Abstract
Background
The prevalence of non-alcoholic fatty liver disease (NAFLD) has increased. Non-alcoholic steatohepatitis (NASH) shows progression of liver fibrosis in NAFLD. It remains unclear which patients with NAFLD will show progression of liver fibrosis. Therefore, we aimed to investigate the risk factor associated with the progression of liver fibrosis among patients with NAFLD.
Methods
This observational study enrolled 157 patients with biopsy-proven NAFLD. Thirty-two patients were excluded because of lack of data. The accuracy of the formulae for estimating liver fibrosis, i.e., the FIB-4 index, APRI, and Forns index, was compared. Using serial changes of the best formula for liver fibrosis, we identified factors associated with the progression of liver fibrosis. Histological liver fibrosis was quantified using the Brunt stage.
Results
Sixty-three patients were diagnosed as having NASH. The FIB-4 index provided the best diagnostic accuracy for liver fibrosis [Brunt stage 0 versus 1–4, areas under the curve (AUC) 0.74; 0–1 versus 2–4, AUC 0.77; 0–2 versus 3–4, AUC 0.78; and 1–3 versus 4, AUC 0.87]. The association between body mass index, sex, observation period, and histological findings (liver fat content, bridging fibrosis, and hepatocyte ballooning) with the change in the FIB-4 index was evaluated among patients with NASH, using multivariate analysis. Among these factors, hepatocyte ballooning was associated with an increase in the FIB-4 index.
Conclusion
The FIB-4 index was the best formula for estimating liver fibrosis in patients with biopsy-proven NAFLD, and the presence of ballooned hepatocytes was a risk factor for the progression of liver fibrosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD), which manifests as the liver form of metabolic syndrome, is a severe health issue because the prevalence of NAFLD has strikingly increased in western countries [1]. Non-alcoholic steatohepatitis (NASH) is a stage of NAFLD that shows progression of fibrosis due to inflammation [2]. Because of the increased prevalence of NAFLD, NASH has been focused on as the cause of liver cirrhosis [1]. Since fibrosis is associated with mortality in patients with NASH [3], anti-fibrosis is considered as a therapeutic target for NASH.
Although NASH is characterized by inflammation and fibrosis in the liver, the histological hallmark of NASH is ballooning of the hepatocytes [4, 5]. Indeed, Matteoni et al. reported that the presence of ballooned hepatocytes is associated with patients’ prognosis [5]. However, diagnostic criteria for ballooned hepatocytes vary among pathologists; therefore, these findings might be subjective [6, 7]. Ballooned hepatocytes are significant in the pathophysiology of NASH, although they may be difficult to be objectively used as the diagnostic hallmark of NASH.
Fibrosis of the liver can be objectively evaluated using elastography [8, 9]. Magnetic resonance (MR) elastography and transient elastography are now available for evaluating fibrosis. Although these methods are non-invasive, repeatable, and safe, elastography requires expensive equipment. Since the prevalence of NAFLD is increasing among individuals in western countries, the assessment of fibrosis using several serum laboratory data and general information is also useful for general physicians. Several formulae calculated by laboratory data, such as the Fibrosis 4 (FIB-4) index and Forns index, have been proposed for the evaluation of liver fibrosis [10,11,12].
Several clinical trials have investigated the pharmacologic treatment of NASH [13]. Because the prevalence of NASH has drastically increased and use of a new therapeutic agent is expensive in general [14], the medical cost for NASH is incalculable. To reduce the medical cost and increase the efficacy of treatment for NASH, patients with NASH who require treatment need to be identified. Specifically, patients with NAFLD at risk for progression of liver fibrosis in the future need to be identified. Therefore, we aimed to investigate the risk factor associated with the progression of liver fibrosis among patients with NAFLD.
Materials and methods
Patients
One hundred fifty-seven consecutive patients who were diagnosed as having NAFLD by liver biopsy between December 2008 and March 2016 were screened for the present study (Fig. 1). Seven of the 157 patients eligible for the study were excluded because of an incomplete dataset. An additional 25 of the 157 patients were excluded because either the observation period was < 12 months or they voluntarily withdrew from the study.
