Abstract
Background
Adaptations of dynamic balance performance are related to sway excursions in older adults with chronic low back pain (LBP). However, there is a lack of understanding on postural control within different thresholds of radius from the center of pressure (COP).
Purpose
This study was conducted to compare the normalized stability based on the time-in-boundary (TIB) during repeated unilateral limb standing trials between subjects with and without chronic LBP.
Methods
There were 26 older adults with LBP and 39 control subjects who completed three trials of repeated unilateral limb standing on a force plat.
Results
The TIB based on the seven thresholds was analyzed, and the groups demonstrated a significant interaction on thresholds for TIB (F = 8.76, p = 0.01). The TIB was significantly different in the 10 mm (F = 4.01, p = 0.04), 15 mm (F = 5.21, p = 0.03), and 20 mm (F = 4.48, p = 0.04) radius of thresholds only in the second trial. However, there was no group difference on TIB at the first and third trials due to potential compensatory and/or adaptive reactions to avoid fall risks.
Conclusion
The LBP group lacked postural stability within the thresholds less than a 20 mm radius at the second trial of unilateral standing. The significant group interaction with the thresholds indicates an adaptation strategy on sway thresholds. This postural reaction from repeated trials should be considered with sway excursion adjustments and fall prevention in older adults with LB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older adults with low back pain (LBP) may demonstrate fall-related self-efficacy on postural control that could impact neurophysiological changes [1,2,3]. Fall-related injuries were reported in approximately 30% of adults 60 years of age or older [4,5,6]. These studies indicated that individuals with LBP may have serious functional consequences for balance deficits.
It has been reported that individuals with chronic LBP implement compensatory strategies in standing balance due to lower limb function [7, 8]. Clinicians utilize the unilateral standing test as one of the most valuable balance tests because it is widely considered to be cost-effective and feasible in clinical research settings [9, 10]. However, there is a lack of understanding on adaptations of dynamic balance performance during repeated unilateral standing trials between individuals with and without LBP.
Previous studies reported postural stability during unilateral standing to assess time-to-boundary of postural control [11,12,13]. This measure estimates the time required for the center of pressure (COP) to reach the boundary of sway excursions if it were to continue on its instantaneous trajectory. Although their results imply different aspects of postural control in unilateral standing, the results are limited to make a postural correction before the COP reaches the base of support [14, 15]. A meta-analysis also reported poor sensitivity of the COP spatial-based measures due to the overlooked temporal aspect of balance [14]. These results might be related to various factors, including small sample sizes, test conditions for the balance strategy with pain, and, more importantly, data analyses of sway excursions within the specific boundary.
A recent study reported setting boundaries to objectively analyze results for better accuracy in detecting postural deficits [16]. Our normalized stability analyses for the time-in-boundary (TIB) based on various thresholds may provide valid information for postural stability. A TIB analysis is a measurement to compute the total time percent which subjects keep the COP within the ‘hypothetical circle,’ which was used as various levels of threshold. This normalized relative stability time analysis in individuals with LBP may provide additional clinical insights for postural stability. Previous studies summarized that balance is impaired in individuals with chronic LBP; however, there is limited evidence regarding possible postural sway mechanisms [7, 17, 18]. It is critical to consider fall prevention strategies from repeated unilateral standing trials, which is an objective measure for the adaptability of postural stability in older adults with and without LBP.
There is a lack of understanding on adaptations of postural control with LBP within different thresholds of radius from the COP sway excursion during repeated trials of unilateral standing between individuals with and without LBP. Postural stability within the boundaries might be different when considering other individual characteristics, such as age, body mass index (BMI), and gender. Without controlling those confounding factors, the results could lead to limited generalizability of the outcome measures. Therefore, the purpose of this study was to compare the normalized stability within the sway excursion boundaries based on the TIB during three repeated unilateral limb standing trials between individuals with and without chronic LBP. It was hypothesized that the LBP group would demonstrate reduced performance of TIB at the 10 mm threshold following the first unilateral standing trial compared to the control group.
