Abstract
Citral is the main ingredient of the lemongrass plant with anti-inflammatory properties. In this study, the effects of citral on reducing inflammation in experimental diabetes in rats were investigated. Forty rats were randomly divided into four groups. There were two control groups (healthy controls (H) and citral alone-treated control (HC)) and two diabetic groups (diabetes (D) and diabetes+citral treatment (DC)). After diabetes confirmation on day 7, treatment with citral (300 mg/kg) was started for 2 weeks by gavage in the DC and HC groups. On days 0, 7, and 21 of the study, inflammatory elements of blood serum, IL-6, TNF-α, haptoglobin, and α2-macroglobulin were compared between the four groups. Also, on day 21 of the study, the expression level of IL-6 and TNF-α in the liver tissue was analyzed by quantitative real-time PCR. On day 21 of the study, following treatment with citral for 14 days, there was a significant difference in the DC group’s inflammatory factors compared to the D group (P < 0.005). However, no significant difference was observed in DC and the two control groups’ inflammatory factors. Regarding gene expression, the levels of IL-6 and TNF-α in the liver were significantly downregulated in the DC group compared to those in the D group (P < 0.05). According to the results of this study, citral can be used as a suitable ingredient to reduce the inflammatory complications of diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The metabolic condition described with hyperglycemia and the coincident glycosuria is known as diabetes mellitus (DM). In type 1 (T1) DM, the insulin secretion in the pancreatic islet is eliminated due to the decrease in the Langerhans pancreatic islet during a chronic autoimmune process (Yang et al. 2012). Besides, the latest reports have demonstrated a major role for the innate immune system and inflammatory mediators in T1DM pathogenesis (Eizirik et al. 2009). Complex inflammatory and immune mechanisms contribute to the onset of diabetes and its complications; therefore, suggesting an inflammatory basis for diabetes and its pathogenesis has been gaining new interest. Also, the inflammatory and oxidative stress markers increase concurrently with the progression of diabetes intricacies. Moreover, activation of various pathways appears to be important in the progression of diabetic complications, including the pathway of polyol, intermediate pathway of reactive oxygen, pathway of protein kinase C (PKC), and advanced glycation end product (AGE) pathway (Scott and King 2005). These signaling pathways give rise to inflammatory and oxidant responses, resulting in local and systemic tissue damage. During diabetes mellitus, the elevation in glucose and free fatty acids in serum leads to increased release of pro-inflammatory cytokines, PKC function regulation, and mitogen-activated protein kinase (MAPK) activity (King 2008).
The overexpression of pro-inflammatory cytokines and chemokines is another pathogenic pathway that exacerbates the complications of diabetes. Among these cytokines, there are some molecules, such as IL-6, IL-1, and TNF-α (Navarro et al. 2006), with high pro-inflammatory activity. Increased inflammatory activity is well recognized in type 1 diabetes patients with elevated CRP levels (Schalkwijk et al. 1999) and TNF-α (Schram et al. 2003). The liver is a major organ that is adversely affected by diabetes (Kobori et al. 2009). Haptoglobin (Hp) and α2-macroglobulin (α2-MG) are synthesized primarily in the liver and secreted into the plasma as acute-phase proteins. Haptoglobin is an important acute phase response (APR) that was investigated as an indicator of inflammation in rats and was observed to increase up to tenfold in response to stimuli in humans (Giffen et al. 2003). As a scavenger protein with anti-inflammatory and antioxidative properties, haptoglobin is an acute-phase protein that attaches hemoglobin and maintains the iron freed from hemoglobin (Ceron et al. 2005). α2-macroglobulin is another major acute-phase protein in rats (Kuribayashi et al. 2015).
Additionally, TNF-α, a multifunctional cytokine, seems to be closely related to metabolic disorders, cardiovascular risk factors, atherogenesis, and oxidative stress in diabetes patients. Several studies have indicated that the amount of TNF-α in the plasma increase in type 1 diabetes mellitus and that TNF-α is involved in the autoimmune process, which is associated with beta-cell damage and insulin resistance (Lechleitner et al. 2000; Pamir et al. 2009). However, the current limitations of anti-inflammatory drugs are adverse side effects, inadequate responsiveness, delivery problems, and high manufacturing cost. Accordingly, there has been considerable interest in exploiting novel anti-inflammatory factors with less toxicity and particular pharmacology. Plant essential oils have been used for a long time as treatments for inflammatory diseases in traditional medicine.
Cymbopogon citratus (DC) Stapf (lemongrass) belongs to the family Poaceae-Gramineae, an important source of ethnomedicines worldwide. Citral (3,7-dimethyl-2,6-octadienal) is the main constituent of Cymbopogon citratus and has been used in the cosmetic, perfumery, and pharmaceutical industries to control both fungal and bacterial pathogens (Guynot et al. 2003). Lemongrass tea has been widely used for antidyspeptic, antiseptic, antifever, tranquilizer, carminative, and stomachic properties (Barbosa et al. 2008). Lemongrass is a widely used herbal remedy due to its medicinal properties, particularly in Brazil and Southeast Asia. The essential oil or tea provided from lemongrass is commonly used for its anti-inflammatory and analgesic properties; however, further studies need to understand better the molecular mechanisms underlying these effects (Katsukawa et al. 2010).
