Abstract
Purpose
To evaluate the effectiveness of brace treatment in patients with Chiari malformation type 1 (CM-1) or syringomyelia associated scoliosis without neurosurgical intervention.
Methods
This was a retrospective case–control study. 34 CM-1 or syringomyelia (CMS) patients who received brace treatment without neurosurgical intervention were recruited. Another 68 matched patients with idiopathic scoliosis who received bracing served as the control group. The matching criteria included gender, age (± 1 years), Risser sign (± 1 grade), initial curve magnitude (± 5°), curve patterns and follow-up time (± 6 months). Patients who encountered curve progression and scoliosis surgery were compared between different groups.
Results
Until the last visit, 16 (47%) patients in CMS group and 18 (26%) patients in IS group occurred curve progression; 9 (26%) patients and 15 (22%) patients underwent scoliosis surgery, respectively. Compared to idiopathic scoliosis, patients with CMS-associated scoliosis had a significantly higher rate of curve progression (P = 0.038). However, no significant difference was observed between two groups regarding to the rate of surgery (P = 0.867). Patients with combined CM-1 and syringomyelia had a higher rate of surgery than patients with isolated CM-1 or syringomyelia (P = 0.049). The double major curve pattern was identified as the risk factor for curve progression.
Conclusion
Brace treatment is effective for CMS-associated scoliosis without neurosurgical intervention. Compared to idiopathic scoliosis, brace can provide similar prevention for scoliosis surgery in CMS patients, but slight or moderate curve progression may occur. Specifically, patients with combined CM-1 and syringomyelia should be followed closely with a higher expectation of curve progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brace or orthosis, as a noninvasive approach, had a long history in the treatment of scoliosis. For patients with adolescent idiopathic scoliosis (AIS), the effectiveness of brace treatment for delaying curve progression had been confirmed by randomized controlled trials [1]. For scoliosis derived from other etiologies, such as congenital or syndromic scoliosis, brace could also be used as a time-consuming method to delay the timing of surgery in clinical practices [2, 3].
Chiari malformation type 1 (CM-1), defined as the cerebellar tonsillar descent below the level of foramen magnum more than 5 mm, is frequently associated with syringomyelia and scoliosis in pediatrics. The reported incidence of scoliosis ranged from 13 to 36% in patients with CM-1 and was up to approximately 80% in patients with combined CM-1 and syringomyelia [4,5,6,7,8,9]. Scoliosis can also exist in patients with idiopathic syringomyelia, suggesting that isolated syringomyelia is another possible independent contributor to the pathogenesis of scoliosis [10, 11].
For patients with CM-1 or syringomyelia (CMS) associated scoliosis, Sha et al. found that brace was effective in preventing curve progression in majority of them, and its effectiveness was comparable with idiopathic scoliosis patients [12, 13]. Nevertheless, all patients in their studies had a history of prior neurosurgical intervention, such as posterior fossa decompression. The role of brace treatment in patients who didn’t receive neurosurgery had never been proved in literature.
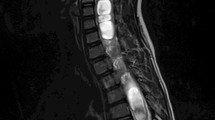
Due to no hindbrain-related symptoms, some CMS patients visited the outpatient clinic primarily for scoliosis. The diagnosis of CM-1 or syringomyelia was made by magnetic resonance imaging (MRI) due to physicians’ suspicion for underlying etiologies of scoliosis. These patients didn’t necessarily need a prophylactic neurosurgery after consulting neurosurgeons, and their curve magnitude of scoliosis didn’t reach the operation criteria as well. Thus, brace treatment could serve as a conservative strategy to prevent scoliosis progression. In this study, we aimed to evaluate the clinical outcome of brace treatment for CMS-associated scoliosis without any prior neurosurgical intervention and to compare its effectiveness with matched idiopathic scoliosis.
Materials and methods
Patient population
This is a retrospective case–control study. After institutional review board approval, we reviewed patients with CMS-associated scoliosis in outpatient clinic from 2005 to 2018. The informed consent was exempted because of the retrospective nature of this study. The following inclusion criteria for CMS patients were used in this study: (1) confirmed diagnosis of CM-1 or syringomyelia; (2) receiving brace treatment without prior neurosurgical intervention; (3) regular follow-up till skeletal maturity or scoliosis surgery. Patients who had other spinal disorders, incomplete clinical and radiographic data, poor compliance to brace or follow-up time less than 2 years were excluded from this study. 34 patients (CMS group) were finally enrolled (Fig. 1). Among them, 14 patients presented isolated CM-1, 12 patients presented isolated syringomyelia, and 8 patients presented combined CM-1 and syringomyelia.
