Abstract
Background
The interaction between T-cells/fatty acids involved in non-alcoholic fatty liver disease (NAFLD) and liver fibrosis progression is poorly understood. In this study, we conducted a comprehensive analysis of T-cell profiles of NAFLD patients to better understand their relationship with fatty acids and relevance to liver fibrosis.
Methods
We analyzed the differences in T-cell profiles of peripheral blood mononuclear cells (PBMCs) between 40 NAFLD patients and 5 healthy volunteers (HVs), and their relationship with liver fibrosis stage or progression. Moreover, we analyzed the relationship between T-cell profiles and fatty acid compositions in vivo, and changes in T-cell profiles after treatment with fatty acids in vitro.
Results
T-cell profiles of NAFLD patients were different from those of HVs. The CD25+CD45+CD4+ T-cell frequency was increased in NAFLD patients with high liver fibrosis stage and progression, and this indicated immune activation. Despite such a state of immune activation, the PD1+CD4+ T-cell frequency was decreased in the same patients group. The PD1+CD4+ T-cell frequency had a significantly negative correlation with the serum fatty acid composition ratio C16:1n7/C16:0. Moreover, the PD1+CD4+ T-cell frequency was significantly decreased by in vitro treatment with fatty acids. In addition, its rate of frequency change was significantly different between C16:0 and C16:1n7 and decreased by artificially increasing the C16:1n7/C16:0 ratio.
Conclusions
The analysis of PBMCs in NAFLD patients showed that T-cell profiles were different from those of HVs. And, it suggested that fatty acids modified T-cell profiles and were involved in liver fibrosis in NAFLD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With an increase in the number of patients with obesity, diabetes, and dyslipidemia, the phenotype of metabolic syndrome of the liver, non-alcoholic fatty liver disease (NAFLD), has become the main cause of chronic liver disease [1]. The pathology of non-alcoholic steatohepatitis (NASH) accompanied by inflammation is a risk factor for hepatic cirrhosis and hepatocellular carcinoma with poor prognosis [2].
The liver is the central metabolic organ in the human body and also the largest organ involved in the immune system. Approximately half of the non-hepatocytes, comprising 20–40% of all liver cells, are immune cells. Lymphocytes involved in acquired immunity comprise approximately 15% of the non-hepatocytes [3]. In the liver of a NASH mouse model, cluster of differentiation 8-positive (CD8+)/CD4+ T-cell ratio increases [4], while CD4+ T-cells selectively decreases [5]. In addition, acquired immunity in NASH is caused by oxidative stress and is related to hepatic inflammation [6]. Thus, NAFLD pathology is closely linked to acquired immunity.
NAFLD is characterized by a disruption of fat metabolism that induces fat accumulation in the liver, resulting in a fatty liver. Previously, we have shown that the progression of NASH is driven by the changes in the metabolic pathways that digest accumulated fatty acids in the hepatocytes [7]. Furthermore, such accumulated fatty acids have been reported to induce immune cell infiltration through lipotoxicity characterized by apoptosis, endoplasmic reticulum oxidative stress, and mitochondrial dysfunction that affects NAFLD pathophysiology [8, 9].
Therefore, both the immune system and fatty acids are closely associated with NAFLD disease progression. Recently, the regulation of fatty acid metabolism has been elucidated as the main mechanism behind T-cell differentiation and regulation [10,11,12], serving as a central regulatory switch that determines T-cell fate [13]. These findings suggest that fatty acids are linked to immune cells through direct and indirect lipotoxicity-driven effects; however, the details of this association are unknown.
In the present study, we analyzed the peripheral blood of NAFLD patients to investigate T-cell profiles and better understand their associations with pathophysiology and fatty acids in vivo. Moreover, by analyzing changes in the peripheral blood mononuclear cells (PBMCs) upon treatment with fatty acids in vitro, we investigated whether fatty acids can modify NAFLD pathophysiology by affecting the profiles of T-cell.
Methods
Patient population
The target population of this study was patients diagnosed with NAFLD through ultrasound-guided percutaneous liver biopsy at Kanazawa University Hospital, and healthy volunteers. Healthy volunteers were judged normal by a medical examination and the absence of fat deposition in the liver was confirmed by abdominal ultrasound. All participants in this study tested negative for hepatitis B surface antigen and hepatitis C virus antibody, and were free of any other chronic liver diseases. Furthermore, we excluded patients with a history of significant alcoholic consumption (alcohol consumption over 20 g/day), long-term use of steatogenic medications, or suffering from diseases associated with liver fat deposition, such as monogenic hereditary disorders [2]. Two pathologists independently conducted pathological evaluation and diagnosis. Three evaluation items (steatosis, lobular inflammation, and hepatocellular ballooning) were scored for the NAFLD activity score (NAS) along with fibrosis in all patients [14]. All patients gave written informed consent to participate in the study in accordance with the Helsinki declaration. This study was approved by the regional ethics committee (Medical Ethics Committee of Kanazawa University, No. 2418).
