis among neurologic and orthopedic patients. A GDI score of 100 is representative of healthy individuals and decreasing scores represent a greater abnormality. Preliminary data is needed to help assess the utility of GDI as a measure of compromised gait among spine patients and to provide reference values for commonly treated pathologies.
Methods
GDI scores were obtained from healthy adults and four symptomatic degeneration groups: cervical spondylotic myelopathy (CSM), adult degenerative scoliosis (ADS), and single-level lumbar degeneration (LD). Clinical gait analysis was done using a three-dimensional motion tracking system. Evaluations were done 1 week prior to surgical intervention for degeneration groups. Two-sample t-tests were used to compare degenerative cohorts to healthy controls and for inter-cohort comparisons. Pearson correlations were used to test for significant relationships between GDI and walking speed.
Results
Degenerative cohorts all showed significantly lower (worse) GDI scores compared to healthy (all p < 0.001). CSM patients showed the best GDI scores with an average of 90, and LD patients showed the worst GDI scores with an average of 86. Worsening GDI significantly correlated with decreased walking speed among ADS patients.
Conclusion
Composite metrics like GDI provide a tempting means to summarize nuanced and complex gait characteristics into a single, comparable value among cohorts. The results of this study provide preliminary GDI scores for common degenerative spine pathologies.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The burden of degenerative spine conditions
Symptomatic conditions of the spine represent one of the largest sources of pain, disability, and health care burden in the world [1, 2]. Trends in the prevalence of surgical treatment of degenerative spine conditions have varied between neck and lumbar pathologies; however, both have shown substantial increases in cost and need for improved valuation of treatment in recent years [1,2,3,4,5,6]. Among all orthopedic procedures reported in a 2018 review of Medicare and Humana databases, incidences of lumbar degeneration and cervical degeneration were roughly 30% and 16%, respectively [2]. Individuals with degenerative spine conditions often have reduced quality of life as well as reduced functional abilities [7, 8].
Gait analysis and complexity of data
Clinical functional evaluations are increasingly being used to objectively quantify spine patient disability and in the postoperative assessment of spine surgery [9,10,11,12,13,14]. Gait analysis can provide a wide scope of gait features ranging from stride parameters (spatiotemporal parameters), dynamic joint range-of-motion angles, neuromuscular activity, and dynamic joint reaction forces [9]. These parameters can be evaluated in two-dimensional (2D) or three-dimensional (3D) plane to assess characteristics in particular anatomical planes. Often, combinations of 2D-derived measures are used to describe more complex 3D characteristics and relationships [9, 10, 15]. While advances in motion tracking and video analysis tools in recent years have made it easier to track and record complex 3D gait patterns, the data associated with these have unfortunately equally increased in size and complexity. As interest and use of clinically derived functional evaluations tailored specifically for spine patients grow, there will be a need for simple, objective measures to summarize the complexity of modern motion tracking data sets to simple, clinically meaningful and interpretable terms.
The Gait Deviation Index
While a variety of composite measures have been proposed for gait abnormality [16], the Gait Deviation Index (GDI) has been increasingly being used and reported alongside standard kinematic measures for functional gait evaluations [17,18,19]. The GDI was originally developed by Schwartz et al. [19] as a means to calculate a composite score for gait abnormality among children with cerebral palsy. The GDI was designed to be unitless with two primary features: (1) a meaningful summation of trunk and lower-extremity joint ROM variance and (2) a built-in reference to a healthy control cohort through normalization. A culmination of 15 “gait features” (kinematic joint ROM parameters) was found to account for 98% of the variance seen in lower-extremity motion which included the following: pelvic tilt, pelvic obliquity, pelvic rotation, right and left hip flexion, right and left hip adduction, right and left hip rotation, right and left knee flexion, right and left ankle dorsiflexion, and right and left foot progression (internal rotation relative to the direction of travel). For the built-in healthy control referencing, the calculation uses a set of user-definable control data to normalize the GDI score so that the average healthy score is equal to 100 and so that 1 SD is equal to 10, with decreasing scores indicating greater abnormality. In addition to its original use among cerebral palsy children, the GDI is increasingly being reported among a variety of conditions with orthopedic and neurological aspects including hip arthritis, total hip arthroplasty, and stroke patients [20,21,22,23].
