Abstract
Background
The risk:benefit ratio of concomitant use of thiopurines with scheduled adalimumab (ADA) maintenance therapy for Crohn’s disease is controversial. The aim of this study is to identify the influence of withdrawal of thiopurines in patients in remission with combination therapy in an open-label, randomised, controlled trial (DIAMOND2; UMIN000009596).
Methods
Patients in corticosteroid-free clinical remission (CFCR) for ≥ 6 months with ADA (40 mg, s.c., every other week) scheduled maintenance combined with thiopurines were randomised into two groups, “continue” (Con) or “discontinue” (Dis) group of thiopurines, whereas all other patients kept receiving scheduled ADA maintenance therapy for 52 weeks. The primary endpoint was the proportion of patients in CFCR at week 52. Secondary endpoints were endoscopic remission (ER), trough levels of ADA in serum, and safety.
Results
Fifty patients were randomised to Con or Dis groups. Characteristics of patients were not significantly different between the groups. CFCR and ER prevalence at week 52 were not significantly different between groups (log rank, P = 0.704, P = 1.000, respectively). Trough levels of ADA were not significantly different between groups (P = 0.515). The proportion of patients with AAA positivity at week 52 was not significantly different (P = 0.437). ER at week 0 was involved in ER and triple remission at week 52. No serious adverse effects were observed in either group.
Conclusion
Continuation of thiopurines > 6 months offers no clear benefit over scheduled ADA monotherapy. CFCR, ER, and ADA trough level at week 52 were not significantly different between groups. ER at week 0 may be involved in better long-term clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, anti-tumour necrosis factor (TNF)α monoclonal antibody (mAb) has become the main treatment for Crohn’s disease (CD) [1, 2]. Concomitant use of immunosuppressants with anti-TNFα mAb is controversial. In patients with biologic-naïve CD, a combination of the chimeric anti-TNFα mAb infliximab (IFX) with azathioprine (AZA) has shown clinical benefit [3]. Conversely, the continuation of thiopurines > 6 months has shown no clear benefit over scheduled IFX monotherapy [4].
Adalimumab (ADA) is a human anti-TNFα mAb, so antigenicity (which is a way of inducing anti-drug antibodies) seems to be weaker than that of IFX. Long-term use of thiopurines is a risk factor for opportunistic infections and development of malignancies [5]. Thus, the benefits and risks of combination therapy are controversial [6, 7].
A prospective randomised controlled trial comparing the efficacy of ADA monotherapy and combination therapy with AZA for CD patients naïve to biologic agents and thiopurines (DIAMOND study) did not show a benefit of concomitant use of AZA in the prevalence of clinical remission at week 26 as the primary endpoint [8]. However, concomitant use of AZA showed marginal benefits in generation of anti-adalimumab antibodies (AAAs) [9] and endoscopic improvement [10]. Considering these findings (especially for ADA), a suitable time for combination with thiopurines could be important.
The aim of the present multicentre, prospective, randomised, open-label study was to evaluate if continuing use of standard thiopurines in patients who had been responding to a combination of ADA and thiopurine for ≥ 6 months adds to the long-term efficacy of scheduled maintenance compared with ADA monotherapy.
Materials and methods
Ethical approval of the study protocol
The study protocol was approved by the Ethics Review Board at each institution and registered publicly (UMIN000009596). All patients provided verbal and written informed consent for blood testing and collection of clinical data before enrolment.
Patients
The DIAMOND2 was a multicentre, randomised, prospective, open-label study. Patients with CD who were in corticosteroid-free clinical remission (CFCR; Crohn’s Disease Activity Index (CDAI) < 150 [11]) with concomitant use of thiopurines with scheduled maintenance of ADA for ≥ 6 months were enrolled. The diagnosis of CD was based on criteria determined by the Japanese Ministry of Health, Labour and Welfare. The age range of patients was 15–65 years. Patients met all other inclusion criteria and none of the exclusion criteria.
Exclusion criteria were patients: (1) with a contraindication to anti-TNF-α (severe infection, active mycobacterial infection, past/present history of demyelinating disease, or clinically evident congestive heart failure); (2) with a contraindication for thiopurines (peripheral white blood cell count < 3000/ml); (3) who were pregnant or breastfeeding; (4) with a malignant neoplasm; (5) with an interval of < 6 months after their latest surgical procedure; (6) with short-bowel syndrome; (7) with an ileostomy or colostomy; (8) regarded as being unsuitable for the DIAMOND2 by the attending physician.