Idiopathic scoliosis patients who received brace treatment during the same period were matched at a 2:1 ratio. The matching criteria included gender, age (± 1 years), Risser sign (± 1 grade), initial curve magnitude (± 5°), curve patterns and follow-up time (± 6 months). MRI was used to rule out any neural axis abnormality. In total, 68 patients (IS group), including 28 patients with juvenile idiopathic scoliosis and 40 patients with adolescent idiopathic scoliosis, were selected to serve as the control group.
Brace treatment
The indications for brace treatment for scoliosis were as followed: (1) skeletally immature patients with Risser sign 0–2; (2) curve magnitude ranging from 20° to 40° in adolescents; (3) curve magnitude exceeding 40° in patients younger than 10 years. Patients with curve progression to 50° or more after brace treatment will be recommended to scoliosis surgery.
The protocol of brace treatment was in accordance with previously studies [14]. All patients were prescribed a Boston brace. At first, patients were ordered to wear brace for at least 22 h every day. They were required to visit the outpatient clinic at an interval of 4–6 -months. At each appointment, the time of daily bracing was adjusted according to the changes of curve magnitude. If the main curve remained unchanged or progressed, the daily wearing time of brace was maintained at 22 h per day and would not decrease. If the main curve improved or Risser sign was larger than 3 or girls were more than 1 years after menarche, the daily wearing time of brace was shortened by 4 h per day. The brace also needed to be modified if curve pattern or patient’s body height changed greatly. Upon reaching skeletal maturity, patients could discontinue the brace treatment with a weaning process. The following indices indicated the skeletal maturity: no more than 1 cm increase in body height over last 6 months, at Risser sign 4 or 5 grades and two years post-menarche in girls.
At each visit, the actual time of daily bracing was recorded according to the information provided by the patients and confirmed by their parents. The compliance of bracing was calculated by actual hours of bracing divided by the total hours prescribed [15]. A compliance ratio of less than 75% is regarded as poor compliance and will be excluded from this study.
Clinical and radiographical assessments
The medical records of patients were reviewed at each visit, including age, menarcheal status, Risser sign, curve magnitude and curve pattern. Curve magnitude was measured on the out-of-brace standing full spine posteroanterior radiograph. A curve will be considered as no progression if the Cobb angle increased no more than 5° compared to the initial magnitude. Conversely, a 6° or more increase will be regarded as curve progression [16].
The diagnosis of CM-1 or syringomyelia was confirmed by MRI for evaluation of a possible cause of scoliosis. The distance between the tip of the cerebellar tonsil perpendicular to basion-opisthion line was more than 5 mm in all CM-1 patients [17]. All IS patients also underwent a routine MRI to rule out any neural axis abnormality.
Statistical analysis
Statistical analysis was performed with SPSS 22.0 statistical software (SPSS Inc., Chicago, IL). The independent t-test was used to compare continuous parameters between different groups. The chi-square test or Fisher's exact test was performed to compare categorical variables between different groups. The logistic regression analysis was performed to identify the risk factors for curve progression. A p value less than 0.05 was considered statistically significant.
Results
Patient population
Thirty-four CMS patients with scoliosis were included (15 male and 19 female). At the first visit, 15 female patients were premenstrual, and 4 were postmenstrual. The average age was 10.1 ± 3.1 years (range, 4–14 years). The Risser sign was Grade 0 in 29 patients (85%), Grade 1 in 3 patients (9%) and Grade 2 in 2 patients (6%). The average primary curve magnitude was 31.4° ± 7.5° (range, 20°–45°). Curve patterns were classified as follows: 19 thoracic curves, 8 double major curves and 7 thoracolumbar/lumbar curves.
Sixty-eight case-matched IS patients were enrolled at a 2:1 ratio, including 30 males and 38 females. The average age was 10.4 ± 2.7 years, and the average primary curve magnitude was 31.3° ± 6.3° at the first visit. A comparison of demographic and clinical characteristics was described in Table 1.
