Abstract
Although body temperature is a classic primary vital sign, its value has received little attention compared with the others (blood pressure, heart rate, and respiratory rate). This may result from the fact that unlike the other primary vital signs, aging and diseases rarely affect the thermoregulatory system. Despite this, when humans are exposed to various anesthetics and analgesics and acute etiologies of non-infectious and infectious diseases in perioperative and intensive care settings, abnormalities may occur that shift body temperature up and down. A recent upsurge in clinical evidence in the perioperative and critical care field resulted in many clinical trials in temperature management. The results of these clinical trials suggest that aggressive body temperature modifications in comatose survivors after resuscitation from shockable rhythm, and permissive fever in critically ill patients, are carried out in critical care settings to improve patient outcomes; however, its efficacy remains to be elucidated. A recent, large multicenter randomized controlled trial demonstrated contradictory results, which may disrupt the trends in clinical practice. Thus, updated information concerning thermoregulatory interventions is essential for anesthesiologists and intensivists. Here, recent controversies in therapeutic hypothermia and fever management are summarized, and their relevance to the physiology of human thermoregulation is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothermic animals (e.g., mammals and birds) regulate body temperature by balancing heat loss and heat production. The thermoregulatory center (anterior hypothalamus) maintains a narrow temperature range and asymmetrically adjusts temperature to the upper limit of survival, which is generally determined by the irreversible denaturation of enzymes and structural proteins [1]. Compared with other mammals, humans have an especially high defensive capacity against heat through autonomic thermoregulation of skin blood flow and perspiration. In humans, maximal skin blood flow increases to approximately 50 % of the cardiac output under excessive environmental heat stress, mainly by the cutaneous active vasodilator system. The maximal perspiration rate of the human eccrine sweat apparatus exceeds 3 L/h. Its primary purpose is for cooling [2–4].
Advantages of maintaining a higher body temperature include increased immune function and a greater exercise capacity from enhanced nerve conduction velocity and muscle contractions. However, disadvantages include a heat production requirement of ≳75 % of the chemical energy in foods, necessitating greater food consumption to maintain body temperature [5–8]. Mammals appeared on Earth approximately 60 million years ago when the climate was tropical or subtropical worldwide. Homeothermic mammals are thought to have adjusted and survived by maintaining physical activity during subsequent cyclic glacial environmental changes [6]. Although the normal body temperature of a mammal is determined by the climatic temperature when they first appeared on Earth, a recent unique study showed that optimal core temperature can be calculated as approximately 36.7 °C from the trade-off between bacterial propagation from hypothermia and increased metabolic cost from hyperthermia [9].
Over the past two decades, there have been studies showing changes in patient outcomes by actively or passively modulating human thermoregulation in the perioperative and critical care field. This review aims to highlight the two controversial topics of therapeutic hypothermia and fever management in critical care.
Therapeutic hypothermia
Clinical relevance of hypothermia
Recently, physicians have focused on the beneficial effects of brain protection from hypothermia. The Greek physician Hippocrates advocated packing wounded soldiers in ice and snow to control bleeding as early as 400 BC. Dominique Jean Larrey, surgeon-in-chief of the Napoleonic armies, used therapeutic hypothermia to both preserve injured limbs and relieve pain during amputation, and noted that wounded officers who kept closer to a fire for rapid rewarming experienced increased mortality [10]. The first scientific report on the clinical use of hypothermia was published in 1945. Fay treated patients who suffered severe head trauma with deep hypothermia (28 °C); the outcomes were positive, although several patients died from arrhythmia and sepsis [11]. In the 1950s, hypothermia was utilized to create a bloodless field in cerebral aneurysm surgery [12].
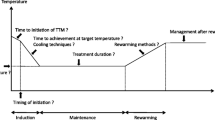
Sudden cardiac death represents a major health problem. The overall survival rate for out-of-hospital cardiac arrest in adults is approximately 10 %, and approximately 20 % for in-hospital cardiac arrest. Major causes of mortality are post-resuscitation brain injury and myocardial infarction [13]. More than a decade ago, randomized controlled studies from Australia and Europe demonstrated that therapeutic hypothermia for comatose cardiac arrest survivors after a return from a shockable rhythm (ventricular fibrillation [VF] or pulseless ventricular tachycardia [VT]) for 12–24 h and subsequent slow rewarming over 12–16 h had beneficial effects on survival and neurological outcomes [14, 15].
These studies laid the foundation for the 2005 American Heart Association guidelines recommending that unconscious adults with a return of spontaneous circulation after an out-of-hospital cardiac arrest should be cooled to 32–34 °C for 12–24 h when they initially had a shockable VF rhythm (Class IIa). A similar therapy may be beneficial for patients who experience non-VF arrests, both out-of-hospital and in-hospital (Class IIb) [16]. After the addition of >40 non-randomized studies supporting the beneficial effects of therapeutic hypothermia, the 2010 American Heart Association guidelines upgraded the recommendation level for comatose patients with a return of spontaneous circulation after an out-of-hospital cardiac arrest. The guidelines include shockable VF rhythm and pulseless VT rhythm (Class I), in-hospital cardiac arrests of any initial rhythm, and out-of-hospital cardiac arrests with initial rhythms of pulseless electrical activity or asystole (Class IIb) (Table 1) [17].