Study protocol
Each patient had CFCR for ≥ 6 months with scheduled maintenance using ADA (40 mg, s.c., e.o.w.) combined with thiopurines.
Patients assigned to the ‘continue’ (Con) group were treated further with ADA combined with oral thiopurines [AZA or 6-mercaptopurine (6-MP)] for 52 weeks. Patients assigned to the ‘discontinue’ (Dis) group received scheduled maintenance therapy using ADA for 52 weeks (Supplemental Figure 1).
The DIAMOND2 was an open-label study, so patients in the Dis group were not treated with a placebo either. Patients in the Con group were treated with 25–50 mg/day of AZA or 30 mg/day of 6-MP. The dose of thiopurines was maintained during investigation periods. The maintenance dose of thiopurines was chosen based on reports in Japanese patients with inflammatory bowel disease [12]. Follow-up data were collected several weeks after a patient completed the study at week 52 or immediately after withdrawal from the DIAMOND2. Randomisation was done centrally at the Clinical Research Centre within Keio University (Tokyo, Japan) using computer-generated randomisation system. All data were collected at the Clinical Research Centre within Keio University. During the investigation period, mesalazine (p.o.) or sulfasalazine (p.o) was maintained at a stable dose.
Efficacy and safety
CDAI scores were determined at weeks 0, 4, 12, 26 and 52. ‘Clinical recurrence’ was defined as an increase in the CDAI ≥ 70 from baseline and CDAI ≥ 150. Ileocolonoscopy was done at baseline and at week 52. The mucosal lesion at each ileocolonoscopy was assessed according to the Simple Endoscopic Score for Crohn’s Disease (SES-CD) [13]. Endoscopic images at sites of mucosal involvement were recorded as stills, and the SES-CD at each colonoscopy calculated by the attending physician. ‘Clinical remission’ was defined as a CDAI score < 150 [11]. Mucosal healing was defined as SES-CD ≤ 2 [10, 14]. Blood samples were collected from patients in both groups at weeks 0, 4, 12, 26, and 52. Blood samples were also collected if a patient withdrew from the study. The 6-thioguanine (6-TGN) concentration in red blood cells (RBCs) was measured at baseline (Con and Dis) and week 52 (Con). Samples of whole blood were collected in heparinised tubes and centrifuged. After removing plasma, RBCs were hydrolysed with acid and extracted with phenylmercuric acetate/ethyl acetate. 6-TGN levels were measured by high-performance liquid chromatography [15]. Trough levels of ADA and AAAs in serum were measured at baseline and week 52 in both groups. Enzymelinked immunosorbent assay (ELISA) and radio immunoassay were used to measure trough serum adalimumab concentrations and to detect the presence of anti-adalimumab antibodies by Sanquin (Amsterdam, the Netherlands). Based on manufacturer’s recommendations, a serum AAA level of ≥ 12 μg/ml was regarded as ‘positive’ for the antibody [16, 17].
Primary and secondary endpoints
The DIAMOND2 was designed to be a superiority trial. The primary efficacy endpoint was CFCR prevalence at week 52. Secondary efficacy endpoints were: the percentage of patients who showed a negative C-reactive protein (CRP) level; prevalence of mucosal healing (SES-CD ≤ 2) at week 52; serological remission (CRP ≤ 0.10 mg/dl) at week 52. Safety endpoints were the prevalence of: any adverse event during the study period; loss of response to ADA.
Statistical analyses
For the primary endpoint (CFCR prevalence at week 52), it was estimated that 90 patients in each group would be needed to attain a power of 80% to detect a difference in CFCR prevalence of 20% between Con and Dis groups (alpha = two-sided 5%). This calculation was based on the assumption that the CFCR prevalence would be 80% in the Con group and 60% in the Dis group at week 52.
Comparison between groups was done by Welch’s t test for continuous values, and Fisher’s exact test for categorical values. The difference in risk, relative risk, and proportion of each group with confidence intervals (CIs) was calculated for the primary endpoint. Significance was at the 5% level. The statistical power based on the number of people enrolled in the DIAMOND2 was 73.9% with the assumption of CFCR of 95% and 60% (alpha = two-sided 5%). Analyses were undertaken using SPSS v20 (IBM, Armonk, NY, USA).
