Abstract
Purpose
Syringomyelia with coexisting intraspinal abnormities is thought to increase the risk of neurologic injury during surgical correction of the scoliosis. However, surgical treatment for intraspinal abnormities carries significant morbidity risks including worsening neurological function and wound complications. The authors’ aim in this study was to evaluate one-stage posterior correction of scoliosis in this patient population without prophylactic surgical treatment for neural axis malformations before scoliosis correction.
Methods
A total of 29 patients with syringomyelia and coexisting intraspinal abnormities who underwent scoliosis correction were evaluated. The average age was 15.6 years (range 12–23). All patients were examined for neural axis abnormalities using MRI, including syringomyelia with Chiari I malformation in 18 patients, syringomyelia with tethered cord and/or diastematomyelia in 11. None of patients presented with symptoms suggesting significant neurological dysfunction. The surgical efficacies and complications of correction were reviewed.
Results
The preoperative Cobb angle of major coronal curve averaged 65° (range 46°–95°), and it measured 28° (range 22°–43°) at the last follow-up, for a 63 % correction. Maximal kyphosis averaged 52° (range 41°–69°) preoperatively, and improved to 29° (range 22°–43°) at ultimate follow-up, for a 46 % correction. The average follow-up was 6 years (4–8 years). None of the patients experienced deterioration in their neurologic status.
Conclusion
The study results suggested that prophylactic neurosurgery for intraspinal abnormality may be unnecessary in patients with asymptomatic or minor symptomatic syringomyelia and coexisting intraspinal abnormities. One-stage posterior correction of scoliosis in this patient population does not involve significant complications and seems to be an alternative and safe treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the development of MRI, syringomyelia has been discovered with increasing frequency in patients with scoliosis. The concomitant rate of syringomyelia in scoliosis is 4–8 % [1–3]. Patients with syringomyelia often had multiple intraspinal abnormalities, such as Chiari malformation, diastematomyelia, and tethered cord [4]. To prevent potential neurologic complications, neural axis malformations need to be addressed before the treatment of scoliosis. Most surgeons agree that treatment of the neural axis malformations should be preceded because of the increased risk of neurologic deterioration during scoliosis correction [5, 6]. Many patients visit the hospital to undergo treatment for scoliosis as the presenting sign of otherwise asymptomatic neural axis abnormalities [7–9]. Charry et al. [2] showed that 15 (60 %) patients with scoliosis secondary to syringomyelia also had normal neurologic findings. Park et al. [10] mentioned that 38 (56 %) children with Chiari malformations had no detectable neurologic deficits and that 11 (16 %) children were neurologically asymptomatic except for scoliosis. There have been few studies for identifying the risk of neurologic complications as a result of scoliosis surgery in patients with asymptomatic or minor symptomatic syringomyelia with other intraspinal abnormities. In the current study, we have retrospectively analyzed 29 consecutive asymptomatic or minor symptomatic patients with syringomyelia and coexisting intraspinal abnormities undergoing scoliosis surgery without prophylactic treatment for neural axis abnormalities.
Methods
Twenty-nine patients—19 females and 10 males—with syringomyelia who underwent surgery for scoliosis were identified. The average age was 15.6 years (range 12–23 years). Eighteen of 29 patients were associated with Chiari I malformation, other eleven patients with tethered cord and/or diastematomyelia. None of these patients presented with significant neurological dysfunction. Nine patients (31 %) had only minor deficits such as increased deep tendon reflexes or asymmetric superficial abdominal reflexes. None of the patients had been operated for neural axis malformations. We performed SEP before surgery and intraoperative SEP was also applied in all patients and, additionally, wake-up test was applied. All surgeries were performed as a one-stage posterior procedure. AP radiograph and lateral radiograph of spine were performed postoperatively to get the message of deformity correction. The follow-up period was from the time of the scoliosis surgery until the last clinical review. The minimum follow-up was 4 years, average of 6 years (range 4–8 years) (Table 1).