Other guidelines also recommend therapeutic hypothermia for unconscious survivors of out-of-hospital cardiac arrest with systolic blood pressures >90 mmHg, especially after VF or pulseless VT, despite the fact that the precise mechanisms of neuroprotection by therapeutic hypothermia are unknown [18]. A Cochrane review from 2012 supports these recommendations [19].
The negative impacts of therapeutic hypothermia have also been discussed. There are many immediate and delayed risks of complications, including bleeding, infection, metabolic and electrolyte changes, pharmacokinetic changes, cardiovascular effects, shivering, and seizures. The overall rate of these adverse events was reported to be approximately 70 %. However, because these complications were generally reported to be mild and transient, the benefits of therapeutic hypothermia outweigh these adverse effects [20].
Therefore, the main focus of recent studies on therapeutic hypothermia has been alternative indications, the most effective cooling methods, and the most beneficial treatment protocols and supportive therapies. As for other therapeutic hypothermia indications, its efficacy has been well-proven in neonatal encephalopathy patients, and it has been extensively investigated in stroke, traumatic brain injury, and spinal cord injury patients. However, we encounter difficulties in preventing shivering, especially in relatively conscious patients with well-maintained and normal thermoregulatory responses versus those who are comatose. In such cases, the most efficient drug combinations reported to induce thermal tolerance without respiratory depression or severe toxicity are a combination of buspirone and meperidine, and a combination of dexmedetomidine and either meperidine or buspirone [21–23].
However, recent trials demonstrated negative findings concerning therapeutic hypothermia. Two landmark therapeutic hypothermia trials published in 2002 were criticized for their small, underpowered sample sizes. The Bernard trial lacks neurological records from the time of hospital arrival and includes no structural assessment of patient outcome [14]. The Hypothermia After Cardiac Arrest trial is also deficient in that the traditional management group (control group) patients were febrile from approximately 12 h after the restoration of spontaneous circulation, which could have overestimated the effect of therapeutic hypothermia [15]. Fever following resuscitation is a factor well known to negatively impact patient outcome [24].
A rebuttal for therapeutic hypothermia
In a major multicenter trial, 1,359 survivors of out-of-hospital cardiac arrest were randomized to identify the advantages of pre-hospital cooling by rapidly infusing 2 L of cold normal saline approximately 1 h faster than the standard in-hospital method. Surprisingly, the results demonstrated no benefit in the survival rate between the intervention and control groups in either patients with VF (intervention group 62.7 % vs control group 64.3 %; P = 0.69) or without VF (intervention group 19.2 % vs control group 16.3 %; P = 0.30). Similarly, no benefit was observed in neurological outcomes with full recovery or mild impairment at discharge in VF (intervention group 57.5 % vs control group 61.9 %; P = 0.69) or non-VF patients (intervention group 14.4 % vs control group 13.4 %; P = 0.30). In contrast, the proportion of patients who experienced cardiac re-arrest during transport was significantly greater in the intervention group (26 vs 21 % in the control group; P = 0.008) [25]. It thus seems likely that the National Institute for Health and Care Excellence recommendation of cooling patients as soon as possible after cardiac arrest will need to be updated.
Experimental animal data have shown a survival advantage from immediate cooling, even before the return of spontaneous circulation [26–28]. This prehospital cooling trial has been criticized for taking too much time to cool patients compared with animal studies showing a brain protection benefit, even though the average duration to reach the goal temperature of <34 °C in patients receiving both pre-hospital and in-hospital cooling was 4.2 h, and approximately 1 h faster than for patients receiving only in-hospital cooling [25]. Furthermore, the cooling method of using 2 L of cold saline might have negative effects by inducing pulmonary edema and a reduction in coronary perfusion pressure [29]. Thus, alternate cooling methods such as intra-arrest evaporative cooling should be investigated to achieve faster cooling without negative effects and improve patient outcomes [30, 31].
Another clinical trial demonstrated no significant difference in the overall survival rate (hazard ratio 1.06 for 33 °C treatment vs 36 °C treatment; P = 0.51) or a composite of neurological outcome and death after 180 days of follow-up between groups strictly controlled at 33 and 36 °C by strictly preventing fever in comatose patients after cardiac arrest [32]. This study has the advantage of a larger sample size than the sum of the study populations of the other clinical trials. Although it has been criticized for selection bias, long delays before cooling, a shorter target temperature time of 10 h, and a rapid rewarming rate, this could also explain the lack of benefit from early pre-hospital cooling when fever had not yet occurred.
Taking the results of these two studies together, it might be possible that intentional fever prevention was all that was ever required to improve the outcome of comatose patients after cardiac arrest, which has not been demonstrated in randomized studies to date. In fact, Bernard, the author of the landmark therapeutic study in 2002 [14], recommended changing clinical practice guidelines towards strict temperature management for fever prevention, while another author on the Australian Resuscitation Council still recommends therapeutic hypothermia [15].