Results
Study population
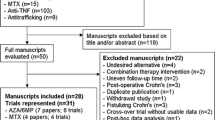
During the predetermined period of recruitment from 1 January 2013 to 31 December 2016, 53 patients were enrolled in the DIAMOND2. One patient relapsed before randomisation and was excluded. Fifty-two patients were randomised to the Con group (n = 23) or Dis group (n = 29). One patient in the Con group was excluded because the patient withdrew consent. One patient in the Dis group was excluded because the study was not carried out. Finally, 22 patients in the Con group and 28 patients in the Dis group were assessed (Supplemental Figure 2).
Twenty-one patients in the Con group and 27 patients in the Dis group completed the study in 52 weeks. One patient in the Con group and two patients in the Dis group withdrew from the study owing to an increase in disease activity. No patients in either group withdrew from the study owing to adverse effects. Table 1 summarises and compares the demographic data and baseline clinical characteristics of the study population between Con group and Dis groups.
Clinical outcomes
As a primary endpoint, CFCR prevalence at week 52 was not significantly different between the two groups. It was 95.5% (21/22, 95% CI 76.5–99.1%) in the Con group and 92.9% (26/28, 72.0–98.9%) in the Dis group (P = 1.000) (Fig. 1a). Kaplan–Meier analyses indicated that the time to CFCR was not significantly different between the two groups (log rank: P = 0.704) (Fig. 1b). Risk difference and relative risk between the groups was 2.6% (95% CI − 10.3–15.5%) and 1.03 (0.90–1.18), respectively.
Endoscopic outcomes
At baseline, the total SES-CD score (mean ± SD) was 5.46 ± 5.66 in the Con group and 4.39 ± 4.04 in the Dis group (P = 0.45). The prevalence of mucosal healing (SES-CD ≤ 2) at baseline was 63.6% (14/22) in the Con group and 57.7% (15/26) in the Dis group (P = 0.771) (Table 1). In patients who received ileocolonoscopy at week 0 and week 52, the total SES-CD score at week 52 was 5.81 ± 7.06 in the Con group and 6.54 ± 7.34 in the Dis group, and they were not significantly different (P = 0.942) (Fig. 2a). The proportion of patients with mucosal healing at week 52 was 30% (6/20) in the Con group and 32% (8/25) in the Dis group (P = 1.000) (Fig. 2b). Change in the SES-CD score at week 52 from baseline (mean ± SE) was 0.57 ± 0.97 in the Con group and 2.52 ± 0.96 in the Dis group (P = 0.162) (Fig. 2c). Worsening of endoscopic activity was observed in two patients in the Con group and two patients in the Dis group. Endoscopic improvement was observed in one patient in the Con group (SES-CD decreased from 11 at baseline to 0 at week 52) (data not shown).
Endoscopic evaluation. a The SES-CD score (mean ± SD) at week 52 in Con and Dis groups. b Proportion of the patients with endoscopic remission (SES-CD ≤ 2) at week 52. c The mean change in the SES-CD score at week 52 from baseline (∆SES-CD) (mean ± SD). Statistical analyses were by Welch’s t test. Con continue group, D discontinue group, SD standard deviation
Biological outcomes
At week 52, the proportion of patients with a negative CRP level (< 0.10 mg/dl) was 76.2% (16/21) in the Con group and 84.6% (22/26) in the Dis group (P = 0.711) (Fig. 3a). The change in the CRP level (mg/dl) at week 52 from baseline (mean ± SD) was 0.600 ± 1.574 in the Con group and 0.098 ± 0.535 in the Dis group (P = 0.164) (Fig. 3b).
Analyses of serum CRP levels (mg/dl) at week 52. a Proportion of patients with serological remission (CRP ≤ 0.10 mg/dl) at week 52. b Mean change in the CRP level at week 52 from baseline (∆CRP) (mean ± SD). Statistical analyses were by Welch’s t test. Con continue group, D discontinue group, SD standard deviation
‘Triple remission’ at week 52
The percentage of patients with triple remission (i.e., CFCR, endoscopic remission and a negative CRP level) at week 52 was 22.7% (5/22) in the Con and 28.6% (8/28) in the Dis group (P = 0.750) (Supplemental Figure 3).