Laboratory testing and isolation of peripheral blood mononuclear cells
Fasting blood samples for testing were collected from patients before liver biopsy and from healthy volunteers. Serum for fatty acid extraction and PBMCs were also collected simultaneously. PBMCs were separated as previously described [15]. PBMCs were resuspended in Roswell Park Memorial Institute (RPMI) 1640 medium containing 80% fetal calf serum (FCS) and 10% dimethyl sulfoxide and cryopreserved until use.
Analysis of peripheral T-cell profiles
For analyzing of peripheral T-cell profiles, PBMCs were collected from 5 healthy volunteers, 40 NAFLD patients, and 13 patients with serial liver biopsy. A multicolor fluorescence-activated cell sorting analysis was conducted using the Becton–Dickinson FACSAria II system to determine the frequency and phenotype of CD4+ T-cell, CD8+ T-cell, and regulatory T-cell (Treg) cells [16].
Treg cells were classified based on forkhead box P3 (FoxP3). Transcriptional factors, T-box expressed in T-cells (T-bet), GATA3, and retinoic acid-related orphan receptor gamma t (RORγt), were used to distinct the CD4+ T-cell subpopulations T-helper (Th)1, Th2, and Th17 cells.
Moreover, the expression levels of CD25, T-lymphocyte-associated protein 4 (CTLA-4), programmed death 1 (PD-1), C-X-C motif chemokine receptor 3 (CXCR3), C–C motif chemokine receptor 4 (CCR4), CCR6, OX40, CD80, and 4-1BB on each T-cell were evaluated using antibodies against each marker.
The difference between the T-cell frequency of healthy volunteers and NAFLD patients was analyzed. T-cell profiles were evaluated by dividing 40 patients with NAFLD into 2 groups with a fibrosis score of 1 or less (F0–1) and 2 or more (F2–4) to better understand the relationship between T-cells and liver fibrosis stage. Furthermore, in 13 patients with serial liver biopsy, we tracked the changes in T-cell profiles at initial and second biopsies between a progress group, whose members showed a pathological progression of fibrosis, and a non-progress group, whose members showed improvement or no change in fibrosis.
Fatty acid extraction
To analyze the relationship between peripheral T-cell profiles and fatty acids, fatty acids were extracted from the liver tissue and serum samples. Liver specimens collected by percutaneous liver biopsy and serum samples collected before breakfast at diagnosis were used. The wet weight of the liver specimen was measured, and 200 μL of serum was used. Fatty acids were extracted as previously reported [7].
Measurement and analysis of liver tissue and serum fatty acids
Extracted fatty acids were identified and quantified using gas chromatography. The SHIMADZU gas chromatograph GC-2014AF/SPL was used as the measurement device, and Rtx-2330 was used for the column. Gas chromatograms were analyzed using GCsolution version 2.3 (Shimadzu Corporation, Kyoto, Japan). To identify and quantitatively analyze fatty acids, the external reference method was employed using Supelco TM37 Component FAME Mix 47885-U (Sigma-Aldrich, St. Louis, MO, USA) as a standard solution. The fatty acid content was quantified as an amount per mg of wet liver tissue or per 200 μL of serum.