Results
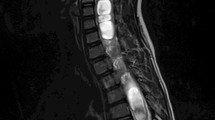
Radiographic measurements were made on AP and lateral radiographs of the spine by a single independent blinded reviewer (Figs. 1, 2, 3). The preoperative Cobb angle of major coronal curve averaged 65° (range 46°–95°), and it measured 28° (range 22°–43°) at the last follow-up, for a 63 % correction. Maximal kyphosis averaged 52° (range 41°–69°) preoperatively, and improved to 29° (range 22°–43°) at ultimate follow-up, for a 46 % correction. The correction loss at the end of follow-up was less than 10 % (Table 2).
There were not any changes in SEP during the surgery. None of the patients experienced deterioration in their neurologic status after surgery. At the follow-up, compared with preoperative situation, there was no difference in deep tendon reflexes or asymmetric superficial abdominal reflexes. There were no superficial or deep wound infections or pseudarthrosis during the follow-up visits.
Discussion
The pathophysiology of the development of scoliosis with syringomyelia has not been yet established. Mass effect in the fetal life, damage to or influence on the anterior and/or posterior horn cells or roots, and possible association with upper motor neuron signs have been suggested [11]. Neurologic signs of syringomyelia have been reported to be frequently minimal or absent in patients with syringomyelia, even with a very large syrinx. Scoliosis with syringomyelia has been characterized by rapid curve progression, juvenile or skeletally immature patients, and less rotation than would otherwise be expected [9].
The effect of neurosurgical treatment of the syrinx on scoliosis is not established. Many authors support syrinx drainage for neurologic improvement or stabilization, [2, 12] however, the effect of syrinx drainage on the scoliosis curve progression is still controversial. Some authors have reported stabilization or improvement of scoliosis after syrinx drainage [5], yet other authors have reported questionable or no effect of drainage on curve progression [13, 14]. Yeom et al. [15] reported that decompression of a syrinx in patients under the age of ten may decrease the curve size and limit scoliosis curve progression. However, in patients over the age of ten, surgical treatment of scoliosis was most likely necessary due to a large initial scoliosis curve or curve progression even after syrinx drainage.
Combination of two or more intraspinal abnormities often existed in patients with scoliosis with syringomyelia, such as Chiari malformation, diastematomyelia, and tethered cord [16]. These anomalies are often asymptomatic or minor symptomatic and may remain undetected until the patient is fully assessed following the diagnosis of congenital spinal deformity. Theoretically, the concurrent intraspinal abnormities can increase the risk of neurologic injury during surgical correction of the deformity. The advocated approach in such patients is first to perform surgery for the intraspinal pathologies and then surgery for correction and stabilization of the deformity, or simultaneous surgical treatment for congenital deformity and intraspinal abnormality [6, 17, 18]. However, performing surgery for the intraspinal pathologies in asymptomatic or minor symptomatic patients also carries some risk of morbidity including neurological deterioration and wound problems.
In recent years, some authors have investigated the feasibility of directly posterior or circumferential approach for scoliosis correction without suboccipital decompression in patients associated with syringomyelia and Chiari I malformation Satisfactory correction outcomes were achieved and no significant neurological deficits occurred [19]. Hui et al. [20] reported that neurosurgical interventions are recommended to patients with type 1 diastematomyelia before spinal deformity surgery; however, patients with type 2 diastematomyelia can be treated safely without a need of neurosurgical intervention. Our results suggest that neurosurgical treatment of neural axis malformation in asymptomatic or minor symptomatic patients with syringomyelia and coexisting diastematomyelia and/or tethered cord may be unnecessary before surgical correction of their scoliosis.
In conclusion, significant correction of scoliosis was achieved and there was no clinical evidence of neurological deficit in our series of 29 patients. Scoliosis surgery in such patients is safe when performed in conjunction with intraoperative spinal cord monitoring or wake-up tests. The main limitations of our study are its retrospective nature and relatively small sample size.