Trough levels of ADA and AAA in serum
The trough level (mean ± SD) of ADA in serum (μg/ml) at week 52 was 7.08 ± 2.96 in the Con group and 6.48 ± 3.16 in the Dis group (P = 0.515) (Fig. 4a). The proportion of patients with AAA positivity at week 52 was 10.0% (2/20) in the Con group and 20.0% (5/25) in the Dis group (P = 0.437) (Fig. 4b). The three patients who suffered clinical relapse had AAA negativity when they relapsed. Among 44 patients who had AAA negativity at baseline, switching to AAA positivity during the observation period in three patients (one in the Con group and two in the Dis group) was noted. The trough level (mean ± SD) of ADA in serum (μg/ml) at week 52 was 4.02 ± 2.81 in patients with AAA- positivity and 7.38 ± 3.29 in patients with AAA negativity (P = 0.014) (Fig. 5a). Especially in patients with a high titre of AAAs, the trough level (mean ± SD) of ADA in serum was very low (Fig. 5b).
Correlation of the trough level of ADA in serum with AAA. a Trough level of ADA in serum (μg/ml) at week 52 in AAA-negative and AAA-positive patients (mean ± SD). b Scatter plot shows the trough concentration of ADA and AAA titre in each patient. Statistical analyses were by Welch’s t test. AAA anti-adalimumab antibody, ADA adalimumab, SD standard deviation
Endoscopic remission at week 0 and clinical outcomes at week 52
As described above, continuation of thiopurines > 6 months offers no clear benefit over the scheduled ADA monotherapy. We performed a sub-analysis to find out whether endoscopic activity at week 0 influenced the clinical outcomes (CFCR, endoscopic remission, serological remission, triple remission) at week 52 (Table 2). Endoscopic remission at week 0 was involved in endoscopic remission (P < 0.001) and triple remission (P < 0.001) at week 52 (Table 2).
Adverse effects
No patients in the Con group and two patients in the Dis group reported adverse effects (common cold), and serious adverse events were not observed in either group (Supplemental Table 1).
Discussion
The DIAMOND2 did not reveal a clear benefit of continuation of thiopurines > 6 months over scheduled ADA monotherapy. There was no difference in the primary endpoint (CFCR prevalence at week 52) between patients who received further concomitant use of thiopurines and patients for whom thiopurines were withdrawn. At week 52, continuation of thiopurines did not show benefit with regard to the serum level of CRP, endoscopic activity, triple remission, or trough level of ADA in serum. Only a change in the SES-CD at week 52 from baseline tended to be higher in the Dis group. The trough level of ADA decreased in patients who were AAA positive.
The benefit of concomitant use of thiopurines in scheduled maintenance therapy using anti-TNFα mAb is controversial. In the Study of biologic and immunomodulator naive patients in Crohn’s Disease (SONIC) study, the combination of IFX with AZA showed clinical benefit with regard to the prevalence of clinical remission at week 26 and appearance of anti-IFX antibodies [3]. Conversely, combination of ADA with thiopurines in biologic-naïve CD patients (DIAMOND study) did not show benefit in clinical remission at week 26 as the primary endpoint [8]. However, sub-analysis of the DIAMOND study suggested that concomitant use of AZA showed some clinical benefit in terms of inhibition of AAA induction and endoscopic improvement [9, 10]. Those findings suggested marginal benefits of concomitant use of thiopurines with anti-TNFα mAbs, even in humanised mAb ADA, as induction therapy in biologic-naïve patients. With regard to generation of anti-drug antibodies, aggressive disease could inhibit the induction of anti-drug antibodies, whereas the risk of induction of anti-drug antibodies could be lower in patients with clinical remission. Hence, concomitant use of thiopurines with ADA in the acute phase of disease may be beneficial.
The benefits and risks of long-term concomitant use of immunosuppressants with anti-TNF mAbs in patients in clinical remission are also controversial. The effects of withdrawal of immunosuppressant therapy in people with quiescent CD are not known [18].