Co-cultured of PBMCs with fatty acids
To confirm the relationship between T-cells and fatty acids in vivo, we analyzed the change in T-cell profiles after treating individual fatty acid in vitro. We selected C16:0 and C18:0 that exhibit strong lipotoxicity [10, 17], C16:1n7 whose ratio with C16:0 is associated with lobular inflammation [7] and increased in NASH patients [18]. In addition, to better mimic in vivo conditions [18], fatty acids were artificially modified to obtain a composition ratio (C16:1n7/C16:0, C18:0/C16:0) of 0.05 or 0.5, respectively. PBMCs obtained from 19 NAFLD patients were incubated with 50 μM each fatty acid (final concentration) or different fatty acid composition ratio in RPMI medium for 24 h, and the frequencies of T-cells were measured by a multicolor fluorescence-activated cell sorting analysis. There was no cellular toxicity in lymphocytes at 50 μM concentration. C16:0, C16:1n7, C18:0, were purchased from Sigma. Fatty acids were dissolved in 50% ethanol, RPMI with 2% fatty-acid-free bovine serum albumin (BSA; Sigma, A6003) was added, and the mixture was warmed to 37 °C. Next, one round of vortexing was conducted, followed by incubation at 45 °C for 5 min. The culture medium was cooled to 37 °C, following which PBMCs were added and incubated at 37 °C for 24 h. Since the fatty acids were dissolved in 50% ethanol, control samples were prepared such that the same volume of 50% ethanol as that in the experimental samples was incorporated in RPMI with 2% fatty-acid-free bovine serum albumin. The final ethanol concentration was 0.025%, a concentration below cellular toxicity levels [19].
Fluorescent multiplex immunohistochemistry
Fluorescent multiplex immunohistochemistry (IHC) was done using an Opal™ Solid Tumor Immunology Kit (PerkinElmer, OP7TL4001KT), a tyramide signal amplification plus system that performed multiple fluorescence detection using multiple antibodies on formalin-fixed paraffin-embedded tissue sections. Among the primary antibodies in this kit anti-CD4, anti-CD8, anti-FoxP3, and 4′,6-diamidino-2-phenylindole (DAPI) antibodies were used. Furthermore, rabbit monoclonal anti-CD25 and rabbit monoclonal anti-PD1 antibodies were added. The following procedure was repeated for each combination of primary and fluorescent antibody: microwave treatment, blocking, primary antibody incubation, secondary antibody incubation, and fluorophore incubation [20]. The slide was evaluated using the Mantra™ quantitative pathology workstation (PerkinElmer).
Immunohistochemistry
Immunostaining was done using a DAKO EnVision™ kit with an immunoperoxidase technique. Rabbit anti-CD4 and rabbit anti-CD8 were used as primary antibodies. Counts of T-cells per unit area were calculated using the BIOREVO BZ-9000 fluorescence microscope image analysis system (KEYENCE Japan). The unit area was defined as the area of one image acquired at a 200-fold magnification.
Statistical analysis
Data are expressed as the median value (range). T-cell profiles were evaluated using the Mann–Whitney U test. The changes in T-cell profiles between the initial and second biopsies of the patients with serial liver biopsy were evaluated using the Wilcoxon signed-rank test. The comparison of fatty acid treatment samples with the control sample was evaluated using the Wilcoxon signed-rank test, whereas fatty acid comparisons were evaluated using the Mann–Whitney U test. Cytokine comparisons to the control samples were evaluated with the Wilcoxon signed-rank test. T-cell frequency and cell surface markers, along with their relationships to fatty acids were evaluated with Spearman’s rank correlation.
Results
Peripheral blood T-cell profiles in NAFLD patients differ from those of healthy volunteers
The background information of 5 healthy volunteers and 40 NAFLD patients whose T-cell profiles were analyzed in the present study is shown in Table 1. PBMCs analyzed by flow cytometry are shown in Fig. 1a, b. The frequencies of CD4+ or CD8+ T-cells were not different in NAFLD patients compared to those in healthy volunteers (Supplementary Fig. 1a). On the other hand, T-cell profiles of NAFLD patients differed from those of healthy volunteers (Supplementary Fig. 1b). The frequencies of Th2 or Th17 cells that acquired an effector function were significantly increased in NAFLD patients compared to those in healthy volunteers (Supplementary Fig. 1c). Moreover, the frequencies of OX40+CD4+, CD80+CD8+, and CD25+CD45RA+CD4+ T-cells expressing activation markers were increased in NAFLD patients (Fig. 1c, Supplementary Fig. 1b). The PD1+CD4+ T-cell and CXCR3+CD4+ T-cell frequencies were significantly lower in NAFLD patients (Fig. 1c). The expression of PD1 in CD25+CD45RA+CD4+ T-cell was significantly lower in NAFLD patients than in healthy volunteers (Fig. 1d).
