Abstract
Purpose
Although subjects with recurrent low back pain (LBP) demonstrate altered postural control, their postural steadiness during one leg standing is unknown. The purpose of this study was to investigate postural steadiness based on relative kinematic index of the lower limbs and trunk with normalized standing time in subjects with recurrent LBP during dominant and non-dominant leg standing.
Methods
Sixty individuals participated in the study, including 29 subjects in the control group (18 male, 11 female) and 31 subjects with recurrent LBP (21 male, 10 female). The outcome measures included relative kinematic index of the body regions and normalized standing time during the one leg standing test. The relative kinematic index was the ratio between standstill time and successful standing time. The normalized standing time was defined as a ratio between the successful standing time and the requested standing time.
Results
The control group demonstrated significantly longer normalized standing time on the dominant (t = −2.57, p = 0.013) and non-dominant (t = −2.78, p = 0.007) legs than the LBP group. The relative kinematic index of the core spine model significantly decreased for the dominant (t = −3.01, p = 0.004) and non-dominant (t = −3.06, p = 0.003) legs in the LBP group. In addition, the kinematic index indicated pelvis and non-dominant shank during dominant leg standing (R 2 = 0.97) in the LBP group. In the control group, the pelvis was significantly correlated with the core spine model during standing on the dominant (R 2 = 0.95) and non-dominant (R 2 = 0.97) legs.
Conclusions
The relative kinematic index of the pelvis was found to be most significant for longer standing durations in both groups. In the LBP group, the shank and foot were significantly higher in addition to the pelvis due to possible compensatory motion. The control group took advantage of pelvic control with the core spine to minimize lower limb movements. Clinicians need to consider the core spine for pelvic control to refine postural adaptations in subjects with recurrent LBP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) affects much of the public population’s work performance and social responsibilities and has increasingly contributed to escalating health-care costs [1]. LBP alone affects up to 80 % of the population at some point in one’s life, and 1–2 % of the adult population in the United States is disabled because of LBP [2]. It is known that subjects with recurrent LBP demonstrate a less refined positional sense and altered proprioceptive postural control [3].
The postural control deficits [4] and decreased abdominal and paraspinal muscle strength play important roles in understanding the characteristics of LBP [5–7]. However, most studies have not compared LBP groups with control groups and have not included standardized methodological procedures with clearly defined inclusion/exclusion criteria. Although these studies attempted to determine posture analysis with motor control, the function of the transversus abdominis muscle must be understood in relation with other body regions, including the lower limbs. It would be necessary to conduct a comprehensive investigation to determine posture analysis based on the control of the lower limbs and trunk during one leg standing in subjects with and without recurrent LBP.
The ability to adapt postural sway as a function of the lower limbs and trunk is a critical component of daily life. However, the effect of minimized lower limbs and trunk motion on increased postural sway by isolating individual body segments is unknown. Postural steadiness is used to characterize the dynamics of the postural control system associated with maintaining balance during quiet standing and is a basic requirement to prevent early mechanical deterioration of balance. The literature reports a number of biomechanical and clinical definitions of postural steadiness, but a consensus on the definition is lacking [8, 9].
Previous studies have indicated that core stability could be increased by effective recruitment of trunk muscles to allow for optimal force production, coordinated lumbopelvic movement, and appropriate load transfers from the spine to distal segments [10–12]. Core spine stability involves a highly integrated activation of multiple segments that provide steadiness and generate interactive movement. However, compensatory patterns of core stability and limb motions for postural steadiness have not been carefully investigated and have failed to show any clinical significance. It is important to understand that a pain avoidance strategy might be related to core spine control in subjects with recurrent LBP. To assess postural control in subjects with recurrent LBP, the relative lower limb movements and normalized standing time during one leg standing test were utilized since approximately 40 % of human gait movement occurs during one leg stance [13, 14].