Long-term, strict immunosuppression could be a risk factor for infection and development of malignancy in patients with inflammatory bowel disease. Long-term concomitant use of immunosuppressants with anti-TNF mAbs increases the risk of infectious disease. In the Crohn’s Therapy, Resource, Evaluation, and Assessment Tool (TREAT) Registry, treatment with thiopurines was associated with more frequent serious infections (adjusted odds ratio (OR), 1.23; 95% CI 0.96–1.57) [19, 20]. With regard to lymphoma risk, the Cancer and Increased Risk Associated with Inflammatory Bowel Disease in France (CESAME) study [combination therapy: standardised incidence ratio, 10.2 (95% CI 1.24–36.9); thiopurine monotherapy: 6.86 (3.84–11.31)] and the Kaiser Permanente IBD Registry [combination therapy: 6.6 (4.4–8.8); thiopurine monotherapy: 1.4 (1.2–1.7)] showed a higher risk of lymphoma on combination therapy than for thiopurine monotherapy [19, 21, 22].
In analyses of 1594 patients with CD who participated in clinical trials using ADA, ADA monotherapy did not show a significant increase in the risk of non-melanoma skin cancer and other cancers, whereas concomitant use of thiopurines with ADA showed a significant increase in the risk of non-melanoma skin cancer and other cancers [5]. In this regard, Van Assche et al. suggested withdrawal of thiopurines in patients with CD in CFCR for ≥ 6 months with scheduled maintenance using IFX combined with thiopurines. They found that the clinical course (a change in IFX dosing, treatment interval, or cessation of IFX therapy) and endoscopic findings were not significantly different between the thiopurines continue and the discontinue groups, but the CRP level was significantly higher and the trough level of IFX in serum was lower in the discontinue group [4].
In the DIAMOND2, the proportion of AAA-positive patients at week 52 tended to be higher in the Dis group, but not significantly so. In fact, AAA negativity changed to AAA positivity during the observation period in only three patients. Conversely, the trough concentration of ADA in serum of AAA-negative patients was significantly higher than that in AAA-positive patients. In patients with a high titre of AAAs, the trough concentration of ADA in serum was extremely low. This observation may suggest that, with regard to the trough concentration of ADA in serum, the AAA titre is more important rather AAA positivity. Although the impact of the titre of anti-drug antibodies upon treatment efficacy is controversial, high levels of AAA were associated with increase in disease activity and decreased ADA trough concentration in previous reports [9, 23, 24].
Taken together, we believe that all patients who are in clinical remission do not necessarily need long-term use of thiopurines with ADA maintenance. The risk of induction of anti-drug antibodies is relatively higher in patients with active disease, so it may be reasonable for concomitant use of thiopurines with anti-TNF mAbs as induction therapy especially in complicated patients with severe disease who have the wild type of NUDT15 genotype (codon 139, Arg/Arg) [25, 26], whereas in patients who can maintain remission for > 6 months, thiopurines could be stopped to reduce the risk of infection and malignancy.
Our study had three main limitations. First, the actual number of registered cases in the DIAMOND2 was lower than that in the schedule, so our study was under-powered statistically. Enrolment of participants required more time than anticipated. Therefore, the initial enrolment period fixed to 12 months was twice extended to ultimately 30 months in an effort to include the required sample size. Further prolongation of inclusion period was financially not feasible especially due to the costs of the study, necessitating closure of the study before reaching the calculated number of patients. In addition, not all the patients who enrolled this study came from DIAMOND1 study. Therefore, there could be selection bias for enrolment. Second, we assumed the superiority of continuation of thiopurines. The DIAMOND2 was not powered to demonstrate subtle differences in clinical benefit between the two groups. However, the lower limit of the CI for CFCR of both groups was ~ 75%, and the CIs of the risk difference and risk ratio were within a narrow range. Therefore, the DIAMOND2 suggested that CFCR prevalence was sufficiently high and not significantly different in both groups (of course, it is not confirmatory). However, we believe that the clinical importance of the DIAMOND2 should be taken into consideration fully even though the response and number of enrolled cases in both groups were unexpected. The CFCR prevalence of both groups in the DIAMOND2 was consistent with that of the long-term efficacy and safety of adalimumab maintenance therapy in Crohn’s disease in a follow-on randomised controlled trial (CLASSIC II) undertaken to evaluate long-term efficacy and safety of ADA maintenance therapy in CD. In the CLASSIC II, patients who were in clinical remission at week 4 were followed up until week 56. At week 56, 79% of patients who were maintained with ADA (40 mg, e.o.w.) and 83% of patients who were maintained with ADA (40 mg) weekly were in clinical remission, in contrast to 44% of the placebo group. Concomitant use of thiopurines was 21% in the ADA (40 mg, e.o.w.) group [27]. In the DIAMOND2, the statistical power was ~ 75% even if the CFCR of 95% in each group and non-inferior margin of 12.5% were assumed (alpha = 10% one-sided). Third, the observation period of the DIAMOND2 was 52 weeks. We may have missed the disadvantage of withdrawal of thiopurines in this observation period if it had a gradual influence. Long-term, extensive observation of patients enrolled in the DIAMOND2 should provide the risk of withdrawal of thiopurines in ADA maintenance in CD.