Informed consent was obtained from all patients. All protocols reported in this study were approved by the Institutional Review Board of Iwate Medical University (approval number: H27-56).
To evaluate the accuracy of several formulae, which are described later, histological findings of fibrosis were compared (part 1 of the study). The factor associated with a change in the value, as calculated by the best formula for evaluating liver fibrosis, was evaluated. To evaluate the risk factor associated with the progression of liver fibrosis, the formula that predicted accurate fibrosis stage was used to assess fibrosis during the last visit in our department (part 2 of the study). The difference between the value at the last visit and that at liver biopsy was considered as a change in the fibrotic state.
Measurements and calculations
Body mass index (BMI) was calculated using the following formula: BMI = weight (kg)/(height × height) (m2). The aspartate transaminase (AST) to platelet ratio index (APRI) [12], FIB-4 index [11], and Forns index [10] were calculated using the following formulae:
-
APRI = \( \left\{ {\frac{{{\text{AST}} \left( {{\text{acutual}} {\text{value}}} \right)}}{{{\text{AST}} \left( {{\text{upper}} {\text{limit}} {\text{of}} {\text{normal}}} \right)}}} \right\}/{\text{platelet}} {\text{count}} (10^{9} /{\text{L}}) \).
-
FIB-4 index = \( \{ {\text{Age}} ({\text{years}}) \times {\text{AST}}\} /\{ {\text{platelet}} {\text{count}} (10^{9} /{\text{L}}) \times \surd {\text{ALT}}\} \).
-
Forns index = \( 7.811 - 3.131 \times {\text{Ln}}({\text{platelet count }}\left( {10^{9} /{\text{L}}} \right) + 0.781 \times {\text{Ln}}\left( {{\text{gamma - glutamyl transferase }}[]} \right) + 3.467 \times {\text{Ln}}\left( {\text{age}} \right) - 0.014 \times {\text{total cholesterol }}({\text{TC}}) \).
To evaluate insulin resistance, homeostatic model assessment for insulin resistance (HOMA-IR) was used. These values were calculated using the following formula:
-
HOMA-IR = \( {\text{insulin}} \times {\text{fasting glucose level}}/405 \).
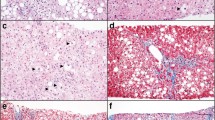
Liver biopsies and histological assessments
Percutaneous needle biopsies were performed on liver segment 6 under ultrasonography, using a 16-gauge (G) needle. To diagnose NAFLD or NASH definitively, all liver biopsy specimens were examined for fibrosis, steatosis, ballooning hepatocytes, and portal inflammation. Although these findings were scored using the NAFLD activity score [15], we evaluated whether ballooning was absent or present to avoid subjective grading of ballooning hepatocytes. NASH was defined based on the following findings: (1) more than 5% of fat in the liver and (2) existence of inflammation in any zone of the liver. NAFL was defined as more than 5% of fat in the liver without inflammation. Histological findings were evaluated by a single pathologist who was blinded to the patients’ clinical characteristics. The fibrosis stage was classified using the Brunt staging system. Because the patients in this study had NAFL and fibrosis was absent in NAFL, NAFL was classified as Brunt stage 0.
Laboratory data
All blood samples were collected on the day of liver biopsy and at every visit to our unit. The levels of AST, alanine transaminase (ALT), γ-GT, fasting glucose, ferritin, insulin, type IV collagen (T4C7s), and TC were analyzed using an autoanalyzer (JCA-BM2250, JEOL, Tokyo, Japan).