In our study, postural steadiness was analyzed based on the relative kinematic index and normalized standing time during the one leg standing test. The relative kinematic index was the ratio between standstill time and successful standing time. The normalized standing time was defined as a ratio between the successful standing time and the requested standing time. In addition, the core spine model was utilized as a reference model for motion analysis to compare specific three-dimensional kinematic changes of the lumbar spine, which is directly articulated between the pelvis and thorax. Core spine steadiness requires dynamic rotational kinematic balance when standing on one leg. In a previous study, the subjects with recurrent LBP demonstrated higher lumbar spine rotational steadiness, which might be due to a possible pain avoidance strategy from the standing limb [15].
It is crucial to maintain postural steadiness of the trunk and lower limbs under static and dynamic conditions. Hamaoui et al. reported that increased postural sway from structural stiffness in subjects with LBP was not related to spinal motion, but was related to dynamic mobility capacity [16]. This postural steadiness might be linked to an increase in muscular active tension, which reduces dynamic mobility capacity in the trunk and lower limbs. Therefore, postural steadiness based on the relative lower limb movements and normalized standing time during the one leg test will provide a better understanding of integrated motor function for impaired balance performance in subjects with LBP.
A kinematic investigation by the one leg standing test could also be useful in understanding postural steadiness and functional improvement in subjects with and without recurrent LBP. The control group, as compared to the LBP group, might be able to adapt compensatory motions to activate pelvic control with the core spine to stabilize lower limb movements during one leg standing. Therefore, the purpose of this study was to investigate postural steadiness based on the relative kinematic index of the lower limbs and trunk with normalized standing time in subjects with recurrent LBP during dominant and non-dominant leg standing.
Methods
Target population
Subjects were recruited from the University community, and those subjects who met the study’s inclusion criteria received information regarding the study design and signed a copy of the Institutional Review Board approved consent form (IRB#8-15B). Subjects with recurrent LBP were eligible to participate if they: (1) were 20 years of age or older and right leg dominant, (2) had recently recovered from bilateral LBP as defined by de Vet et al. [17], (3) had no current episode of acute pain referral into the upper/lower extremities at least 1 month prior to the data collection, (4) had no structural dysfunction of the spine or lower extremities at the time of data collection, which was determined by the subjects’ family physicians, and (5) had no conditions which would prevent them from standing on each leg for 25 s with their eyes closed without impaired balance (e.g., central nervous system disorder, neuromuscular disorder, vestibular disorder, diabetes).
Subjects with recurrent LBP were excluded from participation if they: (1) had a diagnosed psychological illness that might interfere with the study protocol, (2) had overt neurological signs (sensory deficits or motor paralysis), (3) had a structural spinal problem, such as scoliosis, as confirmed by X-ray, and/or (4) were pregnant. Participants were able to withdraw from the study if they requested to withdraw. The control group was matched based on demographic characteristics with the recurrent LBP group.
Lower extremity dominance was also applied in this study since a previous study confirmed that dominance could be a confounding factor [18]. The right lower extremity was regarded as the dominant side for all subjects since they preferred to use the right limb to kick a ball [19, 20]. The non-dominant side standing protocol was defined as standing on the left leg with the right hip and knee flexed approximately 90° during the test.
Outcome measures
Pain/disability was inferred from self-reported scores on the Oswestry Disability Index (ODI) [21]. The ODI is one of the most frequently used tools for measuring chronic disability. A sum of the scores is calculated and presented as a percentage, where 0 % indicates no disability and 100 % indicates the worst possible disability.
Six digital cameras captured the motion of each marker three-dimensionally (Motion Analysis Corporation, Santa Rosa, CA, USA) with the sampling rate of 60 Hz. Marker trajectories were low pass filtered (6 Hz, 4th order Butterworth filter) and then time synchronized within the test cycle into Matlab R2010b (The MathWorks, Inc. Natick, MA).
A total of 34 reflective markers were placed over the bilateral acromioclavicular joints, anterior superior iliac spines (ASIS), posterior superior iliac spines (PSIS), iliac crests, greater trochanters, lateral thighs, lateral and medial epicondyles of the knees, lateral shanks, lateral and medial malleoli, heels, second toes, lateral humeral epicondyles, radial styloid processes, and hands. There were also markers placed on the seventh cervical vertebra (C7) and the middle of the manubrium.