Previous studies have also demonstrated that complications of diabetes are due to the increase in inflammatory factors (Rodríguez-Morán and Guerrero-Romero 1999; Navarro et al. 2006; Scott and King 2005). Lemongrass extract is among the rich polyphenolic compounds, which are secondary metabolites of plants with many beneficial properties, including anti-inflammatory effects (Carbajal et al. 1989; Figueirinha et al. 2008; González-Gallego et al. 2007; Francisco et al. 2011). As a newly discovered hepatoprotective agent, citral (C10H16O) is the main ingredient of lemongrass oil, and this component may reduce the side effects of diabetes complications. Citral has been used as an anti-inflammatory substance in several studies (Lertsatitthanakorn et al. 2006). However, no studies have tested citral’s anti-inflammatory impacts on the serum inflammatory parameters, including IL-6, TNF-α, haptoglobin, and α2-macroglobulin, and the gene expression of TNF-α and IL-6 in type 1 diabetes. In this research, we examined the anti-inflammatory function of citral in a type 1 diabetes rat model.
Materials and methods
Citral
Citral is the most important active ingredient of Cymbopogon citratus. It was provided from MERCK KGaA with an index number of 802489 and isomer purity (GC, area %) of ≥97.0% (a/a). This substance’s chemical formula is (CH3)2C = CHCH2CH2C (CH3) = CHCHO with a molecular weight of 152.23 g/mol. Some physicochemical properties of this compound are presented in Table 1.
Animals, induction of diabetes, and citral therapy
To perform this experimental study, 40 male Wistar rats (200 ± 12 g) were obtained from the Center of Laboratory Animals of the Faculty of Veterinary Medicine of Shahid Bahonar University, Kerman, Iran. The animals were kept in a temperature-regulated environment (at 23 ± 1 °C) with 12-h light/dark cycles and were fed standard rodent chow (Pars, Iran) and had free access to drinking water at all times. The rats experienced 7 days of acclimatization before the initiation of the experiment.
Forty rats were randomly assigned to four following groups: group 1, healthy control (H); group 2, citral alone-treated control (HC); group 3, diabetes (D); and group 4, diabetes+citral treatment (DC). Two groups were controls (H and HC). Two were diabetic groups (D and DC), in which diabetes was induced with two injections of streptozotocin (45 mg/kg body weight; Sigma, Germany), dissolved in 0.05 M citrate buffer, pH 4.5, immediately before use, with an interval of 24 h between them. To confirm the induction of diabetes, blood glucose level was measured by a glucometer (EasyGluco, South Korea) 5 days after the second injection. At this stage, the blood glucose level should be above 300 mg/dl to confirm the induction of diabetes (Chang et al. 2012). The day after diabetes confirmation (day 7), treatment with citral (300 mg/kg BW) was started in two groups (HC and DC) for 2 weeks by gavage. Corn oil was used as a vehicle for the delivery of citral to the HC and DC groups. In the other two groups (H and D), the corn oil was gavaged separately.
Serum biochemical assays
Blood samples were taken on days 0 (before the injection of streptozotocin), 7, and 21 from the rats in all four study groups and separated serum stored at − 20 °C until further use. The amount of glucose in the serum was quantified using glucose oxidase method kits (Pars Azmoon Co., Tehran, Iran) and a biochemical auto-analyzer (Alpha Classic AT++, Sanjesh, Iran). Serum insulin, IL-6, TNF-α, haptoglobin, and α2-macroglobulin were measured based on a quantitative sandwich enzyme immunoassay method using rat-specific ELISA kits (Shanghai Crystal Day Biotech, Shanghai, China).
The sensitivity of the insulin kit was 0.75 μIU/ml. The intra- and inter-assay precision of the insulin kit were CV < 8% and CV < 10%, respectively. The sensitivity of the IL-6 kit was 0.052 ng/L. The intra- and inter-assay precision of the IL-6 kit were CV < 8% and CV < 10%, respectively. The TNF-α kit’s sensitivity was 2.51 ng/L, and its intra- and inter-assay precision were CV < 8% and CV < 10%, respectively. The sensitivity of the haptoglobin kit was 0.22 μg/ml. The intra- and inter-assay precision of this kit were CV < 8% and CV < 10%, respectively. The sensitivity of the α2-macroglobulin kit was 0.21 μg/ml. The intra- and inter-assay precision of α2-macroglobulin kit were CV < 8% and CV < 10%, respectively.
Real-time PCR
The animals were euthanized with ether on day 21. The current study was conducted in compliance with the State Committee on Animal Ethics, Shiraz University, Shiraz, Iran (IACUC no: 468/63). The liver tissue was separated, homogenized in RiboEx™, and kept at − 70 °C until further analysis. Total RNA extraction was performed from 100 mg of liver tissue GeneAll® Hybrid-RTM total RNA isolation kit by RiboEx™ reagent (GeneAll, South Korea). Contaminating DNA from RNA samples was removed by treating RNA (1 μg) with DNase I (2 U/μl) for 1 h at 37 °C (GeneAll, South Korea). The extracted RNA’s quantity and purity were determined by absorbance at the wavelength of 260 nm using a NanoDrop spectrophotometer. Purity was estimated by the optical density (OD) OD260/OD280 ratio, and the samples with a ratio greater than 1.8 were used for the synthesis of cDNA. Reverse transcription was conducted using the PrimeScriptTM RT reagent kit with 1 μg of RNA and random hexamer primers according to the Kit instruction protocol (Takara, Japan). During cDNA synthesis, No-RT controls were also included in each experiment to check the genomic DNA contamination in real-time PCR. Relative quantitative analysis of target genes (IL6 and TNF-α) and an internal reference gene (GAPDH) was done using the real-time PCR system in a LightCycler 96 (Roche, Germany).