Conclusions
In this prospective, controlled study, continuation of combination of ADA with thiopurines > 6 months was not superior to withdrawal of thiopurines. This observation suggests that further consideration of the thiopurine combination in ADA maintenance therapy for CD is necessary from the viewpoints of benefit and risk.
References
Shi HY, Ng SC. The state of the art on treatment of Crohn’s disease. J Gastroenterol. 2018;53:989–98.
Matsuoka K, Kobayashi T, Ueno F, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol. 2018;53:305–53.
Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–95.
Van Assche G, Magdelaine-Beuzelin C, D’Haens G, et al. Withdrawal of immunosuppression in Crohn’s disease treated with scheduled infliximab maintenance: a randomized trial. Gastroenterology. 2008;134:1861–8.
Osterman MT, Sandborn WJ, Colombel JF, et al. Increased risk of malignancy with adalimumab combination therapy, compared with monotherapy, for Crohn’s disease. Gastroenterology. 2014;146:941–9.
Reenaers C, Louis E, Belaiche J, et al. Does co-treatment with immunosuppressors improve outcome in patients with Crohn’s disease treated with adalimumab? Aliment Pharmacol Ther. 2012;36:1040–8.
Kopylov U, Al-Taweel T, Yaghoobi M, et al. Adalimumab monotherapy versus combination therapy with immunomodulators in patients with Crohn’s disease: a systematic review and meta-analysis. J Crohns Colitis. 2014;8:1632–41.
Matsumoto T, Motoya S, Watanabe K, et al. Adalimumab monotherapy and a combination with azathioprine for Crohn’s disease: a prospective, randomized trial. J Crohns Colitis. 2016;10:1259–66.
Nakase H, Motoya S, Matsumoto T, et al. Significance of measurement of serum trough level and anti-drug antibody of adalimumab as personalised pharmacokinetics in patients with Crohn’s disease: a subanalysis of the DIAMOND trial. Aliment Pharmacol Ther. 2017;46:873–82.
Watanabe K, Matsumoto T, Hisamatsu T, et al. Clinical and pharmacokinetic factors associated with mucosal healing induced by adalimumab in patients with Crohn’s disease: a sub-analysis of a prospective randomized clinical trial (DIAMOND study). Clin Gastroenterol Hepatol. 2018;16:542–9.
Best WR, Beckrel JM, Singleton JW, et al. Development of a Crohn’s disease activity index. Gastroenterology. 1976;70:439–44.
Kochi S, Matsumoto T, Esaki M, et al. Prediction of 6-thioguanine nucleotides levels in Japanese patients with inflammatory bowel disease during long-term thiopurine administration. Scand J Gastroenterol. 2010;45:608–14.
Daperno M, D’Heans G, van Asshche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease. The SES-CD. Gastrointest Endosc. 2004;60:505–12.
Ferrante M, Noman M, Vermeire S. Evolution of endoscopic activity scores under placebo therapy in Crohn’s disease. Gastroenterology. 2010;138:s358.
Lennard L, Singleton HJ. High-performance liquid chromatographic assay of the methyl and nucleotide metabolites of 6-mercaptopurine. Quantification of red blood cell 6-thioguanine nucleotide, 6-thionosinic acid and 6-methylmercaptopurine metabolites in a single sample. J Chromatogr. 1992;583:83–90.
Bartelds GM, Krieckaert CL, Nurmohamed MT, et al. Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA. 2011;305:1460–8.
Bartends GM, Wijbrandts CA, Nurmohamed MT, et al. Clinical response to adalimumab. Relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis. 2007;66:921–6.