Composite measures like GDI are not unlike radiographic parameters which account for multiple alignment parameters like pelvic incidence or the T1 pelvic angle [24, 25]. The purpose of a tool like GDI is to provide a single, meaningful metric that provides as much, if not more, useful information than the summation of the measures of which it is derived. This can, however, be challenging, particularly when the data may be less familiar among spine surgeons such as kinematic gait parameters. Even within standard gait analysis techniques, there can be a wide variety of analysis methods and outcome measures used which can lead to inconsistencies across studies and a lack of consensus among center-to-center comparisons of gait measures among cohorts of interest [14]. Currently, there is a need for simple measures to serve as baseline indicators of complex gait performance among spine patients. Additionally, no published GDI data of degradative spine patients referenced to normal, healthy adults are available for preliminary comparisons.
Purpose and hypothesis
The purposes of this study were: (1) to provide preliminary GDI scores and comparison for common degenerative spinal conditions, (2) to test for differences in symmetry of GDI between right and left legs, and (3) to test for relationships between GDI and walking speed. We hypothesized that patients with diagnosed degenerative spine pathologies would exhibit significantly reduced (more abnormal) GDI scores compared to healthy subjects.
Methods
Study design and subject population
This study was performed at a single, private practice institution comprised of seven contributing board-certified spine surgeons. Institutional review board approval was obtained for a retrospective cross-sectional study of symptomatic adult patients and healthy volunteers who received functional evaluations at our institution between 2016 and 2019. Symptomatic adult patients deemed eligible for surgical treatment were drawn from one of four cohorts of degenerative spinal pathologies: cervical spondylotic myelopathy (CSM), adult degenerative scoliosis (ADS), degenerative lumbar spondylolisthesis (DLS), and single-level lumbar degeneration (LD). Inclusion criteria for CSM patients included confirmed cervical spinal cord compression on imaging as well as concordant myelopathic signs or symptoms of cord dysfunction [26]. Inclusion criteria for ADS patients included a progressive and symptomatic degenerative coronal Cobb angle with concurrent axial back pain, radiculopathy, or stenosis [8, 27, 28]. Inclusion criteria for DLS patients included a spondylolisthesis of Grade II or more with symptomatic central stenosis [29]. The LD was comprised of lumbar disc herniation, single-level stenosis, and lumbar radiculopathy with back pain or claudication [27]. Beyond cohort-specific diagnostic criteria, patients were included if they were between the ages of 18 and 80 years, presented with symptomatic degeneration classified by one of the four symptomatic study cohorts and if they were able to stand and walk without assistance. Patients were excluded if they had a body mass index (BMI) of 45 kg/m2 or more, a primary neurological disorder, a diabetic neuropathy, any disease or disorder which impaired their ability to stand and walk without assistance, or if they were pregnant. Subjects for the healthy control group were recruited primarily from friends and family members of patients visiting our clinic with a goal of targeting individuals with an average level of daily activity. Table 1 provides a summary of subject demographics.
Preparatory procedures
At each evaluation, patients were fitted with a set of full-body reflective markers normally used for kinematic motion analysis by our laboratory (Fig. 1) [9]. Evaluation of the degeneration cohorts was done one week prior to surgical treatment. Degeneration cohorts also completed a set of patient-reported outcomes measures (PROMs) including visual analog scales (VAS) for pain (neck, middle-back, low-back, leg) and the Oswestry Disability Index (ODI).
Testing procedures
Each subject performed a series of five over-ground walking trials on a 10-m walkway at a normal, self-selected speed. A full gait cycle was taken from the middle of the fifth trial for kinematic analysis.
Data acquisition
Kinematic data were collected at 100 Hz using a ten-camera Vicon motion tracking system (Vicon, Oxford, UK) and was low-pass filtered using a fourth-order Butterworth filter at a 6 Hz cutoff frequency. Normalized gait cycle data of both legs of the healthy control cohort first entered into the GDI calculation as the reference set (Appendix in Table 6), and then, each degenerative cohort’s left and right GDIs were calculated [19]. Walking speed of both legs was also calculated from event timing of the kinematic data for both legs. Data analysis was done using a custom MATLAB program (The Math Works, Natick, MA, USA) and Excel (Microsoft, Redmond, WA, USA).
Statistical methods
Symmetry of GDIs between left and right legs were compared using paired t-tests within each cohort. Independent-sample (two-sample assuming equal variance) t-tests were used to compare side-averaged GDI scores of each degenerative cohort to the healthy cohort. Independent-sample (two-sample assuming equal variance) t-tests were also used for inter-cohort comparisons of side-averaged GDI among the degenerative cohorts. Pearson correlations were used to test for significant relationships between side-averaged GDI and side-averaged walking speed within each cohort. Statistical analyses were performed with Excel and R (The R Foundation for Statistical Computing, Vienna, AT).