Statistical analysis
Continuous variables are presented as mean ± standard deviation. The Mann–Whitney U test was used to compare the laboratory data, BMI, and age between patients with NAFLD who were divided into the NASH and NAFL groups. The diagnostic performance of the formula for detecting the Brunt stage was assessed using the receiver-operating characteristic (ROC) curve method. The cut-off values of the APRI, FIB-4 index, and Forns index in each analysis were estimated using the area under the ROC (AUROC). After evaluating the performance of each formulae used to assess fibrosis in part 1 of the study, serial change of the best formula was calculated for the patients in part 2 of the study. Because the best formula contained laboratory data and age, linear regression analysis of serial change in the value of the formula was analyzed in BMI, sex, age, body weight (BW) change during the observation period, the observation period, and histological findings (fat in the liver, bridging fibrosis, and ballooned hepatocytes). Serial change of the formula was defined as delta: (formula using data at the day of biopsy) − (formula using data at the day of the last visit). All statistical analyses were performed using the SPSS 17.0 software program (SPSS Inc., Chicago, IL, USA). Results were considered significant when the p value was < 0.05.
Results
Patients’ characteristics
The relevant characteristics of patients are summarized in Table 1. Based on histological findings, 62 patients were sub-classified in the NAFL group, and 63 were sub-classified in the NASH group. The two groups were comparable with regard to the BMI distribution. Distributions of Brunt stages in the NASH group were as follows: stage 1, 23 patients; stage 2, 14 patients; stage 3, 21 patients; and stage 4, 5 patients. Among patients in the NASH group, bridging fibrosis was identified in 17, and ballooning hepatocytes were identified in 49. Patients were older in the NASH group (mean age, 54.9 years) than in the NAFL group (mean age, 46.6 years). Levels of the following serum markers were higher in the NASH group than in the NAFL group: AST, 62 versus 51 IU/mL; ferritin, 248 versus 224 mg/dL; glycated hemoglobin, 6.2 versus 5.7%; and T4C7s, 6.09 versus 3.91 ng/mL. However, the platelet count was lower in the NASH group than in the NAFL group (213 versus 234 × 104). There were no between-group differences with regard to the levels of ALT, TC, insulin, and HOMA-IR. As expected, fibrosis scores were higher in the NASH group than in the NAFL group: FIB-4 index, 1.04 versus 2.03; APRI, 0.56 versus 1.05; and Forns index, 5.24 versus 6.48.
FIB-4 index had the best diagnostic accuracy of liver fibrosis
Although each formula used to estimate liver fibrosis showed a high value among the subjects, it remained unclear which formula accurately evaluated the fibrosis stage. To evaluate serial change of fibrosis during the observation period, we needed to identify the best formula for evaluating liver fibrosis. For this purpose, the diagnostic accuracy of each formula was evaluated among the patients with NAFLD in the NASH and NAFL groups using the ROC curve method. To identify the patients with Brunt stage 0, the FIB-4 index, APRI, and Forns index showed AUROCs of 0.743, 0.748, and 0.672 when the cut-off values of each formula were 1.33, 0.68, and 6.04, respectively (Fig. 2a). To distinguish the patients with Brunt stages 0–1 and 2–4, the FIB-4 index, APRI, and Forns index showed AUROCs of 0.765, 0.708, and 0.706 when the cut-off values of each formula were 1.40, 0.65, and 6.45, respectively (Fig. 2b). To determine the patients with Brunt stage 3–4 (advanced fibrosis), the FIB-4 index, APRI, and Forns index showed AUROCs of 0.781, 0.763, and 0.681 when the cut-off values of each formula were 1.62, 0.76, and 6.45, respectively (Fig. 2c). To identify the patients with Brunt stage 4, the FIB-4 index, APRI, and Forns index showed AUROCs of 0.870, 0.732, and 0.892 when the cut-off values of each formula were 1.73, 1.57, and 7.40, respectively (Fig. 2d). All formulae in each analysis showed a relatively high AUROC, high sensitivity, and high specificity. However, the cut-off value of the FIB-4 index was consistent in each analysis, while those of the other indices were inconsistent among each analysis. Therefore, we used the FIB-4 index to evaluate the serial change of fibrosis during the observation period.