Peripheral blood T-cell profiles in NAFLD patients differ from those of healthy volunteers. a Treg cells were classified based on FoxP3 and CD45RA into effector Treg cells (CD45RA−CD4+FoxP3++ T-cells) or naïve Treg cells (CD45RA+CD4+FoxP3+ T-cells). In addition, the CD4+FoxP3− T-cell population was classified based on the presence or absence of CD45RA into CD45RA+CD4+ T-cells or CD45RA−CD4+ T-cells. And, CD8+ T-cell population was similarly classified CD45RA+CD8+ T-cells or CD45RA−CD8+ T-cells. b Each cell expressing cell surface antigens measured are shown. c For each T-cell subtype, the significant differences in frequency between healthy volunteers (normal) and NAFLD patients are shown. d PD1+CD25+CD45RA+CD4+ T-cell frequency are shown. Comparison between the two groups was analyzed by the Mann–Whitney U test
CD25+CD45RA+CD4+ T-cells were a heterogeneous population containing cells expressing T-bet, GATA3, or ROR-γt in significantly different frequencies (Supplementary Fig. 2a). Furthermore, the frequencies of RORγt-expressing T-cells in CD25+CD45RA+CD4+ T-cells increased significantly in relation to those in healthy volunteers (Supplementary Fig. 2b).
Peripheral T-cell profiles are involved in liver fibrosis stage
There were 28 cases in the F0–1 group and 12 cases in the F2–4 group (Supplementary Table 1). As shown in Fig. 2, the PD1+CD4+ T-cell, CXCR3+CD4+ T-cell, and PD1+CD25+CD45RA+CD4+ T-cell frequencies were significantly lower in the F2–4 group compared with the F0–1 group. On the other hand, the CD25+CD45RA+CD4+ T-cell frequency was significantly higher in the F2–4 group compared to the F0–1 group. Furthermore, the frequency of these cells in the F2–4 group was significantly different when compared with the healthy volunteers.
T-cells subsets were associated with histopathology indicative of NAFLD, such as fibrosis, lobular inflammation, and ballooning (Supplementary Fig. 3).
Peripheral T-cell profiles are involved in liver fibrosis progression
To further investigate the relationship between T-cells and fibrosis progression, we analyzed the T-cell profiles of 13 patients who underwent serial liver biopsy. Background information of these 13 patients is shown in Supplementary Table 2. As shown in Fig. 3, the PD1+CD4+ T-cell frequency was maintained at a low level in the progress group, whereas it was maintained at a high level in the non-progress group. Contrastingly, the CD25+CD45RA+CD4+ T-cell frequency was maintained at a high level in the progress group, and it was significantly reduced over time in the non-progress group.
Peripheral T-cell profiles are involved in liver fibrosis progression. The frequency of PD1+CD4+ T-cells and CD25+CD45RA+CD4+ T-cells in 13 serial liver biopsy patients were evaluated for an initial, and a second biopsy; * denotes evaluation by the Wilcoxon signed-rank test and † denotes evaluation by the Mann–Whitney U test
Peripheral T-cell frequencies are correlated with serum fatty acids in vivo
Focusing on fatty acids as a factor affecting T-cell profiles in NAFLD patients, we investigated the relationship between the frequency of each T-cell type and in vivo serum/liver tissue fatty acid composition. Out of 40 patients, serum fatty acid was measured for 20 NAFLD patients, while liver tissue fatty acid was measured for 24 NAFLD patients (Supplementary Tables 3, 4). We compared these serum and liver tissue fatty acids values and found a strong correlation between the C16:1n7/C16:0 fatty acid composition ratio (p < 0.0001) (Supplementary Table 5). These results were similar to those of our previous study [7, 18].
The CD4+ T-cell frequency was negatively correlated with many serum fatty acids; the strongest negative correlation was observed with serum C18:2 as described previously [5, 17] (Fig. 4a).
Peripheral T-cell frequencies are correlated with serum fatty acids in vivo. a The correlation between each T-cell and fatty acids in serum or liver tissue are shown. Especially, the frequency of CD4+ T-cell showed a significantly negative correlation with serum C18:2. b The correlation between each subset of CD4+ T-cells and C16:1n7/C16:0, as well as the correlation between PD1+CD4+ T-cells and C16:1n7/C16:0 are shown. c The correlation between each subset of CD4+ T-cells and C18:0/C16:0, along with the correlation between PD1+CD4+ T-cells and C18:0/C16:0 are shown. The correlation was evaluated using the Spearman’s rank correlation coefficient. Statistical significance was denoted as: *p < 0.05, †p < 0.01, and ‡p < 0.001. The degree of correlation is indicated separately by color
In vivo investigations showed that fatty acids had different effects on each T-cell. Especially, the PD1+CD4+ T-cell and CXCR3+CD4+ T-cell frequencies had significantly negative correlations with the serum fatty acid composition ratios C16:1n7/C16:0 or C18:0/C16:0, respectively (Fig. 4b, c).