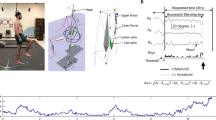
The subjects were given disposable hospital slipper socks with nonslip bottoms to wear during the test in the Motion Analysis Laboratory. The subjects stood upright on their dominant and non-dominant legs separately in random order for 25 s. They stood on a force plate with their eyes closed and the contralateral hip and knee flexed to 90° (Fig. 1). Subjects performed two trials in which they were instructed to stand on a single leg. Subjects were asked to keep their arms along the sides of their trunks in standing, although compensatory arm movements were permitted to maintain balance.
a One leg standing test. The subject maintained postural steadiness while the kinematic data were gathered from the three axes (R x , R y , and R z ). b The identification of successful standing time and standstill time for computing the relative kinematic index. An example of the normalized core spine kinematic changes during the test. The analysis time window excluded the initial transition time (5 s) from standing. The three-dimensional rotation (R xyz ) of the tested axis was below (5°) threshold (Th_k: kinematic threshold)
The angular rotations of the following body regions were collected: pelvis, right and left thighs, right and left shanks, right and left feet, head, upper thorax, lower thorax, lumbar spine, and the core spine model. To capture the motion, the Helen Hayes full body (with head) reflective marker set was used during the task as based on the previous study [22].
Angular rotations of the body segments were recorded, and the segment was created by three non-collinear markers. Those markers were placed on the body segment such that two markers defined a segmental axis, and the third marker formed a segmental anatomical plane. A plane was required to represent each segment so that tri-axial rotation could be fully defined as the joint coordinate system embedded into each body segment for calculation of intersegmental joint angles [23]. For example, the lumbar spine rotation was three-dimensionally defined by a vector from a marker superficial to the second sacrum level (S2) to a marker superficial to the first lumbar process (L1); the lower thoracic region was defined by a vector from the L1 marker to a marker superficial to the sixth thoracic spinous process (T6); the upper thoracic region segment was defined by a vector from the T6 marker to a marker superficial to C7. The body segments were modeled as rigid bodies, and the relative rotation angle was taken from a fixed point in the center of the joint. The kinematic angles were applied to describe relative rotations of one segment with respect to another reference segment based on three markers per rigid body to accurately measure the angular changes. Therefore, lumbar spine angles were derived from the relative orientation based on the core spine axis.
The core spine model was the reference axis from the pelvic plane of S2 and was used to compare specific three-dimensional motions. The core spine was defined as a highly integrated activation of multiple segments that provide steadiness and generate interactive movement. This core spine model needed to be quantified by isolating individual components to reproduce the three-dimensional motions that are used by the core to accomplish its function [10]. The relative kinematic changes were based on the core spine model to compare with other body segments. The pelvic coordinate system was defined, and the origin was set at the S2 marker. The ASIS markers defined the x–y plane of the pelvis, and the positive z-axis was defined by a vector perpendicular to the x–y plane. A computational method that uses vector algebra was utilized for angular joint kinematics, which is the recommended method by the International Society for Biomechanics [23].
In Fig. 1a, the normalized standing time is defined as a ratio between the successful standing time and the requested standing time (Eq. 1). The successful standing time was the amount of time the subject was able to successfully stand based on the amount of time requested (25 s). For the data analysis, only 20 s of the 25 s standing test protocol was utilized. The analysis time window excluded the initial transition time (5 s) from double leg standing to single leg standing to minimize individual variations.
In Fig. 1b, the relative kinematic index is the ratio between standstill time and successful standing time (Eq. 2). The standstill time was the summation of temporal segments where the three-dimensional rotation (R xyz ) of the tested axis was below the threshold. The R xyz was defined as the rotational angle of each specific body region (Eq. 3), which was calculated between two adjacent joints in three dimensions and then combined to quantify the relative kinematic index. Again, the data analysis included the angular rotation changes from the starting posture, which was at a time of 5 s, instead of the time of initiation of the test (a time of 0 s).