Diagnostic accuracy of the Fibrosis 4 (FIB-4) index, aspartate transaminase to platelet ratio index (APRI), and Forns index according to the Brunt stage. a–d Diagnostic accuracy of the FIB-4 index, APRI, and Forns index was assessed using the receiver operating characteristic (ROC) curve method, and the results are expressed as the area under the ROC curve (AUROC). The cut-off value was estimated by the Youden index. Using each cut-off value, sensitivity, specificity, the positive predictive value (PPV), and negative predictive value (NPV) were estimated. Each graph reveals the ROC curve for Brunt stage 0 versus 1–4 (a), 0–1 versus 2–4 (b), 0–2 versus 3–4 (c), and 1–3 versus 4 (d)
No factors were associated with serial change of liver fibrosis
Since the FIB-4 index showed the most accurate estimation of liver fibrosis in this study, we considered that serial change of the FIB-4 index, i.e., delta FIB-4 index, might reflect fibrotic change of the liver in our study patients. To identify factors associated with the progression of liver fibrosis, linear regression analysis for the delta FIB-4 index in all patients was performed using BMI, sex, age, BW change during the observation period, the observation period, and histological findings (fat in the liver, bridging fibrosis, and ballooned hepatocytes). None of the factors was identified in this analysis (data not shown).
Longer observation period and presence of ballooned hepatocytes were associated with the progression of liver fibrosis
Considering the natural progression of NAFLD, NASH will eventually become the more progressive type of liver fibrosis. Therefore, linear regression analysis of the delta FIB-4 index was performed separately in the NAFL and NASH groups. Because the NAFL group did not show histological findings associated with liver fibrosis, bridging fibrosis and ballooned hepatocytes were not included in this analysis. The observation period was negatively associated with the delta FIB-4 index in the NAFL group (Table 2; t = − 2.621, p = 0.011). Regarding the NASH group, linear regression analysis of the delta FIB-4 index was analyzed using BMI, sex, age, BW change during the observation period, the observation period, and histological findings (fat in the liver, bridging fibrosis, and ballooned hepatocytes). The presence of ballooned hepatocytes was negatively associated with the delta FIB-4 index in the NASH group (Table 2; t = − 2.371, p = 0.023). To confirm the relationship between ballooned hepatocytes and liver fat, the liver fat volume was compared with the presence of ballooned hepatocytes or the grading of ballooned hepatocytes. Neither the presence of ballooned hepatocytes nor the grading of ballooned hepatocytes was associated with the liver fat volume (Supplemental Fig. 1A, B).
Discussion
The clinically significant findings of this study were as follows: (1) the FIB-4 index was the best formula for estimating liver fibrosis in patients with biopsy-proven NAFLD and (2) presence of ballooned hepatocytes predicted the progression of liver fibrosis in the future.
The prevalence of NAFLD is increasing among individuals in the developed countries [1]. The aggressive form of NAFLD, NASH, leads to the progression of liver fibrosis and results in liver cirrhosis [2]. Although the malignant potential of NASH has been recognized, the adequate approach for treating patients with NAFLD remains unclear. As the first step in establishing the treatment strategy for NASH, patients with NAFLD who show progression of liver fibrosis need to be identified. In this study as well as in previous studies [16, 17], the FIB-4 index showed accurate estimation of liver fibrosis in patients with NAFLD. Therefore, the FIB-4 index will be useful for assessing liver fibrosis when a general physician evaluates patients with NAFLD using laboratory data without imaging findings.
Advanced fibrosis of the liver is a distinct issue because cirrhotic liver will be the cause of liver failure and/or hepatocellular carcinoma [3]. Although no factor associated with the progression of liver fibrosis was isolated from all patients with NAFLD in this study, the observation period in the NAFL group and presence of ballooned hepatocytes in the NASH group were associated with the progression of liver fibrosis. The patients with NAFL who showed normalization of the liver enzyme after nutritional intervention were followed in up this study, and those with an abnormal liver enzyme level were followed for longer periods. Thus, the observation period in the NAFL group was identified as a risk factor for the progression of liver fibrosis because of selection bias. In contrast, the presence of ballooned hepatocytes was not associated with any bias, and it is considered a clear risk factor associated with the progression of liver fibrosis.