Effectiveness of brace treatment
The average duration of follow-up in CMS group and IS group was 4.3 ± 1.8 years (range, 2–10 years) and 4.1 ± 1.7 years (range, 2–9 years), respectively. At the latest follow-up, the mean curve magnitude was 37.0° ± 13.1° (range, 15°–65°) in CMS Group and 34.3° ± 12.2° (range, 10°-58°) in IS Group. A more than 5° increase in the Cobb angle of the major curve occurred in 16 (47%) patients in CMS group and 18 (26%) patients in IS group. Table 2 showed a comparison of bracing effectiveness between two groups. Compared to idiopathic scoliosis, patients with CMS-associated scoliosis had a significantly higher rate of curve progression after brace treatment (P = 0.038).
Of the patients who exhibited curve progression, 9 (26%) patients in CMS group and 15 (22%) patients in IS group had underwent scoliosis surgery prior to skeletal maturity because their curve magnitude exceeded 50°. Among the 9 patients who underwent scoliosis surgery in CMS group, 3 patients underwent scoliosis surgery directly, 5 patients underwent posterior fossa decompression, and 1 patient underwent syrinx drainage additionally. Regarding to the rate of progression to surgery, no significant difference was observed between two groups (P = 0.867).
Table 3 showed a comparison of bracing effectiveness between patients with three different pathologies. Curve progression was found in 5, 6 and 5 patients, respectively (Table 3), without statistically significant difference (P = 0.466). In addition, 2 patients with isolated CM-1, 2 patients with isolated syringomyelia and 5 patients with combined CM-1 and syringomyelia underwent surgical intervention. Patients with combined CM-1 and syringomyelia had a significantly higher rate of surgery (P = 0.049).
Risk factors for curve progression in patients with CMS-associated scoliosis
Curve progression was also evaluated in CMS group with respect to age, gender, curve magnitude and curve pattern at the time of brace prescription (Table 4). We found that the progression rates were similar between male and female patients. Patients who exhibited curve progression had younger ages (9.2 ± 3.5 years vs. 10.9 ± 2.5 years), larger curve magnitude (32.9° ± 8.2° vs. 29.9° ± 6.7°). On the basis of univariate analysis, the double major curve pattern was identified as the risk factor for curve progression by logistic regression analysis (P = 0.035).
Discussion
Recently, the natural history of CM-1 and syringomyelia in patients with no or mild neurological symptoms had been extensively investigated. Some experts recommended against prophylactic surgery for asymptomatic patients in a survey of pediatric neurosurgeons [18, 19]. Pomeraniec et al. [20] found that the overwhelming majority of CM-1 patients (92.9%) managed conservatively did not experience clinical or radiological progression. Whitson et al. [21] concluded that isolated CM-1 was not a radiologically static entity but rather was a dynamic one, and a reduction in tonsillar descent was substantially more common than an increase. For patients with combined CM-1 and syringomyelia, Nishizawa et al. [22] described nine cases who were monitored for 10 years or more and found that the long-term clinical courses of asymptomatic patients were benign with little evidence of neurological deterioration or syrinx propagation. Besides, Akhtar et al. [23] summarized approximately 30 patients with CM-1 and syringomyelia that resolved completely and spontaneously in the neurosurgical literature.
However, for patients with CMS-associated scoliosis who don’t need the prophylactic neurosurgery, the effectiveness of bracing had never been discussed, although brace treatment was widely used for skeletally immature patients who have a mild or moderate curve to prevent curve progression nowadays. Therefore, we analyzed the feasibility of brace treatment for these patients and compare its outcome with matched idiopathic scoliosis patients for the first time.
In our study, the average curve magnitude of patients with CMS-associated scoliosis increased moderately from 31.4° ± 7.5° to 37.0° ± 13.1° at final follow-up. The brace treatment was effective in 18 (53%) patients who had curve progression no more than 5°. Compared to idiopathic scoliosis patients, curve progression occurred more frequently and the rate of bracing failure was significantly higher in patients with CMS-associated scoliosis. Charry et al. [24] described 8 scoliotic patients with syringomyelia treated by brace treatment without neurosurgical decompression. They found that only one curve stabilized, and the other curves increased from 5° to 15° variously with an average follow-up of 3.7 years. Tokunaga et al. [25] reported the natural history of scoliosis in 27 children with syringomyelia and CM-1 and divided them into two groups according to the spontaneous reduction of syringomyelia. Five of 14 patients showed more than 5° improvement during the follow-up period in the patients whose syrinx was spontaneously reduced, while only 1 patient showed improvement among patients whose syrinx was unchanged. This suggests that solution of the neural axial abnormities may be associated with the improvement of scoliosis, but now there isn’t enough evidence to prove a causal link between them.