References
Arai S, Ohtsuka Y, Moriya H, Kitahara H, Minami S (1993) Scoliosis associated with syringomyelia. Spine 18:1591–1592
Charry O, Koop S, Winter R, Lonstein J, Denis F, Bailey W (1993) Syringomyelia and scoliosis: a review of twenty-five pediatric patients. J Pediatr Orthop 14:309–317
Maiocco B, Deeney VF, Coulon R, Parks PF Jr (1997) Adolescent idiopathic scoliosis and the presence of spinal cord abnormalities. Preoperative magnetic resonance imaging analysis. Spine 22:2537–2541
Shen J, Wang Z, Liu J, Xue X, Qiu G (2013) Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine 38:814–818
Sengupta DK, Dorgan J, Findlay GF (2000) Can hindbrain decompression for syringomyelia lead to regression of scoliosis? Eur Spine J 9:198–201
McMaster MJ (1984) Occult intraspinal anomalies and congenital scoliosis. J Bone Joint Surg Am 66:588–601
Emery E, Redondo A, Rey A (1997) Syringomyelia and Arnold Chiari in scoliosis initially classified as idiopathic: experience with 25 patients. Eur Spine J 6:158–162
Evans SC, Edgar MA, Hall-Graggs MA, Powell MP, Taylor BA, Noordeen HH (1996) MRI of ‘idiopathic’ juvenile scoliosis: a prospective study. J Bone Joint Surg Br 78:314–317
Lewonowski K, King JD, Nelson MD (1992) Routine use of magnetic resonance imaging in idiopathic scoliosis patients less than eleven years of age. Spine 17:109–116
Park JK, Gleason PL, Madsen JR, Goumnerova LC, Scott RM (1997) Presentation and management of Chiari malformation in children. Pediatr Neurosurg 26:190–196
Chuma A, Kitahara H, Minami S, Goto S, Takaso M, Moriya H (1997) Structural scoliosis model in dogs with experimental induced syringomyelia. Spine 22:589–595
Ghanem IB, Londono C, Delalande O, Dubousset JF (1997) Chiari I malformation associated with syringomyelia and scoliosis. Spine 22:1313–1318
Farley FA, Song KM, Birch JG, Browne R (1995) Syringomyelia and scoliosis in children. J Pediatr Orthop 15:187–192
Phillips WA, Hensinger RN, Kling TF Jr (1990) Management of scoliosis due to syringomyelia in childhood and adolescence. J Pediatr Orthop 10:351–354
Yeom JS, Lee CK, Park KW, Lee JH, Lee DH, Wang KC, Chang BS (2007) Scoliosis associated with syringomyelia: analysis of MRI and curve progression. Eur Spine J 16:1629–1635
Shen J, Wang Z, Liu J, Xue X, Qiu G (2013) Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine 38:814–818
Winter RB, Haven JJ, Moe JH, Lagaard SM (1974) Diastematomyelia and congenital spine deformities. J Bone Joint Surg Am 56:27–39
Hamzaoglu A, Ozturk C, Tezer M, Aydogan M, Sarier M, Talu U (2007) Simultaneous surgical treatment in congenital scoliosis and/or kyphosis associated with intraspinal abnormalities. Spine 32:2880–2884
Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Yang Z, Liu L, Lu N (2011) One-stage and posterior approach for correction of moderate to severe scoliosis in adolescents associated with Chiari I malformation: is a prior suboccipital decompression always necessary? Eur Spine J 20:1106–1113
Hui H, Tao HR, Jiang XF, Fan HB, Yan M, Luo ZJ (2012) Safety and efficacy of 1-stage surgical treatment of congenital spinal deformity associated with split spinal cord malformation. Spine 37:2104–2113
Conflict of interest
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Zx., Feng, Dx., Li, P. et al. Surgical treatment of scoliosis associated with syringomyelia with no or minor neurologic symptom. Eur Spine J 24, 1555–1559 (2015). https://doi.org/10.1007/s00586-014-3692-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3692-1