Specific sequences of PCR primers used in this study are listed in Table 2.
The final reaction volume for the study of gene expression was 20 μl, containing 4 μlq of EVAGreen™ qPCR Master mix (Solis BioDyne, Estonia), 0.4 μl of each primer (200 nM), 2 μl cDNA (~100 ng), and 13.2 μl nuclease-free water. The cycling conditions were one cycle of initial denaturation at 95 °C for 15 minutes, followed by 45 cycles of amplification (95 °C/15 sec, and 60 °C/30 sec). Reactions were done in triplicate. Each PCR run included a no-template control (NTC), consisting of PCR-grade water instead of the cDNA and No-RT controls. At the end of each run, a melting curve analysis was performed to assess amplification specificity. Standard curve analysis was carried out to confirm the assay, ensuring that the target and internal reference genes’ primers had similar amplification efficiencies. The experimental samples’ gene expression values were compared with those of the control samples based on the comparative 2−ΔΔCt method and using the REST2009 software (Qiagen, USA). The results were also subjected to analysis of variance (ANOVA), followed by the least significant differences (Tukey) test.
All qPCR analysis was performed according to the MIQE (Minimum information for publication of quantitative real-time PCR experiments) guidelines.
Statistical analysis
Statistical analysis was accomplished utilizing SPSS version 25. Descriptive statistics were presented as means ± SE. The means for each variable in the treatment groups and at various time points were compared using one-way analysis of variance, followed by the least significant differences (Tukey) test. Time, group, and their interaction were considered as fixed effects in the model. In all significant cases, the adjusted means were compared using Tukey’s test. The transformation of data was performed in the case of high variability and non-homogeneous variance. For most factors, the variance became homogenous after logarithmic transformation. A p value of less than 0.05 was considered statistically significant in all analyses.
Results
Results of factor analysis by ELISA
The following results were obtained from the data related to serum sampling’s three stages on days 0, 7, and 21.
Insulin
The results from comparisons between the groups showed that on day 0, there was no significant difference between the four groups in terms of insulin levels. On day 7 of the study, after the STZ injection and the development of diabetes in the D and DC groups, there was a significant difference between the H and HC groups compared with the D and DC groups. On the 21st day of the study, following treatment with citral in the HC and DC groups, there was a significant difference between the H and HC groups compared with the D and DC groups. All the changes observed in the serum insulin are shown in Fig. 1A.
A A comparison of serum insulin levels in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005. B A comparison of the mean fasting blood glucose levels in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005
Glucose
The results related to the serum glucose levels closely matched those related to the insulin levels, and no significant difference between the four groups could be observed on day 0. On days 7 and 21, there was a significant difference between the H and HC groups compared with groups D and DC in terms of serum glucose level. All the changes observed in the serum glucose are shown in Fig. 1B. One week after the streptozotocin injection, the fasting blood glucose level in the diabetic groups was greater than 300 mg/dl.
Inflammatory factors
The results related to the serum inflammatory factors, including IL-6, TNF-α, haptoglobin, and α2-macroglobulin, are presented below.
At day 0 of the study, no significant differences were observed between the four groups regarding inflammatory factors. On day 7 of the study, there was a significant difference between the control groups (H and HC) and the two diabetic groups (D and DC). On day 21, there was a significant difference between group D and groups H, HC, and DC. All the results related to the abovementioned parameters, i.e., IL-6, TNF-α, haptoglobin, and α2-macroglobulin, are demonstrated in Figs. 2A, B and 3A, B, respectively.
A A comparison of serum IL-6 levels in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005. B A comparison of serum TNF-α levels in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005
A A comparison of serum haptoglobin (HP) in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005. B A comparison of serum α2-macroglobulin (A2MG) in the diabetes (D), diabetes+citral treatment (DC), healthy control (H), and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.005
Real-time PCR
In the present study, the expression profiles of pro-inflammatory cytokines, including IL-6 and TNF-α, genes in the liver tissue of groups D, DC, and H on day 21 were measured, shown in Fig. 4A and B, respectively. The expression levels of IL-6 and TNF-α in the liver were upregulated in group D compared to those in group H (P < 0.05). However, the expression levels of IL-6 and TNF-α in the liver were significantly downregulated in the DC group in comparison with those in group D (P < 0.05) (Fig. 4A, B). Moreover, similar comparisons were made between the H and HC groups concerning the abovementioned genes. The findings revealed no significant difference between the mRNA expression levels of IL-6 and TNF-α (Fig. 5A, B).