Methods
Participants
Subjects were recruited from the community through advertisement, and those subjects who met the study’s inclusion criteria received information about the study and signed a copy of the Institutional Review Board approved consent form. Subjects were eligible to participate if they were between 50 and 75 years of age and were right limb dominant; had consistent LBP for at least a 3-month duration prior to data collection; had no serious pathology, such as nerve root compromise, at the time of data collection; and had no conditions which would prevent them from unilateral standing.
Subjects were excluded from participation if they had a diagnosed psychological illness that might interfere with the study’s protocol; had overt neurological signs (sensory deficits or motor paralysis); or were pregnant. The anthropometric variations with age and BMI were considered when recruiting the control group. The dominant sides of the upper and lower limbs were applied in our study since previous reports confirmed them as confounding factors [19, 20].
Experimental procedures
During the consent process, each subject was given standardized procedures to measure the outcomes of the test during unilateral standing with and without visual input. The level of disability of the participants was measured by the ODI, which consists of 10 items regarding the degree of severity to which back (or leg) trouble has affected the ability to manage tasks in everyday life. The 10 sections cover pain with daily functions, and each item is rated on a 6-point scale; a higher score means higher level of disability [21].
Upon arrival at the lab, individual demographic data were collected. Participants were instructed to remove their footwear and to stand barefoot on the platform. Subjects wore a full-body safety harness system that imposed negligible resistance and protected them from any potential injuries if they completely lost their balance; however, the harness did not affect the subjects’ balance recovery or assist them in any way. The tension on the safety straps was adjusted so the straps were neither too slack nor too taught. The experimental protocol included subjects standing on the computer-controlled, motorized Bertec Balance Advantage® system, Computerized Dynamic Posturography with Immersion Virtual Reality (CDP-IVR), with their feet placed at a comfortable distance apart.
The medial malleolus of each foot of the subject was positioned over the blue horizontal line on the support surface, so that the ankle joint was aligned with the transverse rotational axis and the lateral side of the calcaneus. The y-axis indicated AP movements on the platform, while side-to-side movements on the support surface occurred along the x-axis. The dual force plates can rotate about the x-axis, which represents the transverse axis of the ankle joint. This position acts as a reference point for the calculation of sway angles.
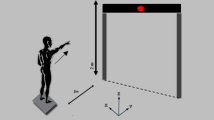
As shown in Fig. 1, the unilateral standing test was conducted with the Bertec® Balance System for postural stability during dominant limb standing. Each condition of the standardized procedure was demonstrated for the subjects. For example, each subject was asked to stand steady on the dominant foot for 10 s on the balance plate with his/her eyes open. The initial position included standing upright on the force plate with the contralateral hip and knee flexed to approximately 30 degrees. Though the subjects began each trial with their arms at their sides, compensatory arm movements were permitted to maintain balance.
The starting position of the unilateral standing test. Each subject was protected by a full-body safety harness and was instructed to remain on his/her dominant foot during the trial. Subjects were asked to stand barefoot on the dominant foot for 10 s, whilst flexing the contralateral knee at approximately 30° behind them and maintaining a vertical limb position to the standing limb. This balance test was performed with 10 s rest between trials
The force plate (Columbus, Ohio) was used to record the ground reaction forces (GRF) based on the Fx, Fy, and Fz, in orthogonal directions at a sampling frequency of 1000 Hz. The manufacturer calibrated the force plate, and a sensitivity matrix was provided to convert the voltages to forces and torques. The data was collected from the unloaded platform to determine the zero offset, and the balance changes imposed during unilateral limb stance balance tasks were utilized. Force plate data represented a combination of both disturbance and postural control reaction when subjects were engaged in a balance task typically employed to measure postural sway. The Bertec® force plates are the ‘gold standard’ for balance testing, and the plates have been shown to exhibit moderate to very high reliability across a range of postural sway measures [22]. All kinetic data were filtered using a fourth-order low-pass Butterworth filter with a 20 Hz cutoff frequency, and normalization was performed based on individual body weight.