In vitro fatty acid treatment changes T-cell profiles in PBMCs
Using PBMCs from 19 NAFLD patients, we analyzed changes in individual T-cell frequencies upon in vitro fatty acid treatment. The demographics of the 19 patients are shown in Supplementary Table 6. Although the treatment of fatty acids resulted in various changes, many fatty acids reduced the frequency of T-cells. And, the rate of T-cell frequency change due to the treatment with fatty acids differed according to the treated fatty acid. Particularly, the rate of frequency change significantly differed for the PD1+CD4+ T-cells between C16:0 and C16:1n7 and CXCR3+CD4+ T-cells between C16:0 and C18:0 (Fig. 5a).
In vitro fatty acid treatment changes the PD1+CD4+ and CXCR3+CD4+ T-cells frequencies. a The differences in the rate of frequency change of PD1+CD4+ T-cells after treatment C16:0 or C16:1n7, and CXCR3+CD4+ T-cell after treatment of C16:0 or C18:0 are shown. Comparison between the two groups was analyzed by the Mann–Whitney U test. b, c The rate of change for each T-cell subset is shown, as the fatty acid composition ratio is artificially increased from 0.05 to 0.5. We defined change rate of frequency as the ratio of frequencies before and after fatty acid treatment. A change rate of frequency > 1 denotes an increase in T-cell frequency upon fatty acid treatment, whereas a rate < 1 denotes a decrease in T-cell frequency. Frequency indicates the ratio of CD4+ T-cells expressing each surface antigen. The relations of C16:1n7/C16:0 (b), and C18:0/C16:0 c are shown. Comparison of change rate of each T-cell subset between two concentrations was analyzed by the Wilcoxon signed-rank test
We then artificially set the fatty acid composition ratio of C16:1n7/C16:0 and C18:0/C16:0 to 0.05 and 0.5, respectively, and analyzed the change in rate of the frequency for each T-cell subset. An increase in the fatty acid composition ratio of C16:1n7/C16:0 was correlated with a significant decrease in PD1+CD4+ T-cell frequency (Fig. 5b). However, no correlation between an increase in the fatty acid composition ratio of C18:0/C16:0 and the frequency of CXCR3+CD4+ T-cells was found (Fig. 5c).
T-cells in the liver change with fibrosis progression in NAFLD patients
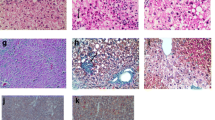
The number of CD4+ T-cells and CD8+ T-cells per unit area increased at each stage in the liver tissues of patients with progressing fibrosis (F0–1, n = 18 and F2–4, n = 12) (Fig. 6a, b).
T-cells in the liver change with fibrosis progression in NAFLD patients. The presence of CD4+ (a) and CD8+ T-cells (b) in the liver was assessed through immunohistochemistry (IHC). The number of CD4+ or CD8+ T-cells per unit area was compared between F0–1 (n = 18) and F2–4 (n = 12). Blue and red rectangle frames denote the lobular and portal areas, respectively. Comparison between the two groups was analyzed by the Mann–Whitney U test. c The presence of T-cells in the liver was analyzed by fluorescent multiplex IHC. Representative cases of F0–1 and F2–4 are shown. The IHC image is shown on the left. Phenotypes of subsets of T-cells are represented by colored dots on the right image. Corresponding colors were used in both images
Furthermore, we analyzed the presence of T-cells in the liver by flow cytometry (Supplemental Fig. 4) and fluorescent multiplex IHC (Fig. 6c). T-cells including FoxP3−CD25+CD4+ T-cell, PD1+CD4+ T-cell, and CXCR3+CD4+ T-cells were found.
Discussion
In the present study, we conducted comprehensive analyses of peripheral blood T-cell profiles of NAFLD patients and analyzed the in vivo and in vitro association of these profiles with fatty acids.
The peripheral T-cell profiles of healthy volunteers and NAFLD patients differed. Previous studies have shown that T-cells with effector functions are involved in the pathology of NAFLD [21, 22], and that T-cells expressing PD1 or CXCR3 are associated with organ fibrosis [23, 24]. Therefore, we focused on PD1+CD4+, CXCR3+CD4+, and CD25+CD45RA+CD4+ T-cells, the latter of which were activated before acquiring the effector function.