Regarding three-dimensional angular kinematics data, the relative kinematic index was calculated for each segment, side-to-side (R x ), back-and-forth (R y ), and up-and-down (R z ), from a mean value. Therefore, the R xyz was computed as a square sum of the three rotations of which the mean was subtracted to have zero-mean as was previously reported [24]. The R x_mean is the average value of R x over the analysis window. The R y_mean and R z_mean were from the R y and R z signals, respectively.
Statistical analysis
Statistical analyses were completed using SPSS 22 (SPSS, Chicago, IL). Normality was assessed for each dependent variable (normalized standing time, relative kinematic index) during dominant and non-dominant leg standing. An independent t test was used to analyze normalized standing time based on groups. A Pearson correlation analysis was used to analyze the degree of associations with the relative kinematic index for whole body regions and the normalized standing time between groups. Pearson r was interpreted as 0.0–0.25 for little to no relationship, 0.26–0.50 for a fair relationship, 0.51–0.75 for a moderate to good relationship, and 0.76–1 for a good to excellent relationship [25].
A stepwise multiple regression analysis was conducted to find the most critical factors of the relative kinematic index for normalized standing time between groups. For all statistical tests, type I error rate was set at 0.05.
Results
Description of samples
A summary of subject demographics and the relationship of groups are indicated in Table 1. In total, 60 subjects enrolled in the study, including 29 control subjects (18 male, 11 female) and 31 LBP participants (21 male, 10 female). There were no significant age (t = 1.84, p = 0.07) or gender (χ 2 = 0.21, p = 0.79) differences between groups. Height (t = −1.29, p = 0.20) and weight (t = 0.59, p = 0.55) were not significantly different between groups. The LBP group reported an average ODI score of 21 %, which is within the moderate disability level (20–40 %). The control group reported that their ODI score was 0 %.
The standing duration and kinematic data
The standing duration (s) was compared between dominant and non-dominant leg standing between the groups. During dominant leg standing, the control group demonstrated significantly longer standing duration (25.51 ± 4.17) than the LBP group (21.79 ± 6.68), and there was a statistically significant difference between groups (F = 7.73, p = 0.007). During non-dominant leg standing, the control group demonstrated significantly longer standing duration (24.57 ± 4.16) than the LBP group (20.51 ± 6.75), and there was a statistically significant difference between groups (F = 6.60, p = 0.013).
As shown in Table 2, there were significant relative kinematic index differences between groups during dominant leg standing for the pelvis (t = −3.68, p = 0.001), dominant shank (t = −3.39, p = 0.001), non-dominant shank (t = −2.17, p = 0.03), head (t = −2.14, p = 0.03), upper thorax (t = −4.87, p = 0.001), lower thorax (t = −3.98, p = 0.001), lumbar spine (t = −2.02, p = 0.04), and core spine model (t = −3.01, p = 0.004). During non-dominant leg standing, there were also significant relative kinematic index differences between groups for the pelvis (t = −2.06, p = 0.04), dominant shank (t = −2.20, p = 0.03), upper thorax (t = −3.15, p = 0.01), lower thorax (t = −2.63, p = 0.01), lumbar spine (t = −2.13, p = 0.04), and core spine model (t = −3.06, p = 0.003).
Kinematic factors for normalized standing time
Correlation analysis was conducted comparing relative kinematic index and normalized standing time (Table 3). In the control group, the normalized standing time for the relative kinematic index was correlated with the lumbar spine (r = 0.92, p < 0.01 on dominant side; r = 0.64, p < 0.01 on non-dominant side). The non-dominant foot also demonstrated a very strong relationship (r = 0.93, p < 0.01) with dominant leg standing in the control group; however, the LBP group was not significantly correlated. The LBP group demonstrated normalized standing duration with the lumbar spine (r = 0.87, p < 0.01 on dominant side; r = 0.63, p < 0.01 on non-dominant side).