All subjects were able to stand the requested time of 10 s during the test protocol. Regarding the kinetic data, the COP sway path lengths (mm) for the medial–lateral (ML) and anterior–posterior (AP) directions were compared. These parameters were independent of the effect of body weight, and those linear measures quantify the amount of variability in the data. Therefore, the COP refers to the point of application of the GRF vector, and it describes the organization of posture. The weighted sum of the time-varying position of the COP sway excursions during unilateral standing was calculated using the orthogonal forces and moments as recorded by the force plates. The ranges were analyzed by seven different levels of threshold (10 mm, 15 mm, 20 mm, 25 mm, 30 mm, 35 mm, and 40 mm) from the COP excursions (Fig. 2).
An example of the normalized stability time based on the threshold time-in-boundary (radius = 25 mm), which was drawn from the trajectory center for 10 s. A normalized stability time with COP was calculated during dominant limb standing on a platform. A First trial of the trajectory was plotted with the medio-lateral location as the x-axis and the anteroposterior location as the y-axis for a subject with LBP. Failing the unilateral standing task shows deviation from the center point (black dot) of the trajectory. The data points within the threshold circle were plotted as dark lines. B and C Second and third trials of the same subject. The trajectory of COP from the third trial stayed mostly within the threshold circle. D, E, and F Standing trial with a healthy subject. The first trial shows a moment out of the threshold circle; however, the second and third trials were all within the threshold circle. G The normalized stability time percent (relative time of trajectory staying within a threshold circle during 10 s standing) was calculated as a function of the threshold. The relative stability time increased as the threshold got bigger. The vertical dotted line is the example threshold (20 mm) used in A through F. The lower-case alphabet letters (a–f) correspond to each A–F. For example, subject A maintained standing posture for 18% of relative stability tolerance; however, subject C was able to maintain 85% of relative stability tolerance within the threshold in standing. The relative stability time within the thresholds decreased in a subject with LBP during the first trial. (LBP: low back pain, COP: center of pressure)
Statistical analysis
Preliminary power analyses were conducted based on the pilot data comparing groups, under the assumption of setting the type I error rate at 0.05. The mixed repeated measure ANOVA was utilized between groups to analyze any main and/or interaction effects on the dependent variables including observed power (or post-hoc power). This observed power is the statistical power of the test to estimate the power of a test given an observed effect size.
The effect sizes were also confirmed by partial eta-squared values (η2p) within a repeated measures analysis of variance (ANOVA) squared (small ≥ 0.01, medium ≥ 0.06, large ≥ 0.14), which was used to indicate the mean difference between groups with and without LBP. The mean difference between groups was analyzed by the Cohen’s d (d; small ≥ 0.2, medium ≥ 0.5, large ≥ 0.8). The demographic factors, such as age and BMI, were used as covariates if a group difference was revealed. Statistical analyses were completed using SPSS 26.0 (IBM Corp, Armonk NY, USA). For all statistical tests, the type I error rate was set at 0.05.
Results
As shown in Table 1, 26 subjects with LBP (16 female and 10 male) and 39 control subjects (20 female and 19 male) participated in the study. There was no significant group difference on gender (χ2 = 0.66, p = 0.41), age (t = − 1.31, p = 0.19), or BMI (t = 1.33, p = 0.18). The LBP group reported higher ODI (t = − 8.52, p = 0.001) scores than the control group.
As shown in Table 2, the TIB within the threshold boundaries was analyzed by the repeated measure ANOVA between groups with and without LBP. The groups demonstrated a significant interaction on thresholds (F = 8.76, p = 0.01, η2p = 0.10). The main effects of repeated trials (F = 4.21, p = 0.04, η2p = 0.06) and thresholds (F = 124.85, p = 0.001, η2p = 0.68) demonstrated significant differences. However, the groups did not demonstrate a significant interaction on repeated trials x thresholds (F = 0.11, p = 0.75, η2p = 0.01). The observed powers for trials (0.52), thresholds (1.00), and trials x thresholds (0.46) were warranted to establish statistical significance.