A A comparison of IL-6 gene expression in the liver tissue of the diabetes (D), diabetes+citral treatment (DC), and healthy control (H) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.05. B A comparison of TNF-α gene expression in the liver tissue of the diabetes (D), diabetes+citral treatment (DC), and healthy control (H) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.05
A A comparison of IL-6 gene expression in the liver tissue of healthy control (H) and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.05. B A comparison of TNF-α gene expression in the liver tissue of the healthy control (H) and citral alone-treated control (HC) groups. Non-similar letters on each bar at each sampling day show significant differences at P < 0.05
Discussion
Management of diabetes and its complications are a growing concern worldwide (King 2008). Presently, it has been documented that inflammatory processes are involved in the development of diabetic complications. For instance, it was observed that the plasma concentrations of different inflammatory markers increased in diabetic patients (Pickup et al. 1997; Rodríguez-Morán and Guerrero-Romero 1999). Also, diabetic hyperglycemia and oxidative stress situations have been believed to cause the activation of the nuclear factor κB (NF-κB). They can generate many inflammation-regulated genes, such as pro-inflammatory cytokines, adhesion molecules, and growth factors (Chang et al. 2012). In the present study, citral’s anti-inflammatory effects, the major constituent of lemongrass essential oil, were examined in diabetic rats. To examine the mechanisms underlying citral effects, we explored serum pro-inflammatory cytokines (IL-6 and TNF-α), acute-phase proteins (haptoglobin and α2-macroglobulin), and cytokine gene expressions in the liver tissue (IL-6 and TNF-α). In this study, type 1 diabetes was induced by STZ injection. There was a significant increase in all examined inflammatory factors, including IL-6, TNF-α, haptoglobin, and α2-macroglobulin, on day 7 in the diabetic groups (D and DC) compared to the control groups (H and HC). In type 1 diabetes, the inflammatory response is a complex process, involving many signaling cascades. C-reactive protein is a major human acute-phase protein, while α2-macroglobulin is considered a typical acute-phase protein in rats (Kuribayashi et al. 2011). Haptoglobin is part of a practically heterogeneous group of proteins named positive acute-phase proteins, which are synthesized and secreted by liver cells, and their serum levels increase during the acute-phase response (Arambašić et al. 2012). Previous studies have proposed that interleukins IL-1 and IL-6 and tumor necrosis factor are the key inducers of acute-phase proteins in rats (Bauer et al. 1985; Jinbo et al. 2002). In humans, the plasma concentration of C-reactive protein was higher in diabetic patients than in patients in the healthy control group. Patients with diabetes type 1 experienced a considerable rise in fucosylated a1-acid glycoprotein’s proportional content, indicative of a chronic hepatic inflammatory response (Schalkwijk et al. 1999).
Lemongrass extract, which is among the rich polyphenolic compounds, has many beneficial properties, including anti-inflammatory effects (Figueirinha et al. 2008; González-Gallego et al. 2007). Because NF-B plays a crucial role in inflammation and its inhibition is one of the main approaches used to alleviate chronic inflammation, lemongrass extract, especially its polyphenol-rich fractions, is an encouraging source for the development of new anti-inflammatory agents (Lee et al. 2008; Lertsatitthanakorn et al. 2006).
In the present study, the inflammatory factors in the serum of the DC group, which were treated with citral for 14 days, were examined to evaluate citral’s effects on type 1 diabetes. The ELISA results showed a significant reduction in the measures of serum pro-inflammatory factors (IL-6 and TNF-α) in the treated diabetic (DC) group compared to those of the non-treated diabetic (D) group. Consistent with the ELISA results, the quantitative RT-PCR analysis showed a downregulation of inflammatory gene expression in the liver, confirming the serum assay results observed on day 21 (14 days after the administration of citral). The current study results indicated a significant decrease in the production of acute-phase proteins, including haptoglobin and α2-macroglobulin, in the liver in the DC group following gavage administration of citral and response to the decreased pro-inflammatory cytokines.
IL-6 stimulates the synthesis of acute-phase proteins by liver cells, and its gene transcripts are expressed in human atheromatous lesions (Saraheimo et al. 2003). The primary sources of IL-6 are a variety of cell types, such as muscle cells (Pedersen et al. 2001), adipocytes (Yudkin et al. 2000), hepatocytes, microglial cells, and astrocytes (Kamimura et al. 2003).
In the fasting state, the amounts of blood glucose were always significantly higher in the diabetic (D and DC) groups than in those of the control (H and HC) groups. Consistent with the fasting blood sugar results, serum insulin levels were lower in the diabetic (D and DC) groups compared to those in the control (H and HC) groups. However, the results showed that citral did not affect blood glucose in the fasting state and serum insulin in the diabetic groups. This herbal compound was found to induce the downregulation of inflammatory genes in the DC group.
In this study, to confirm the reduction of inflammation in the citral-treated diabetic (DC) group, the gene expressions of TNF-α and IL-6 in the liver, as one of the important tissues affected by diabetes complications, were examined. There was an increase in the gene expression of IL-6 and TNF-α in group D compared to that of group H. Also, no significant difference in IL-6 and TNF-α gene expression was observed between group DC and group H.