Future clinical studies will be required to elucidate the precise effects of various temperatures (32–36 °C) and treatment durations (24–72 h) on the outcomes of patients with shockable rhythms. Furthermore, future randomized controlled studies focusing on the effect of hyperoxia avoidance [33], arterial pressure maintenance [34], and early coronary intervention [35] on patient outcomes might be necessary.
Lastly, non-VF and VT are the most common initial cardiac rhythms, and represent the majority of deaths among adult in-hospital and out-of-hospital cardiac arrests. In fact, less than one-third of out-of-hospital and in-hospital cardiac arrest patients have VF or VT. The widespread use of the implantable cardioverter-defibrillator might cause this ratio to decline even further over time [36]. However, indications for therapeutic hypothermia in non-VF and VT patients remain unclear, and large randomized controlled trials might encounter difficulties in enrolling >1,000 patients, as non-VF and VT patients are resistant to returning to spontaneous circulation, and <10 % of these patients survive to be discharged from the hospital [37–41].
Regardless, the 2015 American Heart Association guidelines updated several recommendations concerning therapeutic hypothermia. First, all comatose adult patients with return of spontaneous circulation after both out-of and in-hospital cardiac arrest with any initial rhythm should receive the target temperature management between 32 and 36 °C (Class I), maintained constantly for at least 24 h (Class IIa). The selected temperature could be determined by clinician preference or clinical factors. Second, it may be reasonable to actively prevent fever in those patients after target temperature management (Class IIb). Lastly, the routine pre-hospital cooling of patients with rapid infusion of cold intravenous fluids after return of spontaneous circulation is not recommended (Class III) (Table 1) [42]. A summary of randomized controlled trials evaluating the therapeutic hypothermia in patients after cardiac arrest is shown in Table 2.
Fever management in critical care
Hyperthermia and fever
Hyperthermia, an elevation of core body temperature, can be divided into two clinical diagnoses—febrile hyperthermia (fever) and non-febrile hyperthermia. The distinction is that fever is specifically regulated, and thus difficult to treat. Textbooks on physiology document that in fever, exogenous and endogenous pyrogens actively shift the thermoregulatory threshold temperature upwards by affecting the thermoregulatory center control. Fever-like responses, including behavioral thermoregulation, are observed in invertebrates having solely innate immune responses, and are speculated to have developed 600 million years ago [43]. Thus, fever acts as a defensive reaction against pyrogens and foreign objects by increasing their clearance, the immune response, and heat-shocking proteins, along with protection against infectious agents [44–46].
On the other hand, in excessive exogenous heat exposure in hot environments and endogenous heat production in metabolic disorders, the thermoregulatory threshold temperature remains unchanged and passively results in non-febrile hyperthermia [47, 48]. In most cases, these two conditions can be differentiated after obtaining the patient’s history and performing a physical examination. However, they are difficult to differentiate in some cases, because thermoregulation can be maintained by changing the thermoregulation threshold in mild hyperthermia [49, 50]. Because medical treatment can save the life of non-febrile hyperthermia patients by decreasing their temperature below a critical level [51, 52], this review will focus on the clinical aspects of febrile hyperthermia (fever).
Association between fever and mortality in critically ill patients
More than 50 % of patients in intensive care units (ICUs) experience fever from infectious and non-infectious causes. Fever is associated with a longer ICU stay for general ICU patients and increased mortality, especially in certain groups such as patients with external and internal central nervous system injuries [53]. However, which critically ill patients will experience benefits or damage from the fever itself remain unknown in cases of infectious and non-infectious disease [54]. Although the febrile response is important to enhance the immune system, humans might not be well adapted to severe sepsis; however, mortality is increased without medical intervention.
A recent observational study reported that the adjusted odds ratio for in-hospital mortality in infectious patients, especially in the first 24 h after ICU admission, was lower when the peak temperature was in the range of 37.0–39.9 °C in an Australian and New Zealand cohort group, and even from 37.0 to >40 °C in an United Kingdom cohort, as opposed to normothermic patients (36.5–36.9 °C). Moreover, the adjusted odds ratio for in-hospital mortality was elevated for patients without infection with temperatures >39.0 °C compared to normothermia (36.5–36.9 °C) [55]. Another recent multicenter observational study demonstrated similar results, showing that patients with a maximal temperature >39.5 °C during their ICU stay had an increased 28-day mortality risk in a cohort without sepsis compared with normothermic patients (an adjusted odds ratio of 8.14 with every 1.0 °C increase, P < 0.01), but not in a cohort with sepsis (adjusted odds ratio 0.47; P = 0.11) [56]. Refractory postoperative fever is classically thought to be a benign clinical finding resulting from a postoperative inflammatory cytokine response. However, it sometimes exceeds 40 °C, in which case peak body temperature is reported to be the strongest predictor of patient mortality. There is also a strong positive association between patient mortality and peak body temperature [57].
Recent large retrospective cohort studies showed the survival advantage of a core temperature >37.5 °C in septic non-neutropenic patients, but not in neutropenic patients, indicating that neutrophil activation during fever had a clinical impact by improving patient mortality [58]. Taken together, fever in infectious patients could be advantageous, while it might be a maladaptive phenomenon in non-infectious patients.