In Fig. 3, plots with separate lines were distributed for each subject during three repeated unilateral standing trials. The trends of TIB responses were similar across the trials within the group, and most subjects performed postural stability greater than 75% of the TIB radius at the 40 mm threshold level. During the second trial, however, the control group performed better within the TIB radius at 10 mm, 15 mm, and 25 mm than the LBP group. The LBP group demonstrated a significantly decreased TIB within the 10 mm (F = 4.01, p = 0.04, η2p = 0.06, d = 0.51), 15 mm (F = 5.21, p = 0.03, η2p = 0.07, d = 0.58), and 20 mm (F = 4.48, p = 0.04, η2p = 0.06, d = 0.54) radius of thresholds (Fig. 4). The results of Cohen’s d for 10 mm, 15 mm, and 20 mm were greater than 0.5, which indicated a medium difference of the group. However, other unilateral standing trials did not demonstrate group differences.
Plots with separate lines were distributed for each subject during three repeated unilateral standing trials. The trends of time-in boundary (TIB) responses were similar across the trials within the group. During the second trial, there were six subjects with low back pain (LBP) at 20 mm thresholds below 50% of TIB radius, while four control subjects were in the same TIB radius. At the 40 mm threshold level, most of the control group performed greater than 75% of TIB radius
The normalized stability time within the thresholds between groups during repeated unilateral standing. The sway ranges were analyzed by the seven different threshold levels [10 mm (A), 15 mm (B), 20 mm (C), 25 mm (D), 30 mm (E), 35 mm (F), and 40 mm (G)] from the COP. Although the groups did not demonstrate significant interactions on trials and thresholds (F = 0.11, p = 0.75), they demonstrated a significant interaction on thresholds (F = 8.76, p = 0.01). (*p < 0.05; LBP: low back pain, COP: center of pressure)
Discussion
Our study was conducted to compare the normalized stability based on the TIB during three repeated unilateral limb standing trials between subjects with and without chronic LBP. Our study might be the first investigation to provide quantified analyses for the TIB, which may provide clinical insights of postural stability within the specific boundary radius of thresholds. The results indicated that the groups demonstrated significant differences on the threshold less than the 20 mm radius at the second trial. However, no group difference was found at the first and third trials due to possible compensatory and/or adaptive reactions.
Clinicians have been utilizing the unilateral standing test as one of the most valuable balance tests because it is widely considered to be cost-effective and feasible in clinical research settings [9, 10]. A recent systematic review examined the unilateral standing test, which is associated with balance and fall risk in older adults, and reported that the evidence was commonly of low quality with inconsistent results [23]. Their reports indicated that the test is useful as a fall risk assessment tool to fill the crucial gaps in clinical settings. However, their review suggested interpreting the results with caution due to the lack of evidence level of each of the studies and conflicting results on sway excursion on dynamic postural reactions [23].
Our study hypothesized that the LBP group would demonstrate reduced performance of TIB at the 10 mm threshold following the first unilateral standing trial compared to the control group. We partially accepted the hypothesis; the LBP group lacked postural stability within the thresholds less than 20 mm radius at the second trial. It is important to provide reliable applications of unilateral standing to mimic the loss of balance on the force plate, which may reduce the gap between laboratory and real-life falls and potentially lead to fall-rate reductions in participants [24]. Although the LBP group demonstrated decreased normalized stability time across the trials and thresholds, the first trial did not differentiate the group difference due to novel experiences of the unilateral standing test.
Our TIB analysis within the thresholds may provide clinical insight on postural stability and spinal stabilization. This normalized relative stability provides better detection based on the various levels of threshold for sway excursions. The TIB counts only the data points within the threshold (distance from the mean value of COP during the test) without penalizing the sporadic sway during posture correction. Previous studies reported that higher stability of the lumbar spine might be due to a possible pain avoiding strategy from the standing limb [25,26,27], as the fallers demonstrated poorer body balance in the standing position than non-fallers [28]. Our sensitive measures on balance stabilities directly reflected minimizing sway excursions during unilateral standing. Thresholds less than the 20 mm radius at the second trial sensitively detected group differences due to spatiotemporal characteristics of postural control between groups with and without LBP.