Results
Patient-reported pain and disability
Table 2 provides a summary of PROM data for pain and disability among the degenerative cohorts. All cohorts indicated at least one score of greater than 5 which typically was the score most closely related to the region of the pathology: CSM reported the highest neck and arm pains, ADS had high low-back and leg pains, and DLS and LD had high middle-, low-back, and leg pains. All degenerative cohorts indicated severe disability with average ODI scores all being greater than 40 and an average NDI of over 40 for the CSM group.
Comparison of left- and right-sided GDI scores
Table 3 provides a summary of side-to-side comparisons of GDI and walking speeds among all study cohorts. No significant differences were found between left and right GDI scores. Significant differences were found between left and right walking speeds for CSM (p = 0.030), ADS (p = 0.003), and DLS (p = 0.001) cohorts; however, the relative differences were small.
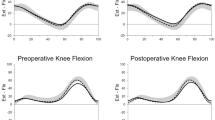
Comparisons of side-averaged GDI and walking speeds
Figure 2 provides histogram and density plots of side-averaged GDI and walking speed distributions by cohort. Table 4 provides a summary of two-sample comparisons of degenerative cohorts to healthy controls as well as inter-cohort pairwise comparisons for side-averaged GDI and side-averaged walking speed. All degenerative cohorts exhibited significantly lower GDI values compared to the healthy controls (all p < 0.001). Within the pairwise comparisons of degenerative cohorts, the only significant difference identified was with LD having a lower score than CSM (p = 0.021). All degenerative cohorts also exhibited significantly slower walking speeds compared to healthy controls (all p < 0.001). No significant difference in walking speed was seen within inter-cohort pairwise comparisons.
Correlation of GDI to walking speed
Table 5 provides a summary of Pearson correlations between side-average GDI and side-averaged walking speed. All correlation coefficients indicated positive trends between greater GDI scores and increasing walking speed; however, the only significant correlation found was for the ADS cohort with an r of 0.278 (p = 0.008).
Discussion
The goal of this study was to provide preliminary GDI scores for common degenerative spinal conditions and to identify any basic differences between cohorts and relationships of cohort GDI scores to walking speed. All degenerative cohorts showed significant abnormality in gait according to their GDI scores which were calculated relative to healthy controls. No significant differences were seen in left- versus right-sided GDI scores which indicate that gait performance was symmetric among the study cohorts, even in the presence of measurable abnormality as defined by GDI. Average GDI scores among the degenerative cohorts ranged from a value of 90 out of 100 for CSM as the highest (most normal) score to a value of 86 out of 100 for LD as the lowest (most abnormal) score. The CSM to LD comparison was the only inter-cohort comparison that reached statistical significance which indicates that differentiation of the other cohorts included in this study by score is likely not reliable with GDI alone. It is not unsurprising that DLS and LD cohorts had similar GDI scores as both share similar symptoms in terms of pain and neurological deficits [11, 30]. ADS may also share similar symptoms; however, there are added considerations such as degree of coronal deformity and a greater range of possible levels requiring treatment which may differentiate it from other lumbar pathologies in terms of effects on gait normality [9, 31]. CSM was the most unique cohort included in this study as it was the only condition representing degeneration other than lumbar. Although the GDI scores among the CSM patients were the most normal among the degradative cohorts, CSM has been shown to have strong effects on gait, balance, and proprioception due to its neurologic and myelopathic components [9, 13, 32, 33]. The findings of this study suggest that GDI may not be the best indicator for identifying the key aspects of reduced gait function among CSM patients although it may still serve as a simple measure of gait abnormality compared to healthy individuals.
Previous investigations of GDI have demonstrated a dependency of GDI to positively correlate with walking speed such that worse GDI scores reflect slower speed [22, 34]. The results of our study did show positive correlations across all groups GDI scores with walking speed, however, ADS was the only one to show a significant relationship. In a 2014 study of rheumatoid arthritis patients by Esbjornsson et al. [22], GDI was derived from data collected at both a subject-selected speed and a speed-matched GDI to account for speed-related effects and found a small but significant increase of approximately 4 points for speed-matched GDI compared to the standard calculated value (p = 0.017). While a significant change was found by adjusting GDI for speed, the degree of the change still requires further relation to clinically meaningful thresholds for interpretation. In the absence of such references, an adjustment may not necessarily provide a substantial improvement in the meaning of the base GDI score. The use of GDI in addition to standard spatiotemporal measures likely provides an optimal means to account for this dependency.