We sometimes encounter hypothermia in septic patients (10–20 %). Because patient mortality was consistently worse in hypothermic infectious patients than in severely hyperthermic (hyperpyrexic) infectious patients in many previous studies, hypothermia might indicate an impaired immune response [59–61]. Furthermore, a bipolar presentation of fever and hypothermia along with hypothermia alone within the first 24 h after ICU admission in severely infectious patients significantly affected mortality [62]. These clinical studies indicate that thermoregulation might be dysregulated in conditions with hypothermia and biphasic temperature changes, likely from severe sepsis, as human temperature responses are concordant with those of rodents administered different doses of lipopolysaccharide (LPS). These studies show that a small amount (<101 µg/kg) of LPS increased core temperature by shifting the thermoregulatory threshold temperature upward, while medium doses (between 101 and 104 µg/kg) of LPS fluctuated the core temperature by widening the inter-threshold range, and high doses (>104 µg/kg) of LPS decreased core temperature, presumably by deteriorating thermoregulation further, especially below ambient temperature [63, 64]. Accordingly, when rats and mice are not allowed to regulate their body temperatures behaviorally, the direction of the body temperature response is determined by LPS dose and ambient temperature. Alternatively, it seems likely that the degree of clinical severity influences whether homeothermy is maintained in infectious disease.
Antipyretic treatment in critically ill patients
Recent guidelines concerning fever have documented the evaluation, diagnosis, and treatment of febrile patients, but do not describe temperature management [65]. Under wide ranges of fever definitions and management practices [66], most medical staff tend to manage hyperthermic patients when their temperatures rise >38.5 °C [67]. Although possible side-effects of fever include discomfort, increased heart rate, arrhythmia, accelerated cardiac output, and increased energy use, permitting fever without intervention might be advantageous in lowering personnel and drug costs related to patient care while improving survival.
It is known that neurologically damaged patients with fever should be treated, except for those with central nervous system infection [46, 68, 69]. Some prospective randomized clinical trials have focused on temperature changes, the amount of vasopressor use, tachycardia, oxygen consumption, and lactate levels in fever treatment [70–72]. Thus, the question of whether treating the fevers of neurologically normal critically ill patients using non-steroidal anti-inflammatory drugs and other cooling methods worsens mortality and morbidity remains unresolved, despite the classical clinical theme of the debate [46, 66, 73].
A small randomized clinical trial of 82 patients comparing critically ill patient mortality and morbidity between aggressively treated and permitted fever groups was terminated early because of unexpectedly higher mortality in the groups aggressively treated using non-steroidal anti-inflammatory drugs and cooling devices [74]. Although the target sample from the power analysis was not achieved, the question of increased mortality caused by routine early interventions for fever prevention arose. Recent large multicenter observational studies confirmed clinical findings that antipyretic drugs and acetaminophen increased mortality in septic patients (adjusted odds ratio 2.61 for non-steroidal anti-inflammatory drugs, P = 0.028; adjusted odds ratio 2.05 for acetaminophen, P = 0.01), in contrast to results showing little difference in mortality in non-septic patients (adjusted odds ratio 0.22 for non-steroidal anti-inflammatory drugs, P = 0.15; adjusted odds ratio 0.58 for acetaminophen, P = 0.63) in a multivariate analysis [56].
However, external cooling in septic shock patients significantly increased the percentage of patients with a 50 % decrease in baseline vasopressor dose 12 h after treatment (54 vs 20 %; P < 0.001) and shock reversal during their ICU stay (86 vs 73 %; P < 0.021), and decreased the 14-day mortality (19 vs 34 %; P < 0.013) as the secondary outcome [72]. Furthermore, a retrospective observational study showed a significant and independent association between acetaminophen use and reduced in-hospital mortality in critically ill patients after a multivariate logistic regression analysis including a propensity score for acetaminophen treatment (adjusted odds ratio = 0.60, P < 0.001), and after a Cox proportional hazards analysis (adjusted odds ratio 0.51, P < 0.001) [75]. A recent large multicenter, randomized, double-blind controlled trial to investigate intravenous acetaminophen administration every 6 h in critically ill patients with fever >38.0 °C did not find a decrease in ICU free days to day 28 (composite outcome combining mortality and ICU length of stay). Because open-label acetaminophen was administered after discontinuation of the study in approximately 30 % of patients exclusively due to ICU discharge, resolution of fever, or cessation of antimicrobial therapy, this study did not exclude the possibility of prolonged acetaminophen usage, which may have had a negative impact on patient outcome [76].