Therefore, our analysis represents the amount of remaining COP within the specific threshold to stabilize corrective postural adjustments prior to reaching an increased radius of the thresholds during unilateral standing. The normalized stability differences on the various thresholds indicated trunk neuromuscular function, which is a valuable tool when assessing dynamic balance during unilateral standing [25, 26]. The difficulty of minimizing stability in the LBP group shed light on the clinical importance of the motor control subsystem, which interacts with the spinal musculature to stabilize the trunk to coordinate trunk and limb functions to protect against possible injuries and to allow the desired movements.
Although the time-to-boundary measure more adequately differentiates unilateral standing than path length analyses in AP and ML directions [16], the correlations between time-to-boundary and traditional measures were not sensitive to detect changes [11]. Our results of the TIB measure provide sensitive differences on the level of thresholds in older adults with and without LBP. A sensitive analysis for the TIB is a postural metric that links sway excursion and base of support to determine relative stability times in percentages.
The participants in our study with LBP demonstrated a moderate level of disability (25.62%), which was measured by the ODI tool; and our data ensured internal validity of controlled confounding factors. A recent secondary analysis reported that the improvements in self-efficacy and kinesiophobia following the intervention were individually associated with clinically important reductions in ODI scores [29]. The areas of improvement that help guide the course of evaluation, as well as reassess treatment progresses, concluded that balance assessments should be completed for older adults with chronic LBP [7, 8]. However, their study inclusion criteria started with worse baseline self-efficacy and higher kinesiophobia, which may change the association of their results with recovery among more impaired adults.
The subjects with LBP in our study demonstrated significant improvements in sway excursions in the ML and AP planes during repeated unilateral standing. Although our subjects with LBP reported a moderate level of dysfunction, their compensatory reactions on the second trial in the AP and ML planes were specific enough to evaluate decrements in dynamic stability. During the third trial of unilateral standing, there was no group difference due to the motor learning effect in the LBP group for the thresholds less than 20 mm. It was evident that the first trial effect with various responses did not demonstrate a group difference on their normalized stability. It would be possible to have a novel experience and delayed trunk reactions due to possible coordination problems relative to the lower limb muscles [30] as musculoskeletal pain in the LBP group depends on reconnecting the brain with the rest of the body [31].
Our results confirmed that there was no group difference on TIB at the first and third trials due to potential compensatory and/or adaptive reactions to avoid fall risks. The LBP group lacked postural stability within the thresholds less than a 20 mm radius at the second trial of unilateral standing. In general, if subjects can stay within threshold for TIB measurement with some variation or disturbance, it will be considered stable, while widely distributed COP without clear steady state point of COP will significantly penalize TIB results. At the second trial, the LBP group significantly reduced their stability on the sway boundaries (10 mm, 15 mm, and 20 mm). The subjects learned characteristics from the first trial of unilateral standing and adjusted their postural demand to minimize fall risks. More importantly, our normalized stability of TIB sensitively detected group differences, since TIB is the total time percent which subjects keep COP within a ‘hypothetical circle’ used as thresholds to determine posture control in standing. The TIB counts only the data points within threshold (distance from the mean value of COP during the test) without penalizing the sporadic sway during posture correction.
At the third trial, there was no group difference on the normalized stability. It might be possible to efficiently adjust the sway ranges from the repeated postural control in the LBP group. A clinical application of repeated trials is important to understand balance deficits and relevant features with different motor control strategies. It has been proposed that a persistent “tight control strategy” may be specifically targeted by reducing muscle excitability and co-contraction while increasing movement variability in motor control [32].