T-cells expressing the activation marker CD25, OX40 [25], or CD80 [26], and Th2 or Th17 cells that acquired effector function were significantly increased in NAFLD patients, suggesting immune activation (Fig. 1c, Supplementary Fig. 1b, c). CD25, the α-chain of the trimeric IL-2 receptor, is constitutively expressed in Treg cells expressing the master regulator gene FoxP3, but CD25 is also one of the T-cell activation markers [27]. The CD45RA+CD4+ T-cells in all 40 NAFLD patients were FoxP3 negative (Fig. 1a), and CD25 expression levels reflected activated T-cells. Antigen-stimulated Th1, Th2, and Th17 cells acquire effector functions after limited clonal expansion through further signaling. CD25 is expressed during this limited clonal expansion. Therefore, CD25+CD45RA+CD4+ T-cells are in a pre-activated stage [28]; yet, their differentiation fate has already been determined. Th1, Th2, or Th17 cells expressing master regulators T-bet, GATA3, or RORγt were included in the CD25+CD45RA+CD4+ T-cell subpopulation (Supplementary Fig. 2a). The increase in RORγt+ T-cells in NAFLD patients is consistent with previous studies reporting that Th17 cells are involved in the progression from non-alcoholic fatty liver (NAFL) to NASH [21] (Supplementary Fig. 2b). Similarly, T-cell activation in NAFLD patients are consistent with previous reports that the activation of CD4+ T-cells occurs in liver tissue in NAFLD mouse models [5, 6] and in peripheral blood cells in NAFLD patients [29].
PD1, a type I transmembrane protein, is an important regulator of immune homeostasis and tolerance. It is usually expressed in activated T-cells and suppresses T-cell proliferation and effector functions. Its upregulation of CD8+ T-cell potentially limits T-cell mediated liver damage in murine steatohepatitis [30]. In this study, the expression level of PD1 on CD25+CD45RA+CD4+ T-cells was low in NAFLD patients, despite the activation of the immune environment. This suggests that maintenance of immune homeostasis is impaired and that activated CD4+ T-cells are not properly regulated in NAFLD patients.
Liver fibrosis is known as a NAFLD prognostic factor [31]. It has been reported that the presence of ballooned hepatocytes is associated with fibrosis progression [32]. And, the gene expression levels in PBMCs are correlates with ballooning in NAFLD patients [33]. Furthermore, previous reports have shown that T-cells and surface antigens contribute to fibrosis through various mechanisms and exert both effects to promote or suppress fibrosis [34]. The activation of CD4+ T-cell affects the development of fibrocytes and is associated with renal fibrosis [35]. CXCR3 is involved in different antifibrogenic or profibrogenic functions in the liver depending on its ligand [24]. PD1 mediates the alleviation of pulmonary fibrosis by human mesenchymal stem cells [23]. The CD4+ T-cell activation and expression of such surface antigens involved in fibrosis on T-cells were also associated with liver fibrosis in NAFLD patients. In other words, decreases in the PD1+CD4+ and CXCR3+CD4+ T-cell frequencies and an increase in the CD25+CD45RA+CD4+ T-cell frequency were associated with liver fibrosis (Figs. 2, 3).
We evaluated whether fatty acids that increase in NAFLD patients [7, 36, 37] could be a factor that caused such immune conditions. In vivo analysis revealed that many fatty acids were associated with various peripheral T-cell frequencies. Particularly, serum C16:1n7/C16:0 ratio, which is increased in NASH patients [18], was significantly negatively correlated with the PD1+CD4+ T-cell frequency (Fig. 4b). This indicates that fatty acids and T-cells are closely related in vivo and are possibly the factors that modify the T-cell profile of NAFLD patients.
To better understand this association, we analyzed T-cell profile changes in PBMCs upon in vitro fatty acid treatment. The changes in the PD1+CD4+ T-cells and CXCR3+CD4+ T-cells driven by in vitro treatment of fatty acids supported an in vivo relationship (Fig. 5a). By artificially modifying the fatty acid composition, our tests suggest that the relationship between the C16:1n7/C16:0 ratio and PD1+CD4+ T-cells was more specific (Fig. 5b). Fatty acid metabolism in T-cells largely influences their functions [11,12,13] and the expression of these surface antigens. PD1 causes lipolysis and β-oxidation of endogenous fatty acids in T-cells [38], and CXCR3 contributes to the regulation of lipogenesis in hepatocytes [24]. Thus, changes in the expression of these surface antigens due to the fatty acid treatments may be related to a change in lipid metabolism. This might explain the reason why the expression of PD1 on CD4+ T-cells is unsuitably downregulated despite the state of immune activation.