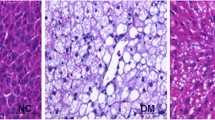
Diabetes is related to changes in the liver’s structure and function, resulting in hepatomegaly characterized by disproportional hypertrophy, hyperplasia, and apoptosis (Herrman et al. 1999). Our study’s findings indicate that the initiation of the inflammatory process in rats occurs in the early stages of diabetes development. This period is characterized by a significant increase in haptoglobin serum concentrations, suggesting that haptoglobin can be used as an early diabetes diagnostic marker. This suggestion agrees with the findings of Kruger et al. (2010), who detected elevated concentrations of serum haptoglobin before type 1 diabetes onset.
A more detailed study revealed that treating mice with lemongrass water extract reduced macrophages, thereby inhibiting the production of IL-1 and IL-6. Also, lemongrass essential oil was found to inhibit the same cytokines’ production by reducing macrophages in vitro (Sforcin et al. 2009).
Diabetic complications, such as ketosis, significantly increased hyperglycemia’s effects on the secretion of IL-6 by U937 monocytes in a cell culture model and type 1 diabetic patients (Jain et al. 2003). Elevated serum haptoglobin rates have been reported in people with diabetes and individuals with glucose intolerance (McMillan 1989). Increased serum levels of TNF-α and IL-6 during diabetes may indicate that these pro-inflammatory cytokines have dose-dependent effects on haptoglobin concentration, echoed by Baumann et al. (1989).
Similarly, Lechleitner et al. (2000) showed that TNF-α serum levels were significantly higher in patients with type 1 diabetes. The plasma amounts of TNF-α have been shown to have a strong positive association with HbA1c and fructosamine content. Likewise, experimental researches have shown that the mRNA expression of TNF-α has dramatically increased in diabetic rat kidneys compared to healthy rat kidneys (Navarro and Mora 2005). In type 1 diabetes, TNF-α is involved in the autoimmune process, which finally leads to beta-cell damage. The evidence for the involvement of TNF-α in insulin resistance was provided by the researches that showed the overexpression of TNF-α in the adipose tissue of obese animals. Insufficient insulin synthesis and subsequent chronic hyperglycemia lead to insulin resistance in type 1 diabetes (Lechleitner et al. 2000).
Furthermore, long-term and severe hyperglycemia in diabetes activates the p38 mitogen-activated protein (MAP) kinase pathway to increase the expression of the inflammatory IL-8 gene and enhance monocyte adhesion to the endothelium.
Upon phosphorylation on threonine and tyrosine, particular MAP kinases stimulate the mitogen-activated protein kinase p38. The p38 MAP kinase has an endothelial tissue signaling pathway which is enabled by stimuli including hyperglycemia, reactive oxygen species (ROS), which trigger stress, and pro-inflammatory cytokines, such as TNF-α (Surapisitchat et al. 2001). The activation of p38 activates other inflammatory signaling pathways and regulates the induction of inflammatory genes, including the nuclear factor B (NF-B) pathway and arachidonate-mediated survival signaling pathway (Evans et al. 2002). Previous data show that activated p38 induces actin cytoskeletal reorganization and leukocyte adhesion and migration (Rousseau et al. 1997). Thus, the onset of the p38 pathway in endothelial vessels induced by chronic high glucose could contribute significantly to the development of vascular complications of diabetes. A previous study also demonstrated that the p38 pathway was activated in the mouse endothelial cells during diabetes, suggesting that chronic elevated glucose in the serum could lead to p38 activation in endothelial tissue and promote monocyte/endothelial interactions observed in type 1 diabetes. The raised IL-8 formation due to chronic high glucose is mediated by p38 activation (Srinivasan et al. 2004). Our data agree with those studies that showed the anti-inflammatory properties of citral on cytokine production by murine macrophage culture (Bachiega and Sforcin 2011). Similarly, Uchida et al. (2017) revealed that consumption of citral (123–500 mg/kg) showed hepatoprotective effects against hepatocyte injury caused by acetaminophen-induced hepatic lesions during an experimental model. This hepatoprotective effect of citral can be attributed to either reducing oxidative stress following its treatment or its inhibitory effect on inflammatory events (Uchida et al. 2017). However, in the present study, the optimization dose of citral was not performed and the renal toxicity and hepatic toxicity of citral were not checked using biochemical and histopathological evaluation.
Conclusion
This research broadened citral’s possible application, as the main ingredient of the lemongrass plant, in inflammatory disorders. Moreover, the findings showed that the citral induced the downregulation of inflammatory genes and decreased related cytokines in diabetic rat serum. Based on these and other similar results and due to the growing worldwide interest in herbal remedies instead of chemicals, citral, an active ingredient in the lemongrass, can be used as a substance to reduce the inflammatory effects of type 1 diabetes. However, further biochemical and histopathological studies are necessary in detail to adjust the dose and evaluate the organ toxicity of citral.