Our results were supported by these studies that the normalized stability times significantly decreased in the thresholds less than the 20 mm radius at the second unilateral standing trial. In addition, the successive COP measurements during repeated trials were clinically important to consider to examine compensatory mechanisms of balance. The significant group interaction with the thresholds indicates an adaptation strategy on sway thresholds. This postural reaction from repeated trials should be considered with sway excursion adjustments and fall prevention in older adults with LBP. These compensatory reactions warrant future investigations of causal interactions of repeated trials with motor control strategies using longitudinal study designs.
Our study has several limitations. The demographic variations might invalidate the results even though older adults with similar individual characteristics participated in the study. It would be beneficial to perform a validation analysis to ensure the sensitivity and reproducibility of the methodology in future studies. In addition, the subjects’ characteristics were not restricted based on postural deficits or fall episodes. There were subjects with standing posture and/or lower limb compensations during repeated unilateral trials. This postural reaction may have produced less accurate measures for each test, but our standardized procedure of measurements was a primary reason for conducting three trials for each condition. Further studies are warranted to improve postural equilibrium strategies to help dynamic balance and control while considering fall efficacy in older adults.
Conclusion
The LBP group lacked postural stability for less than 20 mm thresholds at the second trial of unilateral standing. The TIB analysis was sensitive to the threshold levels during the second trial in older adults with LBP. Our findings imply that the LBP group was able to adapt their sway excursions to improve their fall-related confidence with repeated unilateral standing.
Data availability
The data that support the findings of this study are not openly available due to the conditions of ethics approval for the study and current data protection legislation. Dependent on compliance with data protection legislation and ethical approval, they may be available from the corresponding author upon reasonable request.
References
Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S (2006) The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med 7:60–70
Ge L, Wang C, Zhou H, Yu Q, Li X (2021) Effects of low back pain on balance performance in elderly people: a systematic review and meta-analysis. Eur Rev Aging Phys Act 18:8
Hlaing SS, Puntumetakul R, Wanpen S, Boucaut R (2020) Balance control in patients with subacute non-specific low back pain, with and without lumbar instability: a cross-sectional study. J Pain Res 13:795–803
Muir SW, Berg K, Chesworth B, Klar N, Speechley M (2010) Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community-dwelling older adults: a prospective study. J Geriatr Phys Ther 33:165–172
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J et al (2021) Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw Open 4:e2138911
Beauchet O, Fantino B, Allali G, Muir SW, Montero-Odasso M, Annweiler C (2011) Timed up and go test and risk of falls in older adults: a systematic review. J Nutr Health Aging 15:933–938
Berenshteyn Y, Gibson K, Hackett GC, Trem AB, Wilhelm M (2019) Is standing balance altered in individuals with chronic low back pain? A Syst Rev Disabil Rehabil 41:1514–1523
da Silva RA, Vieira ER, Fernandes KBP, Andraus RA, Oliveira MR, Sturion LA et al (2018) People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil 40:1294–1300
Michikawa T, Nishiwaki Y, Takebayashi T, Toyama Y (2009) One-leg standing test for elderly populations. J Orthop Sci 14:675–685
Mancini M, Horak FB (2010) The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med 46:239–248
Hertel J, Olmsted-Kramer LC (2007) Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture 25:33–39
Peterson DS, Phan V, Richmond SB, Lee H (2021) Effects of dual-tasking on time-to-boundary during stance in people with PD: a preliminary study. Clin Biomech 88:105420
Hou ZC, Su T, Ao YF, Hu YL, Jiao C, Guo QW et al (2022) Arthroscopic modified Brostrom procedure achieves faster return to sports than open procedure for chronic ankle instability. Knee Surg Sports Traumatol Arthrosc 30:3570–3578