Furthermore, a clinical question might arise as to whether warming hypothermic septic patients might improve outcomes. This idea is not new, since therapeutic hyperthermia was used for patients with syphilis and gonorrhea in the early twentieth century [77, 78]. Other animals have been observed to typically show warmth-seeking behavior for thermoregulation along with fever from LPS administration, including rats [79–81], mice [82], and rabbits [83]. Therefore, increased temperature could be naturally beneficial. However, they initially express cold-seeking behavior, and higher doses of LPS in rodents result in hypothermia as the initial response. These phases are concordant with phases of arterial pressure drops in sepsis, indicating that regulatory hypothermia prevents cardiovascular collapse by thermoregulatory vasoconstriction [84]. Rodents improve their chances of survival by hypothermia with a regulated thermoregulatory response and cold-seeking behavior, and with increased heat loss following acute exposure to many toxic chemicals [85]. Hypothermic status might be advantageous in reducing the magnitude of the toxicity, despite prolonging the metabolism of toxic insults. In sepsis, hypothermic status has the advantage of maintaining arterial pressure and the disadvantage of increasing bacterial burden [86, 87]. However, regulated hypothermia with increased heat loss and decreased heat production is less likely to occur in large animals because of their limited ability to dissipate heat, resulting from their lower ratios of body surface area to body mass [85]. A summary of randomized controlled trials evaluating fever management in critically ill patients is shown in Table 3.
Conclusion
Since the advent of medicine, physicians have acknowledged that human body temperature significantly changes pathophysiologically with altering patient mortality. Ancient Egyptian, Greek, Roman, and Persian physicians investigated medical applications for hypothermia and febrile disorders over the centuries. However, we do not yet know the best temperature management strategies for comatose patients after cardiac arrest or for critically ill patients without a central nervous system disorder. Future research focusing on the generalizability of temperature intervention is urgently recommended, given the global and long-standing epidemiology of these patients.
References
Romanovsky AA. Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am J Physiol Regul Integr Comp Physiol. 2007;292(1):R37–46.
Rowell LB, Brengelmann GL, Blackmon JR, Murray JA. Redistribution of blood flow during sustained high skin temperature in resting man. J Appl Physiol. 1970;28(4):415–20.
Rowell LB. Cardiovascular aspects of human thermoregulation. Circ Res. 1983;52(4):367–79.
Johnson JM, Minson CT, Kellogg DL Jr. Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr Physiol. 2014;4(1):33–89.
Bennett AF, Ruben JA. Endothermy and activity in vertebrates. Science. 1979;206(4419):649–54.
Ruben J. The evolution of endothermy in mammals and birds: from physiology to fossils. Annu Rev Physiol. 1995;57:69–95.
Nespolo RF, Roff DA. Testing the aerobic model for the evolution of endothermy: implications of using present correlations to infer past evolution. Am Nat. 2014;183(1):74–83.
Clarke A, Portner HO. Temperature, metabolic power and the evolution of endothermy. Biol Rev Camb Philos Soc. 2010;85(4):703–27.
Bergman A, Casadevall A. Mammalian endothermy optimally restricts fungi and metabolic costs. MBio. 2010;1(5):e00212–310.
Guly H. History of accidental hypothermia. Resuscitation. 2011;82(1):122–5.
Fay T. Observations on generalized refrigeration in cases of severe cerebral trauma. Assoc Res Nerv Ment Dis Proc. 1945;24:611–9.
Botterell EH, Lougheed WM, Scott JW, Vandewater SL. Hypothermia, and interruption of carotid, or carotid and vertebral circulation, in the surgical management of intracranial aneurysms. J Neurosurg. 1956;13(1):1–42.
Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118(23):2452–83.
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–63.
Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–56.
ECC Committee, Subcommittees and Task Forces of the American Heart Association. American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1–203.
Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL, American Heart Association. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S768–86.
Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B, ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81(10):1219–76.
Arrich J, Holzer M, Havel C, Müllner M, Herkner H. Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. Cochrane Database Syst Rev. 2012;9:CD004128.
Noyes AM, Lundbye JB. Managing the complications of mild therapeutic hypothermia in the cardiac arrest patient. J Intensive Care Med. 2015;30(5):259–69.
Kurz A, Ikeda T, Sessler DI, Larson MD, Bjorksten AR, Dechert M, Christensen R. Meperidine decreases the shivering threshold twice as much as the vasoconstriction threshold. Anesthesiology. 1997;86(5):1046–54.
Lenhardt R, Orhan-Sungur M, Komatsu R, Govinda R, Kasuya Y, Sessler DI, Wadhwa A. Suppression of shivering during hypothermia using a novel drug combination in healthy volunteers. Anesthesiology. 2009;111(1):110–5.
Mokhtarani M, Mahgoub AN, Morioka N, Doufas AG, Dae M, Shaughnessy TE, Bjorksten AR, Sessler DI. Buspirone and meperidine synergistically reduce the shivering threshold. Anesth Analg. 2001;93(5):1233–9.
Gebhardt K, Guyette FX, Doshi AA, Callaway CW, Rittenberger JC, Post Cardiac Arrest Service. Prevalence and effect of fever on outcome following resuscitation from cardiac arrest. Resuscitation. 2013;84(8):1062–7.
Kim F, Nichol G, Maynard C, Hallstrom A, Kudenchuk PJ, Rea T, Copass MK, Carlbom D, Deem S, Longstreth WT Jr, Olsufka M, Cobb LA. Effect of prehospital induction of mild hypothermia on survival and neurological status among adults with cardiac arrest: a randomized clinical trial. JAMA. 2014;311(1):45–52.
Abella BS, Zhao D, Alvarado J, Hamann K, Vanden Hoek TL, Becker LB. Intra-arrest cooling improves outcomes in a murine cardiac arrest model. Circulation. 2004;109(22):2786–91.