Ballooned hepatocytes are considered a diagnostic hallmark of NASH, and they have a key role in the pathophysiology of NASH [2, 4, 18, 19]. Hepatocytes without cell death under lipotoxicity show a morphological similarity to ballooned hepatocytes [20, 21]. Furthermore, these cells secrete a fibrogenic chemokine, sonic hedgehog (SHH), which affects cell survival under an autocrine mechanism [20]. Recently, autophagic impairment was observed in a NASH model [22]. Intriguingly, the morphological likeness of ballooned hepatocytes was required with autophagic impairment [21]. Lipotoxicity, i.e., the incomplete execution of cell death and impairment of the autophagic process, may lead to the ballooning of hepatocytes. In this study, ballooned hepatocytes were not associated with liver fat, and fibrosis progressed in the liver with the ballooning of hepatocytes. Thus, ballooned hepatocytes might be a therapeutic target in patients with NASH. Further study for the interaction between ballooned hepatocytes and the pathophysiology of NASH is necessary.
We recognize that this study has limitations. The evaluation of liver fibrosis in this study was not highly accurate. However, the FIB-4 index reflected the whole liver condition because the results were calculated using laboratory data. Yet, the liver biopsy had a possibility of sampling error [23]. Although the FIB-4 index did not show a high accuracy in the histological grade of liver fibrosis, the delta FIB-4 index was the difference of each result of the FIB-4 index, and the result might have been associated with a simple change of the whole-liver condition in this study. To confirm this speculation, the delta FIB-4 index should be confirmed in a future study with other modalities, such as transient elastography or MR elastography, to evaluate liver fibrosis. We also noticed a limitation associated with the evaluation of liver fibrosis. Although transient elastography has been recognized as a useful examination for evaluating liver fibrosis [24, 25], these data are absent in this study. We are now collecting the date of transient elastography, but we do not have sufficient data regarding the use of transient elastography in this setting. Thus, we cannot confirm the degree of liver fibrosis using transient elastography. Sampling error caused by liver biopsy should be carefully considered in the histological evaluation of conditions such as fibrosis, ballooned hepatocytes, and steatosis. Although multi-sampling from the same liver tissue would improve the accuracy of the histological evaluation, we obtained a single sample from each liver biopsy. Therefore, more accurate evaluation of ballooning based on multiple sampling may be needed to confirm our findings in the future. We also need to mention the limitation associated with the serum marker of liver fibrosis. Recently, Mac-2 binding protein glycan isomer (M2BPGi) has been reported as a useful marker for detecting liver fibrosis [26,27,28]. Although we need to confirm a correlation between M2BPGi and liver fibrosis in this setting, we did not evaluate this relationship because we did not keep serum samples of the subjects. To avoid subjective bias for the diagnosis of ballooned hepatocytes, the presence or absence of ballooned hepatocytes was considered in this study. Thus, the evaluation of ballooned hepatocytes was not quantitative in this study. Therefore, the meaning of the presence of ballooned hepatocytes and the pathophysiology of NASH remains unclear.
We concluded that the FIB-4 index was the best formula for estimating the progression of liver fibrosis in patients with biopsy-proven NAFLD, and the presence of ballooned hepatocytes was a risk factor for the progression of liver fibrosis.
Abbreviations
- ALT:
-
Alanine transaminase
- APRI:
-
Aspartate transaminase to platelet ratio index
- AST:
-
Aspartate transaminase
- AUROC:
-
Area under the receiver operating characteristic
- BF:
-
Bridging fibrosis
- BH:
-
Ballooned hepatocyte
- BMI:
-
Body mass index
- FIB-4:
-
Fibrosis 4
- γGT:
-
Gamma-glutamyl transferase
- HOMA-R:
-
Homeostatic model assessment for insulin resistance
- M2BPGi:
-
Mac-2 binding protein glycan isomer
- MR:
-
Magnetic resonance
- NAFL:
-
Non-alcoholic fatty liver
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- ROC:
-
Receiver operating characteristic
- SHH:
-
Sonic hedgehog
- T4C7s:
-
Type 4 collagen 7s
- TC:
-
Total cholesterol
References
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84.
Machado MV, Diehl AM. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology. 2016;150(8):1769–77.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149(2):389 e10–397 e10.
Caldwell S, Ikura Y, Dias D, et al. Hepatocellular ballooning in NASH. J Hepatol. 2010;53(4):719–23.