Arnold BL, De La Motte S, Linens S, Ross SE (2009) Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc 41:1048–1062
Song K, Burcal CJ, Hertel J, Wikstrom EA (2016) Increased visual use in chronic ankle instability: a meta-analysis. Med Sci Sports Exerc 48:2046–2056
Richmond SB, Dames KD, Shad JM, Sutherlin MA, Fling BW (2020) Setting boundaries: utilization of time to boundary for objective evaluation of the balance error scoring system. J Sports Sci 38:21–28
Meinke A, Maschio C, Meier ML, Karlen W, Swanenburg J (2022) The association of fear of movement and postural sway in people with low back pain. Front Psychol 13:1006034
Lascurain-Aguirrebena I, Newham D, Critchley DJ (2016) Mechanism of action of spinal mobilizations: a systematic review. Spine 41:159–172
Sung PS, Spratt KF, Wilder DG (2004) A possible methodological flaw in comparing dominant and nondominant sided lumbar spine muscle responses without simultaneously considering hand dominance. Spine 29:1914–1922
Promsri A, Haid T, Federolf P (2018) How does lower limb dominance influence postural control movements during single leg stance? Hum Mov Sci 58:165–174
Fairbank JC (2014) Oswestry disability index. J Neurosurg Spine 20:239–241
Moghadam M, Ashayeri H, Salavati M, Sarafzadeh J, Taghipoor KD, Saeedi A et al (2011) Reliability of center of pressure measures of postural stability in healthy older adults: effects of postural task difficulty and cognitive load. Gait Posture 33:651–655
Blodgett JM, Ventre JP, Mills R, Hardy R, Cooper R (2022) A systematic review of one-legged balance performance and falls risk in community-dwelling adults. Ageing Res Rev 73:101501
Ferreira RN, Ribeiro NF, Figueiredo J, Santos CP (2022) Provoking artificial slips and trips towards perturbation-based balance training: a narrative review. Sensors 22:9254
Sung PS, Leininger PM (2015) A kinematic and kinetic analysis of spinal region in subjects with and without recurrent low back pain during one leg standing. Clin Biomech 30:696–702
da Silva RA, Vieira ER, Leonard G, Beaulieu LD, Ngomo S, Nowotny AH et al (2019) Age- and low back pain-related differences in trunk muscle activation during one-legged stance balance task. Gait Posture 69:25–30
Sung PS, Yoon B, Lee DC (2010) Lumbar spine stability for subjects with and without low back pain during one-leg standing test. Spine 35:E753–E760
Ostrowska B, Giemza C, Wojna D, Skrzek A (2008) Postural stability and body posture in older women: comparison between fallers and non-fallers. Ortop Traumatol Rehabil 10:486–495
Maiers M, Forte ML (2021) Association between psychosocial parameters and response to chiropractic care among older adults with chronic low back pain: secondary analysis of a randomized clinical trial. J Manip Physiol Ther 44:675–682
Sung PS, Park MS (2023) Delayed response in rectus abdominis muscle following a step perturbation in subjects with and without recurrent low back pain. Eur Spine J 32:1842–1849
Langevin HM (2021) Reconnecting the brain with the rest of the body in musculoskeletal pain research. J Pain 22:1–8
van Dieen JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW (2019) Motor control changes in low back pain: divergence in presentations and mechanisms. J Orthop Sports Phys Ther 49:370–379
Acknowledgements
The authors thank the subjects at Indiana Wesleyan University as well as Dr. Phyllis Rowland, Matt Lavin and the students in the Doctoral Program in Physical Therapy for their technical assistance for data analyses and contributions to the study.
Funding
This study was supported by the Scholarship Council, Lilly Faculty Scholarship Award at Indiana Wesleyan University (2573877).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any financial or personal conflicts of interest in relation to the submission, other people, or any organizations.
Ethical approval
Ethics approval for the study was granted from the Indiana Wesleyan University Institutional Review Board (Project ID: (#1653.21; approval date: 12 October 2022). All study participants provided written informed consent to partake in the study. The study adhered to the Declaration of Helsinki on ethical principles for medical research involving human subjects.
Consent to participate
All subjects provided written, explicit, informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, D., Sung, P.S. Postural adaptations within normalized stability between older adults with and without chronic low back pain. Eur Spine J 32, 4420–4427 (2023). https://doi.org/10.1007/s00586-023-07939-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07939-3