Our study might suggest a correlation between T-cells and fibrosis in NAFLD patients. However, further validation on a larger sample of patients with progressive fibrosis is required. In addition, changes found in the frequencies of liver tissue T-cells depending on the fibrosis stage suggest that T-cells might affect liver fibrogenesis (Fig. 6). The finding that the portal inflammatory infiltrate may directly contribute to fibrogenesis [39] might support our results. Nevertheless, our study does not prove a direct relation between peripheral blood and liver tissue T-cells.
In conclusion, T-cell profiles in NAFLD patients differed from healthy volunteers. It is suggested that fatty acids directly modify the T-cell profiles and are involved in pathogenesis such as liver fibrosis in NAFLD patients.
Abbreviations
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- CD:
-
Cluster of differentiation
- PBMCs:
-
Peripheral blood mononuclear cells
- NAS:
-
NAFLD activity score
- RPMI:
-
Roswell Park Memorial Institute
- FSC:
-
Fetal calf serum
- Treg :
-
Regulatory T-cell
- FoxP3:
-
Forkhead box P3
- T-bet:
-
T-box expressed in T-cells
- RORγt:
-
Retinoic acid-related orphan receptor gamma t
- Th:
-
T-helper
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated protein 4
- PD-1:
-
Programmed death 1
- CXCR3:
-
C-X-C motif chemokine receptor 3
- CCR4:
-
C–C motif chemokine receptor 4
- IHC:
-
Immunohistochemistry
- DAPI:
-
4′6-Diamidino-2-phenylindole
- NAFL:
-
Non-alcoholic fatty liver
References
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–90.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from American Association for the Study of Liver Disease. Hepatology. 2018;67:328–57.
Racanelli V, Rehermann B. The liver as an immunological organ. Hepatology. 2006;43:S54–S64.
Henning JR, Graffero CS, Rehman A, et al. Dendritic cells limit fibroinflammatory injury in nonalcoholic steatohepatitis in mice. Hepatology. 2013;58:589–602.
Ma C, Kesarwala AH, Eggert T, et al. NAFLD causes selective CD4(+) T lymphocyte loss and promotes hepatocarcinogenesis. Nature. 2016;531:253–7.
Sutti S, Jindal A, Locatelli I, et al. Adaptive immune responses triggered by oxidative stress contribute to hepatic inflammation in NASH. Hepatology. 2014;59:886–97.
Yamada K, Mizukoshi E, Sunagozaka H, et al. Characteristic of hepatic fatty acid compositions in patients with nonalcoholic steatohepatitis. Liver Int. 2015;35:582–90.
Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implication. Gastroenterology. 2012;142:711–25.
Akazawa Y, Nakao K. To die or not to die: death signaling in nonalcoholic fatty liver disease. J Gastroenterol. 2018;53:893–906.
Cazanave SC, Mott JL, Bronk SF, et al. Death receptor 5 signaling promotes hepatocytes lipoapoptosis. J Biol Chem. 2011;286:39336–48.
de Jong AJ, Kloppenburg M, Toes RE, et al. Fatty acids, lipid mediators, and T-cell function. Front Immunol. 2014;13:483.
Howie D, Ten Bokum A, Necula AS, et al. The role of lipid metabolism in T lymphocyte differentiation and survival. Front Immunol. 2018;8:1949.
Lochner M, Berod L, Sparwasser T. Fatty acid metabolism in the regulation of T cell function. Trends Immunol. 2015;36:81–91.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Mizukoshi E, Nakamoto Y, Marukawa Y, et al. Cytotoxic T cell responses to human telomerase reverse transcriptase in patients with hepatocellular carcinoma. Hepatology. 2006;43:1284–94.
Rosenblum MD, Way SS, Abbas AK. Regulatory T cell memory. Nat Rev Immunol. 2016;16:90–101.
Marra F, Svegliati-Baroni G. Lipotoxicity and the gut-liver axis in NASH pathogenesis. J Hepatol. 2018;68:280–95.
Yamada K, Mizukoshi E, Seike T, et al. Serum C16:1n7/C16:0 ratio as a diagnostic marker for non-alcoholic steatohepatitis. J Gastroenterol Hepatol. 2019;34:1829–35.
Cury-Boaventura MF, Pompeia C, Curi R. Comparative toxicity of oleic acid and linoleic acid on human lymphocytes. Life Sci. 2006;78:1448–566.