Tsai MS, Barbut D, Wang H, Guan J, Sun S, Inderbitzen B, Weil MH, Tang W. Intra-arrest rapid head cooling improves postresuscitation myocardial function in comparison with delayed postresuscitation surface cooling. Crit Care Med. 2008;36(11 Suppl):S434–9.
Chenoune M, Lidouren F, Adam C, Pons S, Darbera L, Bruneval P, Ghaleh B, Zini R, Dubois-Randé JL, Carli P, Vivien B, Ricard JD, Berdeaux A, Tissier R. Ultrafast and whole-body cooling with total liquid ventilation induces favorable neurological and cardiac outcomes after cardiac arrest in rabbits. Circulation. 2011;124(8):901–11, 1–7.
Kim F, Olsufka M, Longstreth WT Jr, Maynard C, Carlbom D, Deem S, Kudenchuk P, Copass MK, Cobb LA. Pilot randomized clinical trial of prehospital induction of mild hypothermia in out-of-hospital cardiac arrest patients with a rapid infusion of 4 °C normal saline. Circulation. 2007;115(24):3064–70.
Lyon RM, Van Antwerp J, Henderson C, Weaver A, Davies G, Lockey D. Prehospital intranasal evaporative cooling for out-of-hospital cardiac arrest: a pilot, feasibility study. Eur J Emerg Med. 2014;21(5):368–70.
Uray T, Mayr FB, Stratil P, Aschauer S, Testori C, Sterz F, Haugk M. Prehospital surface cooling is safe and can reduce time to target temperature after cardiac arrest. Resuscitation. 2015;87:51–6.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Åneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Køber L, Langørgen J, Lilja G, Møller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H, TTM Trial Investigators. Targeted temperature management at 33 °C versus 36 °C after cardiac arrest. N Engl J Med. 2013;369(23):2197–206.
Wang CH, Chang WT, Huang CH, Tsai MS, Yu PH, Wang AY, Chen NC, Chen WJ. The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and meta-analysis of observational studies. Resuscitation. 2014;85(9):1142–8.
Sutton RM, Friess SH, Maltese MR, Naim MY, Bratinov G, Weiland TR, Garuccio M, Bhalala U, Nadkarni VM, Becker LB, Berg RA. Hemodynamic-directed cardiopulmonary resuscitation during in-hospital cardiac arrest. Resuscitation. 2014;85(8):983–6.
Larsen JM, Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest—a systematic review and meta-analysis. Resuscitation. 2012;83(12):1427–33.
Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288(23):3008–13.
Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R, Munkley DP, Lyver MB, Luinstra LG, Campeau T, Maloney J, Dagnone E. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase II. Ontario Prehospital Advanced Life Support. JAMA. 1999;281(13):1175–81.
Rehmani R, Baqir M, Amanullah S. Return of spontaneous circulation and survival at hospital discharge in patients with out-of-hospital and emergency department cardiac arrests in a tertiary care centre. J Pak Med Assoc. 2007;57(6):278–81.
Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I, Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31.
Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81.
Sandroni C, Cavallaro F, Antonelli M. Therapeutic hypothermia: is it effective for non-VF/VT cardiac arrest? Crit Care. 2013;17(2):215.
Callaway CW, Soar J, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, Donnino MW, Drajer S, Kloeck W, Morley PT, Morrison LJ, Neumar RW, Nicholson TC, Nolan JP, Okada K, O’Neil BJ, Paiva EF, Parr MJ, Wang TL, Witt J, Advanced Life Support Chapter Collaborators. Part 4: advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16 Suppl 1):S84–145.
Hasday JD, Thompson C, Singh IS. Fever, immunity, and molecular adaptations. Compr Physiol. 2014;4(1):109–48.
Kluger MJ, Ringler DH, Anver MR. Fever and survival. Science. 1975;188(4184):166–8.
Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol. 2015;15(6):335–49.
Jefferies S, Weatherall M, Young P, Eyers S, Perrin KG, Beasley CR. The effect of antipyretic medications on mortality in critically ill patients with infection: a systematic review and meta-analysis. Crit Care Resusc. 2011;13(2):125–31.
Kluger MJ. Fever vs. hyperthermia. N Engl J Med. 1978;299(10):555.
Stitt JT. Fever versus hyperthermia. Fed Proc. 1979;38(1):39–43.
Mack G, Nishiyasu T, Shi X. Baroreceptor modulation of cutaneous vasodilator and sudomotor responses to thermal stress in humans. J Physiol. 1995;483(Pt 2):537–47.
Nakajima Y, Nose H, Takamata A. Plasma hyperosmolality and arterial pressure regulation during heating in dehydrated and awake rats. Am J Physiol. 1998;275(5 Pt 2):R1703–11.
Danzl DF. Hyperthermic syndromes. Am Fam Physician. 1988;37(6):157–62.
Lee-Chiong TL Jr, Stitt JT. Disorders of temperature regulation. Compr Ther. 1995;21(12):697–704.
Laupland KB, Shahpori R, Kirkpatrick AW, Ross T, Gregson DB, Stelfox HT. Occurrence and outcome of fever in critically ill adults. Crit Care Med. 2008;36(5):1531–5.