As shown in Table 4, the relative kinematic index of the core spine model was correlated with the pelvis (r = 0.98, p < 0.01 on dominant leg; r = 0.98, p < 0.01 on non-dominant leg) in the control group. For the LBP group, the relative kinematic index of the core spine model was correlated with the pelvis (r = 0.98, p < 0.01 in dominant leg standing; r = 0.94, p < 0.01 in non-dominant leg standing) and the lower thorax (r = 0.62, p < 0.01 in dominant leg standing; r = 0.50, p < 0.01 in non-dominant leg standing).
A stepwise multiple regression analysis was conducted to find the significant relative kinematic index of the lower limbs for normalized standing time (Table 5). The control group demonstrated that the relative kinematic index of the pelvis, as a predictor, accounted for 96 % of the variance for normalized standing time during dominant leg standing (F = 627.97, p < 0.01) and 97 % of the variance for normalized standing time during non-dominant leg standing (F = 890.38, p < 0.01).
However, the pelvis and non-dominant shank were included as predictor variables and accounted for 97 % of the variance for normalized standing time (F = 747.59, p < 0.01) during dominant leg standing in the LBP group. During non-dominant leg standing, the pelvis and non-dominant foot were included as predictor variables and accounted for 89 % of the variance for normalized standing time (F = 129.70, p < 0.01) in the LBP group.
Discussion
The purpose of this study was to investigate postural steadiness based on relative kinematic index of the lower limbs and trunk with normalized standing time in subjects with recurrent LBP during dominant and non-dominant leg standing. The results of this study indicated that the subjects in the control group demonstrated significantly longer one leg standing as they took advantage of pelvic control with core spine steadiness to minimize lower limb movements while the LBP group did not.
One of the key points of this study was to investigate the specific body segments related to the relative kinematic index of the lower limbs and trunk with normalized standing time. It has been reported that impaired back muscle function may lead to an inability to adapt postural control strategies to the prevailing conditions in subjects with LBP [26, 27]. The longer standing duration in the control group might be due to motor learning of functional activities that allows for enhancement of postural control strategies [4, 28]. This difference in balance performance may be more pronounced in subjects with recurrent LBP due to diminished proprioceptive conditions in the lumbar spine [27, 29]. The results of the correlation analysis indicated that dominant leg standing was significantly associated with the lumbar spine in the control group. Non-dominant leg standing was also associated with the lumbar spine in the control group.
To maintain postural steadiness during the test, the lower limbs and trunk require not only reliable sensory feedback and muscle activation from all involved joints, but also the sensitive response of proprioceptive receptors to environmental changes [24, 30, 31]. The neuromuscular control on the trunk was often altered in the chronic LBP group [32], which made it difficult to control specific tasks that require the extensors to contribute to trunk steadiness and primary movement control in subjects with recurrent LBP. The differences in balance performance are more pronounced on the dominant side in subjects with recurrent LBP due to diminished proprioceptive conditions [27, 29]. The findings of lower thorax steadiness for normalized standing time in the LBP group may be due to relatively limited lumbar spine motion. Therefore, pelvic motion during one leg standing might be important for trunk control within the whole spine to accommodate balance strategies compared with the core spine model.
The core spine was integrated with the pelvis in the control group during dominant and non-dominant leg standing. The control group might have been able to take advantage of pelvic control with the core spine as a postural strategy to achieve longer one leg standing. The kinematic index of the upper and lower thoraces was also significantly correlated with the core spine during non-dominant leg standing in the LBP group. For the LBP group, the core spine model was associated with the lower limbs in addition to pelvic rotation steadiness. For dominant leg standing, the pelvis and non-dominant shank were associated with the core spine. During non-dominant leg standing, however, the pelvis and non-dominant foot were associated with the core spine. These results were consistent with other studies that found that the control group demonstrated better control than the LBP group [22, 33]. This model would be expected to stabilize limb movements with the integrated core spine, which is closely located to the body’s center of mass on the standing limb.