Altan M, Pelekanou V, Schalper KA, et al. B7–H3 expression in NSCLC and its association with B7–H4, PD-L1 and tumor-infiltrating lymphocyte. Clin Cancer Res. 2017;23:5202–9.
Rau M, Schilling AK, Meertens J, et al. Progression from nonalcoholic fatty liver to nonalcoholic steatohepatitis is marked by a higher frequency of Th17 cells in the liver and an increased Th17/resting regulatory T cell ration in peripheral blood and in the liver. J Immunol. 2016;196:97–105.
Inzaugarat ME, Ferreyra Solari NE, Billordo LA, et al. Altered phenotype and functionality of circulating immune cells characterize adult patients with nonalcoholic steatohepatitis. J Clin Immunol. 2011;31:1120–30.
Ni K, Liu M, Zheng J, et al. PD1/PD-L1 pathway mediates the alleviation of pulmonary fibrosis by human mesenchymal stem cells in humanized mice. Am J Respir Cell Mol Biol. 2018;58:684–95.
Zhang X, Han J, Man K, et al. CXC chemokine receptor 3 promotes steatohepatitis in mice through mediating inflammatory cytokines, macrophages and autophagy. J Hepatol. 2016;64:160–70.
Mallett S, Fossum S, Barclay AN. Characterization of the MRC OX40 antigen of activated CD4 positive T lymphocytes—a molecule related to nerve growth factor receptor. EMBO J. 1990;9:1063–8.
Sabzevari H, Kantor J, Jaigirdar A, et al. Acquisition of CD80 (B7–1) by T cells. J Immunol. 2005;166:2505–13.
Malek TR. The biology of interleukin-2. Annu Rev Immunol. 2008;26:453–79.
Malek TR, Bayer AL. Tolerance, not immunity, crucially depends on IL2. Nat Rev Immunol. 2004;4:665–74.
Inzaugarat ME, Ferreyra Solari NE, Billordo LA, Abecasis R, Gadano AC, Chernavsky AC. Altered phenotype and functionality of circulating immune cells characterize adult patients with nonalcoholic steatohepatitis. J Clin Immunol. 2011;31:1120–30.
Penna A, Pilli M, Zerbini A, et al. Dysfunction and functional restoration of HCV-specific CD8 responses in chronic hepatitis C virus infection. Hepatology. 2007;45:588–601.
Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65:1557–655.
Kakisaka K, Suzuki Y, Fujiwara Y, et al. Evaluation of ballooned hepatocytes as a risk factor for future progression of fibrosis in patients with non-alcoholic fatty liver disease. J Gastroenterol. 2018;53:1285–91.
Kado A, Tsutsumi T, Enooku K, et al. Noninvasive diagnostic criteria for nonalcoholic steatohepatitis based on gene expression levels in peripheral blood mononuclear cells. J Gastroenterol. 2019;54:730–41.
Pellicoro A, Ramachandran P, Iredale JP, et al. Liver fibrosis and repair: immune regulation of wound healing in a solid organ. Nat Rev Immunol. 2014;14:181–94.
Niedermeier M, Reich B, Rodriguez Gomez M, et al. CD4+ T cells control the differentiation of Gr1+ monocytes into fibrosis. Proc Natl Acad Sci USA. 2009;106:17892–7.
Fujita K, Nozaki Y, Wada K, et al. Dysfunctional very-low-density lipoprotein synthesis and release is a key factor in nonalcoholic steatohepatitis pathogenesis. Hepatology. 2009;50:772–80.
de Almeida IT, Cortez-Pinto H, Fidalgo G, et al. Plasma total and free fatty acids composition in human non-alcoholic steatohepatitis. Clin Nutr. 2002;21:219–23.
Patsoukis N, Bardhan K, Chatterjee P, et al. PD-1 alters T-cell metabolic reprogramming by inhibiting glycolysis and promoting lipolysis and fatty acid oxidation. Nat Commun. 2015;26:6692.
Gadd VL, Skoien R, Powell EE, et al. The portal inflammatory infiltrate and ductular reaction in human nonalcoholic fatty liver disease. Hepatology. 2014;59:1393–405.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Seike, T., Mizukoshi, E., Yamada, K. et al. Fatty acid-driven modifications in T-cell profiles in non-alcoholic fatty liver disease patients. J Gastroenterol 55, 701–711 (2020). https://doi.org/10.1007/s00535-020-01679-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-020-01679-7