Although prevention for curve progression was less successful in CMS patients with scoliosis, only 9 (26%) patients reached the threshold for surgery, similar to the rate in IS patients (26% vs. 22%). Therefore, brace treatment was still effective for CMS patients without neurosurgical intervention and should be recommended to these patients (Fig. 2). Despite the development of modern implants and techniques, scoliosis correction surgery was still with risk of neurological complications, especially for CMS patients. Godzik et al. [26] compared the safety and outcomes of scoliosis surgery between patients with CM-1 associated scoliosis and a matched adolescent idiopathic scoliosis cohort. They found that CM-1 group had more neurological deficits (11% vs. 0%) and more neurophysiologic changes shown by neuromonitoring during surgery (28% vs. 3%) despite prior Chiari decompression intraoperative neuromonitoring. As a result, prevention of scoliosis surgery should be considered as the primary clinical outcome and slight or moderate curve progression after bracing might be acceptable. Thus, brace treatment was effective for CMS patients regrading to avoiding surgery when the prophylactic neurosurgical treatment was not necessary.
Our study also found that compared to isolated CM-1 or syringomyelia, patients with combined CM-1 and syringomyelia had higher risk of curve progression to surgery. Godzik et al. [27] found that patients with isolated CM-1 presented with fewer atypical curves features and less severe curve magnitude. They also reported that more patients with combined CM-1 and syringomyelia finally underwent a surgical intervention as compared to patients with CM-1 alone, which was consistent with our results. Zhu et al. [11] recognized that the maximal syrinx/spinal cord ratio and length of the syrinx was larger in CM-1 associated syringomyelia compared to idiopathic syringomyelia. Yan et al. [28] found that when compared with isolated CM-1, the clivus gradient was significantly flattened in combined CM-1 and syringomyelia, which was correlated with the severity of the syrinx. In brief, the different clinical outcomes may be associated with the different neurological pathology. Patients with both CM-1 and syringomyelia should be followed up regularly with a high suspicion of curve progression after brace treatment (Fig. 3).
A 12-year-old boy was diagnosed with combined Chiari malformation and syringomyelia. Initially, the proximal thoracic curve was 32°, and the thoracic curve was 37°. After 4 years of brace treatment, the proximal thoracic curve increased to 50° and the thoracic curve increased to 47°, which meets the threshold of surgery (A–C). A 12-year-old boy diagnosed with adolescent idiopathic scoliosis was matched to compare. The main thoracic curve was 38°, and the proximal thoracic curve was 33° at beginning. After 4 years of brace treatment, the main thoracic curve decreased to 26° finally (D–F)
Our results revealed that CMS patients with curve progression presented more incidence of double major curve pattern (P = 0.035). Sha et al. [12] drawn a similar conclusion in patients with CM-1 and syringomyelia following PFD. They found that patients with double major curves have a significant higher rate of bracing failure compared to patients with single thoracic curve (80% vs. 23%). It is worth mentioning that double major curve pattern is also thought as a predictor for curve progression in AIS patients. Katz et al. [16] found that AIS patients with a double curve pattern were significantly more likely to demonstrate curve progression after bracing. This phenomenon reflected the increased instability of double major curves, which was an intrinsic feature of scoliosis.
Several limitations should be mentioned. First, it is a retrospective study with the inherent risk of data inaccuracy. Second, radiographical parameters in MRI weren’t measured during follow-up, including the extent of tonsillar descent, the maximal syrinx/spinal cord ratio and the syrinx length. Therefore, the relationship between these parameters and curve progression remained further investigated. Third, this study included patients with a wide range of ages. Different ranges of age had different growth velocity, which may influence the effect of brace treatment. In addition, considering that scoliosis progression from CM-1 or syringomyelia was not always growth-dependent and may continue after skeletal maturity, longer follow-up into adulthood should be continued in future study. Finally, the exact values of compliance ratios were not analyzed and compared between different subgroups, which could have a potential influence on the effectiveness of bracing.