The results of our study indicated that pelvic control was most significant for longer standing in both groups. In the LBP group, the relative kinematic indices of the shank and foot were significant in addition to the pelvis due to possible compensatory motion. The control group took advantage of pelvic control with the core spine to minimize lower limb movements. This pelvic control might be related with postural steadiness, which requires not only reliable muscle activation from all involved joints, but also the sensitive response of proprioceptive receptors [24, 31, 34]. Examining spinal dysfunction while considering the core spine model may provide clinical insight into the pattern of trunk movements that occur due to pelvic control in subjects with recurrent LBP [22, 24]. Different postural strategies of whole body kinematic coordination with the core spine could enhance stabilization strategies in subjects with recurrent LBP. The variations in balance and body sway are compensated for by changes in postural alignment and core spine steadiness of the dominant thigh and pelvis [24, 28].
Although the scope of this study did not include compensatory movements of the upper extremities, compensatory lower limb movements in the recurrent LBP group provide additional insights for future studies regarding postural integrity. The participants in the control group were able to maintain their balance with pelvic control, which provides evidence of the reorganization of the trunk muscles that might be associated with deficits in postural control in individuals with recurrent LBP [4]. The postural control of the trunk muscles contributes to the recurrence of pain episodes due to neural changes that underlie these motor deficits [4, 35].
The results of our study indicated that the control group demonstrated significantly longer standing times on the dominant and non-dominant legs than the LBP group. The control of kinematic steadiness may also include changes in excitability in the motor pathway, changes in the sensory system, and factors associated with stressful and fearful aspects of pain [36, 37]. Those subjects with recurrent LBP need to meet the necessary postural integrity of compensatory mechanisms when reducing the risk of injury in balance activities [22, 28, 38]. The results of our study emphasize the need for pelvic steadiness for postural compensation, which might be beneficial to utilize as outcome measurements following specific interventions with the one leg standing test in future studies.
There were several limitations to the current study. One limitation was the age variation of the participants with LBP (who ranged from 21 to 49 years). This age variation might invalidate the results even with statistical adjustments for continuous variables as covariates. However, subgroup analyses would provide more accurate results of intra-/intervariability for future studies. Second, it would be beneficial to perform a validation study to ensure the sensitivity and reproducibility of the methodology. The comparison of postural control based on normalized standing time and relative kinematic index might contribute to a further understanding of postural steadiness and quantification of balance deficits in subjects with recurrent LBP. In addition, the relative kinematic index in the current analysis included the angular displacement changes from the starting posture, which was 5 s later, instead of the time (25 s) of initiation of the test. As previously reported, the successful duration was defined as the total standing time until the subject failed to maintain steadiness during the 20 s of the test window, which excludes the initial 5 s of the standing protocol [22]. It would also be beneficial to quantify the capacity of motor control patterns to compare the first 5 s as the initiation control stage and the next 20 s as the stabilization stage during the test.
The scope of this study included compensatory movements with one leg standing; however, it would be interesting to quantify movements with various tasks to investigate the characteristics of kinematic analysis measures. The comparison of postural control based on the normalized kinematic steadiness measures for standing duration might contribute to a further understanding of postural adaptation in subjects with recurrent LBP.
Conclusion
Postural steadiness based on the relative kinematic index with normalized standing time should be further investigated to determine integrated balance performance. The control group took advantage of pelvic control with the core spine to minimize lower limb movements. Statistically significant and clinically relevant differences in core spine and pelvic control might be useful for outcome measurements to assess postural steadiness.