Matteoni CA, Younossi ZM, Gramlich T, et al. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413–9.
Sumida Y, Nakajima A, Itoh Y. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014;20(2):475–85.
Younossi ZM, Gramlich T, Liu YC, et al. Nonalcoholic fatty liver disease: assessment of variability in pathologic interpretations. Mod Pathol. 1998;11(6):560–5.
Bota S, Herkner H, Sporea I, et al. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int. 2013;33(8):1138–47.
Singh S, Venkatesh SK, Loomba R, et al. Magnetic resonance elastography for staging liver fibrosis in non-alcoholic fatty liver disease: a diagnostic accuracy systematic review and individual participant data pooled analysis. Eur Radiol. 2016;26(5):1431–40.
Forns X, Ampurdanes S, Llovet JM, et al. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology. 2002;36(4 Pt 1):986–92.
Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–25.
Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518–26.
Banini BA, Sanyal AJ. Current and future pharmacologic treatment of nonalcoholic steatohepatitis. Curr Opin Gastroenterol. 2017;33(3):134–41.
Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–21.
Shah AG, Lydecker A, Murray K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104–12.
Sumida Y, Yoneda M, Hyogo H, et al. Validation of the FIB4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol. 2012;12:2.
Hirsova P, Gores GJ. Ballooned hepatocytes, undead cells, sonic hedgehog, and vitamin E: therapeutic implications for nonalcoholic steatohepatitis. Hepatology. 2015;61(1):15–7.
Machado MV, Cortez-Pinto H. Cell death and nonalcoholic steatohepatitis: where is ballooning relevant? Expert Rev Gastroenterol Hepatol. 2011;5(2):213–22.
Kakisaka K, Cazanave SC, Werneburg NW, et al. A hedgehog survival pathway in ‘undead’ lipotoxic hepatocytes. J Hepatol. 2012;57(4):844–51.
Suzuki A, Kakisaka K, Suzuki Y, et al. c-Jun N-terminal kinase-mediated Rubicon expression enhances hepatocyte lipoapoptosis and promotes hepatocyte ballooning. World J Gastroenterol. 2016;22(28):6509–19.
Amir M, Czaja MJ. Autophagy in nonalcoholic steatohepatitis. Expert Rev Gastroenterol Hepatol. 2011;5(2):159–66.
Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128(7):1898–906.
Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48(5):835–47.
Tapper EB, Castera L, Afdhal NH. FibroScan (vibration-controlled transient elastography): where does it stand in the united states practice. Clin Gastroenterol Hepatol. 2015;13(1):27–36.
Kuno A, Ikehara Y, Tanaka Y, et al. A serum “sweet-doughnut” protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci Rep. 2013;3:1065.
Narimatsu H. Development of M2BPGi: a novel fibrosis serum glyco-biomarker for chronic hepatitis/cirrhosis diagnostics. Expert Rev Proteom. 2015;12(6):683–93.
Shirabe K, Bekki Y, Gantumur D, et al. Mac-2 binding protein glycan isomer (M2BPGi) is a new serum biomarker for assessing liver fibrosis: more than a biomarker of liver fibrosis. J Gastroenterol. 2018. https://doi.org/10.1007/s00535-017-1425-z
Acknowledgements
This study was supported by KAKENHI Grant no. JP16K21307 and the Keiryokai Research Foundation Grant no. Y117.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2018_1468_MOESM1_ESM.pptx
Supplemental Fig. 1. Difference of liver fat volume according to ballooned hepatocytes. A and B: Distribution of the liver fat volume among subjects divided by the presence or absence of ballooned hepatocytes (A) or the grading of ballooned hepatocytes (B). (PPTX 73 kb)
Rights and permissions
About this article
Cite this article
Kakisaka, K., Suzuki, Y., Fujiwara, Y. et al. Evaluation of ballooned hepatocytes as a risk factor for future progression of fibrosis in patients with non-alcoholic fatty liver disease. J Gastroenterol 53, 1285–1291 (2018). https://doi.org/10.1007/s00535-018-1468-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-018-1468-9