Harden LM, Kent S, Pittman QJ, Roth J. Fever and sickness behavior: friend or foe? Brain Behav Immun. 2015;50:322–33.
Young PJ, Saxena M, Beasley R, Bellomo R, Bailey M, Pilcher D, Finfer S, Harrison D, Myburgh J, Rowan K. Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med. 2012;38(3):437–44.
Lee BH, Inui D, Suh GY, Kim JY, Kwon JY, Park J, Tada K, Tanaka K, Ietsugu K, Uehara K, Dote K, Tajimi K, Morita K, Matsuo K, Hoshino K, Hosokawa K, Lee KH, Lee KM, Takatori M, Nishimura M, Sanui M, Ito M, Egi M, Honda N, Okayama N, Shime N, Tsuruta R, Nogami S, Yoon SH, Fujitani S, Koh SO, Takeda S, Saito S, Hong SJ, Yamamoto T, Yokoyama T, Yamaguchi T, Nishiyama T, Igarashi T, Kakihana Y, Koh Y, Fever and Antipyretic in Critically ill patients Evaluation (FACE) Study Group. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care. 2012;16(1):R33.
Barie PS, Hydo LJ, Eachempati SR. Causes and consequences of fever complicating critical surgical illness. Surg Infect (Larchmt). 2004;5(2):145–59.
Weinkove R, Bailey M, Bellomo R, Saxena MK, Tam CS, Pilcher DV, Beasley R, Young PJ. Association between early peak temperature and mortality in neutropenic sepsis. Ann Hematol. 2015;94(5):857–64.
Marik PE, Zaloga GP. Hypothermia and cytokines in septic shock. Norasept II Study Investigators. North American study of the safety and efficacy of murine monoclonal antibody to tumor necrosis factor for the treatment of septic shock. Intensive Care Med. 2000;26(6):716–21.
Kushimoto S, Gando S, Saitoh D, Mayumi T, Ogura H, Fujishima S, Araki T, Ikeda H, Kotani J, Miki Y, Shiraishi S, Suzuki K, Suzuki Y, Takeyama N, Takuma K, Tsuruta R, Yamaguchi Y, Yamashita N, Aikawa N, JAAM Sepsis Registry Study Group. The impact of body temperature abnormalities on the disease severity and outcome in patients with severe sepsis: an analysis from a multicenter, prospective survey of severe sepsis. Crit Care. 2013;17(6):R271.
Schell-Chaple HM, Puntillo KA, Matthay MA, Liu KD, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Body temperature and mortality in patients with acute respiratory distress syndrome. Am J Crit Care. 2015;24(1):15–23.
Laupland KB, Zahar JR, Adrie C, Schwebel C, Goldgran-Toledano D, Azoulay E, Garrouste-Orgeas M, Cohen Y, Jamali S, Souweine B, Darmon M, Timsit JF. Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med. 2012;40(1):145–51.
Romanovsky AA, Shido O, Sakurada S, Sugimoto N, Nagasaka T. Endotoxin shock: thermoregulatory mechanisms. Am J Physiol. 1996;270(4 Pt 2):R693–703.
Rudaya AY, Steiner AA, Robbins JR, Dragic AS, Romanovsky AA. Thermoregulatory responses to lipopolysaccharide in the mouse: dependence on the dose and ambient temperature. Am J Physiol Regul Integr Comp Physiol. 2005;289(5):R1244–52.
O’Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, Linden P, Maki DG, Nierman D, Pasculle W, Masur H, American College of Critical Care Medicine; Infectious Diseases Society of America. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med. 2008;36(4):1330–49.
Niven DJ, Laupland KB, Tabah A, Vesin A, Rello J, Koulenti D, Dimopoulos G, de Waele J, Timsit JF, EUROBACT Investigators. Diagnosis and management of temperature abnormality in ICUs: a EUROBACT investigators’ survey. Crit Care. 2013;17(6):R289.
Egi M, Morita K. Fever in non-neurological critically ill patients: a systematic review of observational studies. J Crit Care. 2012;27(5):428–33.
Clifton GL, Miller ER, Choi SC, Levin HS, McCauley S, Smith KR Jr, Muizelaar JP, Wagner FC Jr, Marion DW, Luerssen TG, Chesnut RM, Schwartz M. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001;344(8):556–63.
Oliveira-Filho J, Ezzeddine MA, Segal AZ, Buonanno FS, Chang Y, Ogilvy CS, Rordorf G, Schwamm LH, Koroshetz WJ, McDonald CT. Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology. 2001;56(10):1299–304.
Bernard GR, Wheeler AP, Russell JA, Schein R, Summer WR, Steinberg KP, Fulkerson WJ, Wright PE, Christman BW, Dupont WD, Higgins SB, Swindell BB. The effects of ibuprofen on the physiology and survival of patients with sepsis. The Ibuprofen in Sepsis Study Group. N Engl J Med. 1997;336(13):912–8.
Morris PE, Promes JT, Guntupalli KK, Wright PE, Arons MM. A multi-center, randomized, double-blind, parallel, placebo-controlled trial to evaluate the efficacy, safety, and pharmacokinetics of intravenous ibuprofen for the treatment of fever in critically ill and non-critically ill adults. Crit Care. 2010;14(3):R125.