A key feature of the design of the GDI is that a single standard deviation is normalized to be approximately equal to 10 points away from the healthy control mean and that each additional 10 points away represents another standard deviation away. This scheme allows for a simple inference of the relative distance of a given score to the healthy control reference. In practice, however, there is a need to determine the meaning of a standard deviation in context with a clinically meaningful and interpretable way. Previous studies have investigated the use of reliability measures like standard error measurement (SEM) and interclass correlation (ICC) to define clinically derived thresholds relevant to a particular pathology of interest [22, 23]. These studies found varying degrees of success in determining whether GDI could be reliable and sensitive enough to be used as a meaningful outcome measure for particular pathologies. Repeatability of GDI scoring among rheumatoid arthritis patients was found to be very good resulting in good sensitivity to natural variation in gait [22]. In the present study, standard deviations among the degenerative cohorts were all approximately 10 which coincides with a single standard deviation. Additional investigation is needed to determine if variance of GDI scores among degenerative spine pathologies can allow for adequate detection of natural gait variations driven by the underlying pathologies.
Even if clinically relevant thresholds for pathology-specific GDIs can be identified, there is still a fundamental challenge in interpreting a composite score like GDI. In the original development of the GDI, Schwartz et al. [19] pointed out that meaning might be added to the GDI by considering which “gait features” are used in the calculation based on relevance to a particular pathology. In the present study, we chose to use the standard features for GDI in order to provide preliminary baseline values among our degenerative cohorts. A modified GDI calculation tailored to address more relevant features of degenerative spine pathologies could include more parameters of the torso like lumbar lordosis and thoracic kyphosis. Inclusion of such features may provide better sensitivity to spine-related conditions and to their specific characteristics of altered gait. Ultimately, the optimal strategy would likely be to use GDI in conjunction with existing, validated measures of gait function like spatiotemporal parameters and standard clinical tests like the time-up-and-go test [9, 35]. Utilization of several data types in addition to GDI may help elucidate the strengths or shortcomings of the GDI as a threshold indicator for additional, possibly more in-depth, evaluation of functional abilities.
It is important to note several limitations of this study. The healthy control group used for GDI calculation referencing is younger and has a lower BMI compared to the symptomatic cohorts which may influence the relative differences seen in the GDI scores. The calculation coefficients provided in Appendix in Table 6 can be used to compare our control group to other groups and to be used as reference data for calculation of GDI for data sets which a control is not available. Another limitation of this study was that the LD cohort was comprised of three common types of lumbar denegation which may have independent differentiating factors driving the low overall GDI score. Future investigation is needed to discern factors within this cohort. Additionally, there is an inherent error in gait analysis utilizing 3D motion tracking including variance in marker placement, accuracy in motion tracking, and the need for post-collection processing and filtering of data.
Conclusion
This study provides GDI data among patients with the most common degenerative spine conditions which were calculated using a healthy adult control reference group. These baseline data can now serve as a reference point for further evaluation of GDI to determine its suitability and relevance to spine patients. Additionally, by referring to our healthy control coefficients, other research centers can compare GDI data from their own patients and to other healthy controls. The findings of this study indicate that the standard GDI score as originally developed can indeed identify significant abnormalities across all degenerative cohorts included in this study. When used in conjunction with other functional gait measure like spatiotemporal measures or standard clinical tests, the GDI may serve as a single value and useful baseline indicator of poor gait ability and further examination. Future investigations are needed to further examine the sensitivity and reliability of GDI as a useful and meaningful indicator of gait abnormality among spine pathologies.