Conclusion
In summary, brace treatment is effective for CMS-associated scoliosis without neurosurgical intervention. Compared to idiopathic scoliosis, brace can provide similar prevention for scoliosis surgery in CMS patients, but slight or moderate curve progression may occur. Specifically, patients with combined CM-1 and syringomyelia should be followed closely with a higher expectation of curve progression.
References
Weinstein S, Dolan L, Wright J, Dobbs M (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521. https://doi.org/10.1056/NEJMoa1307337
Sponseller P, Bhimani M, Solacoff D, Dormans J (2000) Results of brace treatment of scoliosis in Marfan syndrome. Spine 25(18):2350–2354
Wang Y, Feng Z, Wu Z, Qiu Y, Zhu Z, Xu L (2019) Brace treatment can serve as a time-buying tactic for patients with congenital scoliosis. J Orthop Surg Res 14(1):194. https://doi.org/10.1186/s13018-019-1244-4
Eule J, Erickson M, O’Brien M, Handler M (2002) Chiari I malformation associated with syringomyelia and scoliosis: a twenty-year review of surgical and nonsurgical treatment in a pediatric population. Spine. https://doi.org/10.1097/00007632-200207010-00015
Ravindra V, Onwuzulike K, Heller R, Quigley R, Smith J, Dailey A, Brockmeyer D (2018) Chiari-related scoliosis: a single-center experience with long-term radiographic follow-up and relationship to deformity correction. J Neurosurg Pediatr 21(2):185–189. https://doi.org/10.3171/2017.8.Peds17318
Strahle J, Muraszko K, Kapurch J, Bapuraj J, Garton H, Maher C (2011) Chiari malformation Type I and syrinx in children undergoing magnetic resonance imaging. J Neurosurg Pediatr 8(2):205–213. https://doi.org/10.3171/2011.5.Peds1121
Strahle J, Smith B, Martinez M, Bapuraj J, Muraszko K, Garton H, Maher C (2015) The association between Chiari malformation Type I, spinal syrinx, and scoliosis. J Neurosurg Pediatr 15(6):607–611. https://doi.org/10.3171/2014.11.Peds14135
Tubbs R, Beckman J, Naftel R, Chern J, Wellons J, Rozzelle C, Blount J, Oakes W (2011) Institutional experience with 500 cases of surgically treated pediatric Chiari malformation Type I. J Neurosurg Pediatr 7(3):248–256. https://doi.org/10.3171/2010.12.Peds10379
Tubbs R, McGirt M, Oakes W (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 99(2):291–296. https://doi.org/10.3171/jns.2003.99.2.0291
Batzdorf U, Khoo L, McArthur D (2007) Observations on spine deformity and syringomyelia. Neurosurgery. https://doi.org/10.1227/01.Neu.0000279971.87437.1f
Zhu Z, Sha S, Chu W, Yan H, Xie D, Liu Z, Sun X, Zhu W, Cheng J, Qiu Y (2016) Comparison of the scoliosis curve patterns and MRI syrinx cord characteristics of idiopathic syringomyelia versus Chiari I malformation. Eur Spine J 25(2):517–525. https://doi.org/10.1007/s00586-015-4108-6
Sha S, Zhu Z, Sun X, Zheng X, Liu Z, Wu T, Yan H, Qiu Y (2013) Effectiveness of brace treatment of Chiari malformation-associated scoliosis after posterior fossa decompression: a comparison with idiopathic scoliosis. Spine 38(5):E299–E305
Sha S, Zhu Z, Lam T, Sun X, Qian B, Jiang J, Cheng J, Qiu Y (2014) Brace treatment versus observation alone for scoliosis associated with Chiari I malformation following posterior fossa decompression: a cohort study of 54 patients. Eur Spine J 23(6):1224–1231. https://doi.org/10.1007/s00586-014-3265-3
Qiu Y, Sun X, Cheng JC, Zhu F, Li W, Zhu Z, Wang B, Yu Y (2008) Bone mineral accrual in osteopenic and non-osteopenic girls with idiopathic scoliosis during bracing treatment. Spine. https://doi.org/10.1097/BRS.0b013e31817b5b9e
Wiley J, Thomson J, Mitchell T, Smith B, Banta J (2000) Effectiveness of the boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine. https://doi.org/10.1097/00007632-200009150-00010