References
Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA (2014) Epidemiology of low back pain in adults. Neuromodulation 17(Suppl 2):3–10. doi:10.1111/ner.12018
Deyo RA, Weinstein JN (2001) Low back pain. N Engl J Med 344:363–370. doi:10.1056/NEJM200102013440508
Brumagne S, Janssens L, Knapen S, Claeys K, Suuden-Johanson E (2008) Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J 17:1177–1184. doi:10.1007/s00586-008-0709-7
Tsao H, Galea MP, Hodges PW (2008) Reorganization of the motor cortex is associated with postural control deficits in recurrent low back pain. Brain 131:2161–2171. doi:10.1093/brain/awn154
Heidari P, Farahbakhsh F, Rostami M, Noormohammadpour P, Kordi R (2015) The role of ultrasound in diagnosis of the causes of low back pain: a review of the literature. Asian J Sports Med 6:e23803. doi:10.5812/asjsm.23803
Hides J, Wilson S, Stanton W, McMahon S, Keto H, McMahon K, Bryant M, Richardson C (2006) An MRI investigation into the function of the transversus abdominis muscle during “drawing-in” of the abdominal wall. Spine (Phila Pa 1976) 31:E175–E178. doi:10.1097/01.brs.0000202740.86338.df
Teyhen DS, Miltenberger CE, Deiters HM, Del Toro YM, Pulliam JN, Childs JD, Boyles RE, Flynn TW (2005) The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther 35:346–355
Izzo R, Guarnieri G, Guglielmi G, Muto M (2013) Biomechanics of the spine. Part I: spinal stability. Eur J Radiol 82:118–126. doi:10.1016/j.ejrad.2012.07.024
Jonsson E, Seiger A, Hirschfeld H (2005) Postural steadiness and weight distribution during tandem stance in healthy young and elderly adults. Clin Biomech (Bristol, Avon) 20:202–208. doi:10.1016/j.clinbiomech.2004.09.008
Kibler WB, Press J, Sciascia A (2006) The role of core stability in athletic function. Sports Med 36:189–198 (pii: 3631)
Lee T, Kim YH, Sung PS (2011) A comparison of pain level and entropy changes following core stability exercise intervention. Med Sci Monit 17:CR362–CR368 (pii: 881846)
Mok NW, Yeung EW, Cho JC, Hui SC, Liu KC, Pang CH (2015) Core muscle activity during suspension exercises. J Sci Med Sport 18:189–194. doi:10.1016/j.jsams.2014.01.002
Aberg AC, Thorstensson A, Tarassova O, Halvorsen K (2011) Calculations of mechanisms for balance control during narrow and single-leg standing in fit older adults: a reliability study. Gait Posture 34:352–357. doi:10.1016/j.gaitpost.2011.05.025
Verhagen E, Bobbert M, Inklaar M, van Kalken M, van der Beek A, Bouter L, van Mechelen W (2005) The effect of a balance training programme on centre of pressure excursion in one-leg stance. Clin Biomech (Bristol, Avon) 20:1094–1100. doi:10.1016/j.clinbiomech.2005.07.001
Sung PS, Leininger PM (2015) A kinematic and kinetic analysis of spinal region in subjects with and without recurrent low back pain during one leg standing. Clin Biomech (Bristol, Avon) 30:696–702. doi:10.1016/j.clinbiomech.2015.05.003
Hamaoui A, Do MC, Bouisset S (2004) Postural sway increase in low back pain subjects is not related to reduced spine range of motion. Neurosci Lett 357:135–138
de Vet HC, Heymans MW, Dunn KM, Pope DP, van der Beek AJ, Macfarlane GJ, Bouter LM, Croft PR (2002) Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine 27:2409–2416. doi:10.1097/01.BRS.0000030307.34002.BE
Sung PS, Spratt KF, Wilder DG (2004) A possible methodological flaw in comparing dominant and nondominant sided lumbar spine muscle responses without simultaneously considering hand dominance. Spine (Phila Pa 1976) 29:1914–1922 (pii: 00007632-200409010-00016)
Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR (2010) Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med 44:694–697. doi:10.1136/bjsm.2008.051243
Andersen TE, Floerenes TW, Arnason A, Bahr R (2004) Video analysis of the mechanisms for ankle injuries in football. Am J Sports Med 32:69S–79S