Abbreviations
- H:
-
Group 1-healthy control
- HC:
-
Group 2-Citral alone-treated control
- D:
-
Group 3-Diabetes
- DC:
-
Group 4-Diabetes+citral treatment
- DM:
-
Diabetes mellitus
- BG:
-
Blood glucose
- T1DM:
-
Typ1 diabetes mellitus
- AGE:
-
Advanced glycation end product
- PKC:
-
Protein kinase C
- MAPK:
-
Mitogen-activated protein kinase
- TNF-α:
-
Tumor necrosis factor
- IL-6:
-
Interleukin 6
- α2-MG:
-
α2-Macroglobulin
- HP:
-
Haptoglobin
- LG:
-
Lemongrass
References
Arambašić J, Mihailovic M, Bogojevic D, Svetlana I-M, Uskokovic A, Goran P, Grigorov I (2012) Haptoglobin and the inflammatory and oxidative status in experimental diabetic rats: antioxidant role of haptoglobin. J Physiol Biochem 69:45–58. https://doi.org/10.1007/s13105-012-0186-7
Bachiega T, Sforcin J (2011) Lemongrass and citral effect on cytokines production by murine macrophages. J Ethnopharmacol 137:909–913. https://doi.org/10.1016/j.jep.2011.07.021
Barbosa LC, Pereira U, Martinazzo A, Maltha C, Teixeira R, Melo E (2008) Evaluation of the chemical composition of Brazilian commercial Cymbopogon citratus (D.C.) Stapf samples. Molecules (Basel, Switzerland) 13:1864–1874. https://doi.org/10.3390/molecules13081864
Bauer J, Weber W, Tran-Thi T-A, NorthofF G-H, Decker K, Gerok W, Heinrich PC (1985) Murine interleukin 1 stimulates α2-macroglobulin synthesis in rat hepatocyte primary cultures. FEBS Lett 190:271–274
Baumann H, Prowse K, Marinković S, Won KA, Jahreis G (1989) Stimulation of hepatic acute phase response by cytokines and glucocorticoidsa. Ann N Y Acad Sci 557:280–296
Carbajal D, Casaco A, Arruzazabala L, Gonzalez R, Tolon Z (1989) Pharmacological study of Cymbopogon citratus leaves. J Ethnopharmacol 25:103–107. https://doi.org/10.1016/0378-8741(89)90049-4
Ceron J, Eckersall D, Martinez-Subiela S (2005) Acute phase proteins in dogs and cats: current knowledge and future perspectives. Veterinary Clinical Pathology/American Society for Veterinary Clinical Pathology 34:85–99. https://doi.org/10.1111/j.1939-165X.2005.tb00019.x
Chang C-C, Chang C-Y, Huang JP, Hung L-M (2012) Effect of resveratrol on oxidative and inflammatory stress in liver and spleen of streptozotocin-induced type 1 diabetic rats. The Chinese Journal of Physiology 55:192–201. https://doi.org/10.4077/CJP.2012.BAA012
Deng Z, Wang Y, Zhou L, Shan Y, Tan S, Cai W, Liao S, Peng L, Lu Z (2017) High salt-induced activation and expression of inflammatory cytokines in cultured astrocytes. Cell Cycle 16:785–794. https://doi.org/10.1080/15384101.2017.1301330
Eizirik DL, Colli ML, Ortis F (2009) The role of inflammation in insulitis and β-cell loss in type 1 diabetes. Nat Rev Endocrinol 5:219–226. https://doi.org/10.1038/nrendo.2009.21
Evans JL, Goldfine ID, Maddux BA, Grodsky GM (2002) Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev 23:599–622
Figueirinha A, Paranhos A, Pérez-Alonso J, Santos-Buelga C, Batista M (2008) Cymbopogon citratus leaves: characterization of flavonoids by HPLC–PDA–ESI/MS/MS and an approach to their potential as a source of bioactive polyphenols. Food Chemistry - FOOD CHEM 110:718–728. https://doi.org/10.1016/j.foodchem.2008.02.045
Francisco V, Figueirinha A, Neves BM, García-Rodríguez C, Lopes MC, Cruz MT, Batista MT (2011) Cymbopogon citratus as source of new and safe anti-inflammatory drugs: bio-guided assay using lipopolysaccharide-stimulated macrophages. J Ethnopharmacol 133:818–827
Giffen P et al (2003) Markers of experimental acute inflammation in the Wistar Han rat with particular reference to haptoglobin and C-reactive protein. Arch Toxicol 77:392–402. https://doi.org/10.1007/s00204-003-0458-7
González-Gallego J, Sánchez-Campos S, Tuñón M (2007) Propiedades antiinflamatorias de los flavonoides de la dieta. Nutr Hosp 22:287–293
Guynot M, Ramos A, Setó L, Purroy P, Marín S (2003) Antifungal activity of volatile compound generated by essential oils against fungi commonly causing deterioration of bakery products. J Appl Microbiol 94:893–899. https://doi.org/10.1046/j.1365-2672.2003.01927.x
Herrman C, Sanders RA, Klaunig J, Schwarz L, Watkins J (1999) Decreased apoptosis as a mechanism for hepatomegaly in streptozotocin-induced diabetic rats. Toxicological Sciences: an Official Journal of the Society of Toxicology 50:146–151. https://doi.org/10.1093/toxsci/50.1.146
Jain S, Kannan K, Lim G, Greer J, McVie R, Bocchini J (2003) Elevated blood interleukin-6 levels in hyperketonemic type 1 diabetic patients and secretion by acetoacetate-treated cultured U937 monocytes. Diabetes Care 26:2139–2143. https://doi.org/10.2337/diacare.26.7.2139