Katz D, Durrani A (2001) Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine 26(21):2354–2361
Aboulezz A, Sartor K, Geyer C, Gado M (1985) Position of cerebellar tonsils in the normal population and in patients with Chiari malformation: a quantitative approach with MR imaging. J Comput Assist Tomogr 9(6):1033–1036. https://doi.org/10.1097/00004728-198511000-00005
Haroun R, Guarnieri M, Meadow J, Kraut M, Carson B (2000) Current opinions for the treatment of syringomyelia and chiari malformations: survey of the Pediatric Section of the American Association of Neurological Surgeons. Pediatr Neurosurg 33(6):311–317. https://doi.org/10.1159/000055977
Singhal A, Cheong A, Steinbok P (2018) International survey on the management of Chiari 1 malformation and syringomyelia: evolving worldwide opinions. Childs Nerv Syst 34(6):1177–1182. https://doi.org/10.1007/s00381-018-3741-x
Pomeraniec I, Ksendzovsky A, Awad A, Fezeu F, Jane J (2016) Natural and surgical history of Chiari malformation Type I in the pediatric population. J Neurosurg Pediatr 17(3):343–352. https://doi.org/10.3171/2015.7.Peds1594
Whitson W, Lane J, Bauer D, Durham S (2015) A prospective natural history study of nonoperatively managed Chiari I malformation: does follow-up MRI surveillance alter surgical decision making? J Neurosurg Pediatr 16(2):159–166. https://doi.org/10.3171/2014.12.Peds14301
Nishizawa S, Yokoyama T, Yokota N, Tokuyama T, Ohta S (2001) Incidentally identified syringomyelia associated with Chiari I malformations: is early interventional surgery necessary? Neurosurgery. https://doi.org/10.1097/00006123-200109000-00018
Akhtar O, Rowe D (2008) Syringomyelia-associated scoliosis with and without the Chiari I malformation. J Am Acad Orthop Surg 16(7):407–417. https://doi.org/10.5435/00124635-200807000-00006
Charry O, Koop S, Winter R, Lonstein J, Denis F, Bailey W (1994) Syringomyelia and scoliosis: a review of twenty-five pediatric patients. J Pediatr Orthop 14(3):309–317. https://doi.org/10.1097/01241398-199405000-00007
Tokunaga M, Minami S, Isobe K, Moriya H, Kitahara H, Nakata Y (2001) Natural history of scoliosis in children with syringomyelia. J Bone Joint Surg Br 83(3):371–376. https://doi.org/10.1302/0301-620x.83b3.11021
Godzik J, Holekamp T, Limbrick D, Lenke L, Park T, Ray W, Bridwell K, Kelly M (2015) Risks and outcomes of spinal deformity surgery in Chiari malformation, Type 1, with syringomyelia versus adolescent idiopathic scoliosis. Spine J 15(9):2002–2008. https://doi.org/10.1016/j.spinee.2015.04.048
Godzik J, Dardas A, Kelly M, Holekamp T, Lenke L, Smyth M, Park T, Leonard J, Limbrick D (2016) Comparison of spinal deformity in children with Chiari I malformation with and without syringomyelia: matched cohort study. Eur Spine J 25(2):619–626. https://doi.org/10.1007/s00586-015-4011-1
Yan H, Han X, Jin M, Liu Z, Xie D, Sha S, Qiu Y, Zhu Z (2016) Morphometric features of posterior cranial fossa are different between Chiari I malformation with and without syringomyelia. Eur Spine J 25(7):2202–2209. https://doi.org/10.1007/s00586-016-4410-y
Funding
This work was supported by the Jiangsu Provincial Key Medical Center (Grant No. YXZXA2016009) and the National Natural Science Foundation of China (Grant No. 81772304).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
The manuscript submitted does not contain information about medical device/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, T., Bao, H., Zhang, X. et al. Brace treatment for scoliosis secondary to chiari malformation type 1 or syringomyelia without neurosurgical intervention: A matched comparison with idiopathic scoliosis. Eur Spine J 30, 3482–3489 (2021). https://doi.org/10.1007/s00586-021-06958-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06958-2