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Sung PS, Yoon B, Lee DC (2010) Lumbar spine stability for subjects with and without low back pain during one-leg standing test. Spine (Phila Pa 1976) 35:E753–E760. doi:10.1097/BRS.0b013e3181d53b9c
Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. Int Soc Biomech J Biomech 35:543–548 (pii: S0021929001002226)
Lee DC, Ham YW, Sung PS (2012) Effect of visual input on normalized standing stability in subjects with recurrent low back pain. Gait Posture 36:580–585. doi:10.1016/j.gaitpost.2012.05.020
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Elfving B, Dedering A, Nemeth G (2003) Lumbar muscle fatigue and recovery in patients with long-term low-back trouble—electromyography and health-related factors. Clin Biomech (Bristol, Avon) 18:619–630
Johanson E, Brumagne S, Janssens L, Pijnenburg M, Claeys K, Paasuke M (2011) The effect of acute back muscle fatigue on postural control strategy in people with and without recurrent low back pain. Eur Spine J 20(12):2152–2159. doi:10.1007/s00586-011-1825-3
Tsao H, Hodges PW (2008) Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J Electromyogr Kinesiol 18:559–567. doi:10.1016/j.jelekin.2006.10.012
Hodges PW, Moseley GL (2003) Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol 13:361–370
Silfies SP, Bhattacharya A, Biely S, Smith SS, Giszter S (2009) Trunk control during standing reach: a dynamical system analysis of movement strategies in patients with mechanical low back pain. Gait Posture 29:370–376. doi:10.1016/j.gaitpost.2008.10.053
Clark NC, Roijezon U, Treleaven J (2015) Proprioception in musculoskeletal rehabilitation. Part 2: clinical assessment and intervention. Man Ther 20:378–387. doi:10.1016/j.math.2015.01.009
Silfies SP, Squillante D, Maurer P, Westcott S, Karduna AR (2005) Trunk muscle recruitment patterns in specific chronic low back pain populations. Clin Biomech (Bristol, Avon) 20:465–473
Jo HJ, Song AY, Lee KJ, Lee DC, Kim YH, Sung PS (2011) A kinematic analysis of relative stability of the lower extremities between subjects with and without chronic low back pain. Eur Spine J 20(8):1297–1303. doi:10.1007/s00586-010-1686-1
Silfies SP, Bhattacharya A, Biely S, Smith SS, Giszter S (2009) Trunk control during standing reach: a dynamical system analysis of movement strategies in patients with mechanical low back pain. Gait Posture 29:370–376
Hodges PW, Tucker K (2011) Moving differently in pain: a new theory to explain the adaptation to pain. Pain 152:S90–S98
Tsao H, Danneels LA, Hodges PW (2011) Smudging the motor brain in young adults with recurrent low back pain. Spine (Phila Pa 1976) 36:1721–1727. doi:10.1097/BRS.0b013e31821c4267
Strutton PH, Theodorou S, Catley M, McGregor AH, Davey NJ (2005) Corticospinal excitability in patients with chronic low back pain. J Spinal Disord Tech 18:420–424 (pii: 00024720-200510000-00008)
Park WH, Kim YH, Lee TR, Sung PS (2012) Factors affecting shoulder-pelvic integration during axial trunk rotation in subjects with recurrent low back pain. Eur Spine J. doi:10.1007/s00586-012-2280-5
Acknowledgments
This work was supported by the Herbert H. and Grace A. Dow College of Health Professions at Central Michigan University. The authors also thank to Dr. Dongchul C. Lee (Director of Theoretical Research in Nevro Corp. Redwood City, CA. USA) for his critical analyses of the important intellectual content and the interpretation of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any financial or personal conflicts of interest in relation to the submission, other people, or any organizations.
Rights and permissions
About this article
Cite this article
Sung, P.S., Danial, P. Analysis of relative kinematic index with normalized standing time between subjects with and without recurrent low back pain. Eur Spine J 26, 518–527 (2017). https://doi.org/10.1007/s00586-016-4727-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4727-6