Jinbo T, Sakamoto T, Yamamoto S (2002) Serum 2-macroglobulin and cytokine measurements in an acute inflammation model in rats. Lab Anim 36:153–157. https://doi.org/10.1258/0023677021912433
Kamimura D, Ishihara K, To H (2003) IL-6 signal transduction and its physiological roles. Rev Physiol Biochem Pharmacol 149:1–38. https://doi.org/10.1007/s10254-003-0012-2
Katsukawa M, Nakata R, Takizawa Y, Hori K, Takahashi S, Inoue H (2010) Citral, a component of lemongrass oil, activates PPARα and γ and suppresses COX-2 expression. Biochim Biophys Acta 1801:1214–1220. https://doi.org/10.1016/j.bbalip.2010.07.004
Khan H, Abdelhalim M, Alhomida A, Al-Ayed M (2013) Effects of naked gold nanoparticles on proinflammatory cytokines mRNA expression in rat liver and kidney. Biomed Res Int 2013:590730–590736. https://doi.org/10.1155/2013/590730
King GL (2008) The role of inflammatory cytokines in diabetes and its complications. J Periodontol 79:1527–1534. https://doi.org/10.1902/jop.2008.080246
Kobori M, Masumoto S, Akimoto Y, Takahashi Y (2009) Dietary quercetin alleviates diabetic symptoms and reduces streptozotocin-induced disturbance of hepatic gene expression in mice. Mol Nutr Food Res 53:859–868. https://doi.org/10.1002/mnfr.200800310
Kruger A et al. (2010) Haptoglobin as an early serum biomarker of virus-induced autoimmune type 1 diabetes in biobreeding diabetes resistant and LEW1.WR1 rats. Experimental Biology and Medicine (Maywood, NJ) 235:1328-1337 doi:https://doi.org/10.1258/ebm.2010.010150
Kuribayashi T, Tomizawa M, Seita T, Tagata K, Yamamoto S (2011) Relationship between production of acute-phase proteins and strength of inflammatory stimulation in rats. Lab Anim 45:215–218. https://doi.org/10.1258/la.2011.010112
Kuribayashi T, Seita T, Momotani E, Yamazaki S, Hagimori K, Yamamoto S (2015) Elimination half-lives of acute phase proteins in rats and beagle dogs during acute inflammation. Inflammation 38:1401–1405. https://doi.org/10.1007/s10753-015-0114-4
Lechleitner M, Koch T, Herold M, Dzien A, Hoppichler F (2000) Tumour necrosis factor-alpha plasma level in patients with type 1 diabetes mellitus and its association with glycaemic control and cardiovascular risk factors. J Intern Med 248:67–76. https://doi.org/10.1046/j.1365-2796.2000.00705.x
Lee HJ, Jeong HS, Kim DJ, Noh YH, Yuk DY, Hong JT (2008) Inhibitory effect of citral on NO production by suppression of iNOS expression and NF-κB activation in RAW264.7 cells. Arch Pharm Res 31:342–349. https://doi.org/10.1007/s12272-001-1162-0
Lertsatitthanakorn P, Taweechaisupapong S, Aromdee C, Khunkitti W (2006) In vitro bioactivities of essential oils used for acne control. Int J Aromather 16:43–49. https://doi.org/10.1016/j.ijat.2006.01.006
McMillan DE (1989) Increased levels of acute-phase serum proteins in diabetes. Metabolism-Clinical and Experimental 38:1042–1046
Navarro JF, Mora C (2005) Role of inflammation in diabetic complications. Nephrol Dial Transplant 20:2601–2604. https://doi.org/10.1093/ndt/gfi155
Navarro J, Milena F, Mora C, León C, Garcia J (2006) Renal pro-inflammatory cytokine gene expression in diabetic nephropathy: effect of angiotensin-converting enzyme inhibition and pentoxifylline administration. Am J Nephrol 26:562–570. https://doi.org/10.1159/000098004
Pamir N, McMillen T, Kaiyala K, Schwartz M, LeBoeuf R (2009) Receptors for tumor necrosis factor-α play a protective role against obesity and alter adipose tissue macrophage status. Endocrinology 150:4124–4134. https://doi.org/10.1210/en.2009-0137
Pedersen B, Steensberg A, Schjerling P (2001) Muscle-derived interleukin-6: possible biological effects. J Physiol 536:329–337. https://doi.org/10.1111/j.1469-7793.2001.0329c.xd
Perrault D et al (2020) Ischemia and reperfusion injury in superficial inferior epigastric artery-based vascularized lymph node flaps. PLoS One 15:e0227599. https://doi.org/10.1371/journal.pone.0227599
Pickup JC, Mattock MB, Chusney GD, Burt D (1997) NIDDM as a disease of the innate immune system: association of acute-phase reactants and interleukin-6 with metabolic syndrome X. Diabetologia 40:1286–1292. https://doi.org/10.1007/s001250050822
Rodríguez-Morán M, Guerrero-Romero F (1999) Increased levels of C-reactive protein in noncontrolled type II diabetic subjects. J Diabetes Complicat 13:211–215. https://doi.org/10.1016/S1056-8727(99)00047-1
Rousseau S, Houle F, Landry J, Huot J (1997) p38 MAP kinase activation by vascular endothelial growth factor mediates actin reorganization and cell migration in human endothelial cells. Oncogene 15:2169–2177