Schortgen F, Clabault K, Katsahian S, Devaquet J, Mercat A, Deye N, Dellamonica J, Bouadma L, Cook F, Beji O, Brun-Buisson C, Lemaire F, Brochard L. Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med. 2012;185(10):1088–95.
Niven DJ, Stelfox HT, Laupland KB. Antipyretic therapy in febrile critically ill adults: a systematic review and meta-analysis. J Crit Care. 2013;28(3):303–10.
Schulman CI, Namias N, Doherty J, Manning RJ, Li P, Elhaddad A, Lasko D, Amortegui J, Dy CJ, Dlugasch L, Baracco G, Cohn SM. The effect of antipyretic therapy upon outcomes in critically ill patients: a randomized, prospective study. Surg Infect (Larchmt). 2005;6(4):369–75.
Suzuki S, Eastwood GM, Bailey M, Gattas D, Kruger P, Saxena M, Santamaria JD, Bellomo R. Paracetamol therapy and outcome of critically ill patients: a multicenter retrospective observational study. Crit Care. 2015;19:162.
Young P, Saxena M, Bellomo R, Freebairn R, Hammond N, van Haren F, Holliday M, Henderson S, Mackle D, McArthur C, McGuinness S, Myburgh J, Weatherall M, Webb S, Beasley R, HEAT Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group. Acetaminophen for fever in critically Ill patients with suspected infection. N Engl J Med. 2015;373(23):2215–24.
Owens C. The value of fever therapy for gonorrhea. JAMA. 1936;107:1942–6.
Wagner-Jauregg J. The history of the malaria treatment of general paralysis. Am J Psychiatry. 1994;151(6 Suppl):231–5.
Sugimoto N, Shido O, Sakurada S, Nagasaka T. Day-night variations of behavioral and autonomic thermoregulatory responses to lipopolysaccharide in rats. Jpn J Physiol. 1996;46(6):451–6.
Bodurka M, Caputa M, Bodurka J. A comparison of febrile responses induced by LPS from E. coli and S. abortus in unrestrained rats placed in a thermal gradient. J Physiol Pharmacol. 1997;48(1):81–8.
Briese E. Selected temperature correlates with intensity of fever in rats. Physiol Behav. 1997;61(5):659–60.
Akins C, Thiessen D, Cocke R. Lipopolysaccharide increases ambient temperature preference in C57BL/6J adult mice. Physiol Behav. 1991;50(2):461–3.
Satinoff E, McEwen GN Jr, Williams BA. Behavioral fever in newborn rabbits. Science. 1976;193(4258):1139–40.
Almeida MC, Steiner AA, Branco LG, Romanovsky AA. Cold-seeking behavior as a thermoregulatory strategy in systemic inflammation. Eur J Neurosci. 2006;23(12):3359–67.
Gordon CJ. Response of the thermoregulatory system to toxic insults. Front Biosci (Elite Ed). 2010;2:293–311.
Allen FM. Theory and therapy of shock: reduced temperatures in shock therapy. Am J Surg. 1943;60:335–48.
Liu E, Lewis K, Al-Saffar H, Krall CM, Singh A, Kulchitsky VA, Corrigan JJ, Simons CT, Petersen SR, Musteata FM, Bakshi CS, Romanovsky AA, Sellati TJ, Steiner AA. Naturally occurring hypothermia is more advantageous than fever in severe forms of lipopolysaccharide- and Escherichia coli-induced systemic inflammation. Am J Physiol Regul Integr Comp Physiol. 2012;302(12):R1372–83.
Hachimi-Idrissi S, Corne L, Ebinger G, Michotte Y, Huyghens L. Mild hypothermia induced by a helmet device: a clinical feasibility study. Resuscitation. 2001;51(3):275–81.
Laurent I, Adrie C, Vinsonneau C, Cariou A, Chiche JD, Ohanessian A, Spaulding C, Carli P, Dhainaut JF, Monchi M. High-volume hemofiltration after out-of-hospital cardiac arrest: a randomized study. J Am Coll Cardiol. 2005;46(3):432–7.
Bernard GR, Reines HD, Halushka PV, Higgins SB, Metz CA, Swindell BB, Wright PE, Watts FL, Vrbanac JJ. Prostacyclin and thromboxane A2 formation is increased in human sepsis syndrome. Effects of cyclooxygenase inhibition. Am Rev Respir Dis. 1991;144(5):1095–101.
Haupt MT, Jastremski MS, Clemmer TP, Metz CA, Goris GB. Effect of ibuprofen in patients with severe sepsis: a randomized, double-blind, multicenter study. The Ibuprofen Study Group. Crit Care Med. 1991;19(11):1339–47.
Memiş D, Karamanlioğlu B, Turan A, Koyuncu O, Pamukçu Z. Effects of lornoxicam on the physiology of severe sepsis. Crit Care. 2004;8(6):R474–82.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakajima, Y. Controversies in the temperature management of critically ill patients. J Anesth 30, 873–883 (2016). https://doi.org/10.1007/s00540-016-2200-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2200-7