References
Vos T, Bell BR (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800
Buser Z et al (2018) Spine degenerative conditions and their treatments: National Trends in the United States of America. Global Spine J 8(1):57–67
Zygourakis CC et al (2017) Geographic and hospital variation in cost of lumbar laminectomy and lumbar fusion for degenerative conditions. Neurosurgery 81(2):331–340
Weinstein JN et al (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 31(23):2707–2714
Liu CY et al (2017) Trends in utilization and cost of cervical spine surgery using the national inpatient sample database, 2001 to 2013. Spine (Phila Pa 1976) 42(15):e906–e913
Martin BI et al (2008) Expenditures and health status among adults with back and neck problems. JAMA 299(6):656–664
Devin CJ et al (2015) A cost-utility analysis of lumbar decompression with and without fusion for degenerative spine disease in the elderly. Neurosurgery 77(Suppl 4):S116–S124
Diebo BG et al (2019) Adult spinal deformity. Lancet 394(10193):160–172
Haddas R et al (2018) The use of gait analysis in the assessment of patients afflicted with spinal disorders. Eur Spine J 27:1712
Lenke LG et al (2001) Prospective dynamic functional evaluation of gait and spinal balance following spinal fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 26(14):E330–7
Malone A, Meldrum D, Bolger C (2015) Three-dimensional gait analysis outcomes at 1 year following decompressive surgery for cervical spondylotic myelopathy. Eur Spine J 24(1):48–56
Yagi M et al (2017) Walking balance and compensatory gait mechanisms in surgically treated patients with adult spinal deformity. Spine J 17(3):409–417
Nishimura H et al (2015) Gait analysis in cervical spondylotic myelopathy. Asian Spine J 9(3):321–326
Siasios ID et al (2017) The role of gait analysis in the evaluation of patients with cervical myelopathy: a literature review study. World Neurosurg 101:275–282
Paul JC et al (2015) Feasibility of a cost-effective, video analysis software-based mobility protocol for objective spine kinematics and gait metrics: a proof of concept study. PM & R 7(3):336–339
Cimolin V, Galli M (2014) Summary measures for clinical gait analysis: a literature review. Gait Posture 39:1005–1010. https://doi.org/10.1016/j.gaitpost.2014.02.001
Hillman SJ et al (2007) Correlation of the Edinburgh Gait Score with the Gillette Gait Index, the Gillette Functional Assessment Questionnaire, and dimensionless speed. J Pediatr Orthop 27(1):7–11
Novacheck TF, Stout JL, Tervo R (2000) Reliability and validity of the Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. J Pediatr Orthop 20(1):75–81
Schwartz MH, Rozumalski A (2008) The Gait Deviation Index: a new comprehensive index of gait pathology. Gait Posture 28(3):351–357
Jensen C et al (2015) The use of the Gait Deviation Index for the evaluation of participants following total hip arthroplasty: an explorative randomized trial. Gait Posture 42(1):36–41
Rosenlund S et al (2016) The Gait Deviation Index Is associated with hip muscle strength and patient-reported outcome in patients with severe hip osteoarthritis: a cross-sectional study. PLoS ONE 11(4):e0153177
Esbjornsson AC et al (2014) Quantifying gait deviations in individuals with rheumatoid arthritis using the Gait Deviation Index. Scand J Rheumatol 43(2):124–131
Correa KP et al (2017) Reliability and Minimum Detectable Change of the Gait Deviation Index (GDI) in post-stroke patients. Gait Posture 53:29–34
Protopsaltis T et al (2014) The t1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 96(19):1631–1640
Iyer S et al (2018) Sagittal spinal alignment in adult spinal deformity: an overview of current concepts and a critical analysis review. JBJS Rev 6:e2
Kim HJ et al (2013) Differential diagnosis for cervical spondylotic myelopathy: literature review. Spine (Phila Pa 1976) 38(22 Suppl 1):S78–S88
Ailon T et al (2015) Degenerative spinal deformity. Neurosurgery 77(Suppl 4):S75–S91
Schwab F et al (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082
Matz PG et al (2016) Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 16(3):439–448
Meyers LL et al (1999) Mechanical instability as a cause of gait disturbance in high-grade spondylolisthesis: a pre- and postoperative three-dimensional gait analysis. J Pediatr Orthop 19(5):672–676
Yagi M et al (2018) Effect of the upper instrumented vertebral level (upper vs. lower thoracic spine) on gait ability after corrective surgery for adult spinal deformity. Spine J 18(1):130–138
Haddas R et al (2018) Spine and lower extremity kinematics during gait in patients with cervical spondylotic myelopathy. Spine J 18(9):1645–1652
Haddas R et al (2019) Characterizing gait abnormalities in patients with cervical spondylotic myelopathy: a neuromuscular analysis. Spine J 19:11
Rozumalski A, Schwartz M (2012) A method to reference the Gait Deviation Index to a speed-matched control. Gait Posture 36:S51–S52
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Acknowledgements
We acknowledge the Viscoliogsi family for their support of the Texas Back Institute Spine Biomechanics Laboratory.
IRB Approval
The study was approved by the Western Institutional Review Board (IRB#: 20152881).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table 6.
Rights and permissions
About this article
Cite this article
Mar, D., Lieberman, I. & Haddas, R. The Gait Deviation Index as an indicator of gait abnormality among degenerative spinal pathologies. Eur Spine J 29, 2591–2599 (2020). https://doi.org/10.1007/s00586-019-06252-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06252-2