Saraheimo M, Teppo AM, Forsblom C, Fagerudd J, Groop PH, on behalf of the FinnDiane Study G (2003) Diabetic nephropathy is associated with low-grade inflammation in type 1 diabetic patients. Diabetologia 46:1402–1407. https://doi.org/10.1007/s00125-003-1194-5
Schalkwijk CG, Poland DCW, van Dijk W, Kok A, Emeis JJ, Dräger AM, Doni A, van Hinsbergh VWM, Stehouwer CDA (1999) Plasma concentration of C-reactive protein is increased in type I diabetic patients without clinical macroangiopathy and correlates with markers of endothelial dysfunction: evidence for chronic inflammation. Diabetologia 42:351–357. https://doi.org/10.1007/s001250051162
Schram M, Chaturvedi N, Schalkwijk C, Giorgino F, Ebeling P, Fuller J, Stehouwer C (2003) Vascular risk factors and markers of endothelial function as determinants of inflammatory markers in type 1 diabetes. The EURODIAB Prospective Complications Study Diabetes Care 26:2165–2173. https://doi.org/10.2337/diacare.26.7.2165
Scott J, King G (2005) Oxidative stress and antioxidant treatment in diabetes. Ann N Y Acad Sci 1031:204–213. https://doi.org/10.1196/annals.1331.020
Sforcin JM, Amaral JT, Fernandes A, Sousa JPB, Bastos JK (2009) Lemongrass effects on IL-1β and IL-6 production by macrophages. Nat Prod Res 23:1151–1159. https://doi.org/10.1080/14786410902800681
Srinivasan S, Bolick DT, Hatley ME, Natarajan R, Reilly KB, Yeh M, Chrestensen C, Sturgill TW, Hedrick CC (2004) Glucose regulates interleukin-8 production in aortic endothelial cells through activation of the p38 mitogen-activated protein kinase pathway in diabetes. J Biol Chem 279:31930–31936. https://doi.org/10.1074/jbc.M400753200
Surapisitchat J, Hoefen RJ, Pi X, Yoshizumi M, Yan C, Berk BC (2001) Fluid shear stress inhibits TNF-α activation of JNK but not ERK1/2 or p38 in human umbilical vein endothelial cells: Inhibitory crosstalk among MAPK family members. Proc Natl Acad Sci 98:6476–6481. https://doi.org/10.1073/pnas.101134098
Uchida NS., Silva-Filho SE, Cardia G F E, Cremer E, Silva-Comar FMDS, Silva EL et al. (2017) Hepatoprotective effect of citral on acetaminophen-induced liver toxicity in mice. Evidence-Based Complementary and Alternative Medicine, 2017.
Xie X, Luo X, Liu N, Li X, Lou F, Zheng Y, Ren Y (2017) Monocytes, microglia, and CD200-CD200R1 signaling are essential in the transmission of inflammation from the periphery to the central nervous system. J Neurochem 141:222–235. https://doi.org/10.1111/jnc.13972
Yang H et al. (2012) Long-term streptozotocin-induced diabetes in rats leads to severe damage of brain blood vessels and neurons via enhanced oxidative stress. Molecular Medicine Reports 7 doi:https://doi.org/10.3892/mmr.2012.1227
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 148:209–214. https://doi.org/10.1016/S0021-9150(99)00463-3
Zhang T-G et al (2015) All-trans-retinoic acid inhibits chondrogenesis of rat embryo hindlimb bud mesenchymal cells by downregulating p53 expression. Mol Med Rep 12:210–218. https://doi.org/10.3892/mmr.2015.3423
Funding
Funding was provided by the Shiraz University, Shiraz, Iran (grant number 97GCU2M143807).
Author information
Authors and Affiliations
Contributions
Maryam Hadadipour Zarandi developed the hypothesis and performed the literature search. Hassan Sharifiyazdi, Saeed Nazifi, and Maryam Hadadipour Zarandi contributed to the design and conceptualized the experiments described. Maryam Hadadipour Zarandi and Mahsa Khosravi Bakhtyari conducted the experiments. Maryam Hadadipour Zarandi performed the data acquisition. Hassan Sharifiyazdi, Mehran Ghaemi, and Maryam Hadadipour Zarandi analyzed the data. Maryam Hadadipour Zarandi wrote the manuscript. Saeed Nazifi, Hassan Sharifi Yazdi, and Mehran Ghaemi carried out a thorough analysis of the text and decided to publish the final edition.
Corresponding author
Ethics declarations
Ethics approval
The current study was conducted in compliance with the State Committee on Animal Ethics, Shiraz University, Shiraz, Iran (IACUC no: 4687/63). The European Council guidelines Directive (86/609/EC) of November 24, 1986, on animal protection used for scientific and other experimental purposes have also been taken into account.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zarandi, M.H., Sharifiyazdi, H., Nazifi, S. et al. Effects of citral on serum inflammatory factors and liver gene expression of IL-6 and TNF-alpha in experimental diabetes. Comp Clin Pathol 30, 351–361 (2021). https://doi.org/10.1007/s00580-021-03205-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-021-03205-4