Boyapati RK, Torres J, Palmela C, et al. Withdrawal of immunosuppressant or biologic therapy for patients with quiescent Crohn’s disease. Cochrane Database Syst Rev. 2018;5:CD012540.
Terdiman JP, Gruss C, Heidelbaugh JJ, et al. American Gastroenterological Association institute guideline on the use of thiopurines, methotrexate, and anti-TNF-a biologic drugs for the induction and maintenance of remission in inflammatory Crohn’s disease. Gastroenterology. 2013;145:1459–63.
Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow-up in the TREAT registry. Am J Gastroenterol. 2012;107:1409–22.
Beaugerie L, Brousse N, Bouvier AM, et al. Lymphoproliferative disorders in patients receiving thiopurines for inflammatory bowel disease: a prospective observational cohort study. Lancet. 2009;374:1617–25.
Herrinton LJ, Liu L, Weng X, et al. Role of thiopurine and anti-TNF therapy in lymphoma in inflammatory bowel disease. Am J Gastroenterol. 2011;106:2146–53.
Imaeda H, Takahashi K, Fujimoto T, et al. Clinical utility of newly developed immunoassays for serum concentrations of adalimumab and anti-adalimumab antibodies in patients with Crohn’s disease. J Gastroenterol. 2014;49(1):100–9.
Mazor Y, Almog R, Kopylov U, et al. Adalimumab drug and antibody levels as predictors of clinical and laboratory response in patients with Crohn’s disease. Aliment Pharmacol Ther. 2014;40(6):620–8.
Kakuta Y, Kinouchi Y, Shimosegawa T. Pharmacogenetics of thiopurines for inflammatory bowel disease in East Asia: prospects for clinical application of NUDT15 genotyping. J Gastroenterol. 2018;53:172–80.
Kakuta Y, Kawai Y, Okamoto D, et al. NUDT15 codon 139 is the best pharmacogenetic marker for predicting thiopurine-induced severe adverse events in Japanese patients with inflammatory bowel disease: a multicenter study. J Gastroenterol. 2018;53(9):1065–78.
Sandborn WJ, Hanauer SB, Rutgeerts P, et al. Adalimumab for maintenance treatment of Crohn’s disease: results of the CLASSIC II trial. Gut. 2007;56:1232–9.
Acknowledgements
We thank Arshad Makhdum, PhD, from Edanz Group (https://www.edanzediting.com/ac) for editing a draft of this manuscript. Members of the DIAMOND2 Study Group are: Katsuya Endo (Tohoku University), Motohiro Esaki (Kyushu University), Hiroyuki Hanai (Hamamatsu South Hospital), Taku Kobayashi and Toshifumi Hibi (Kitasato University Kitasato Institute Hospital), Sakiko Hiraoka (Okayama University), Tadakazu Hisamatsu (Kyorin University), Yutaka Honda (Niigata University), Satoko Inoue (Kobe City Medical Center General Hospital), Takuya Inoue (Osaka Medical College), Shuji Inoue (Kochi National Hospital), Tetsuya Ishida (Ishida Clinic of IBD and Gastroenterology), Hiroaki Ito (Kinshukai Infusion Clinic), Ryuichi Iwakiri (Saga University), Motoyoshi Izumi (Machida Municipal Hospital), Takashi Kagaya (Kanazawa University), Noriko Kamata (Osaka City University), Makoto Naganuma and Takanori Kanai (Keio University), Yumiko Naganawa, Hiroyuki Kaneto (Muroran City General Hospital), Kazuhito Kani and Shingo Kato (Saitama Medical University), Fukunori Kinjyo (Ryukyu University), Reiko Kunisaki (Yokohama City University Medical Center), Hiroki Yasaka and Koichi Kurahara (Matsuyama Red Cross Hospital), Lee Kyouwon (Moriguchikeijinkai Hospital), Yutaka Yano, Fumihito Hirai and Toshiyuki Matsui (Fukuoka University Chikushi Hospital), Takayuki Matsumoto (Iwate Medical University), Hiroki Tanaka and Satoshi Motoya (Sapporo Kosei General Hospital), Yoshinori Munemoto (Fukui-ken Saiseikai Hospital), Yuji Naito (Kyoto Prefectural University of Medicine), Tomoo Nakagawa (Chiba University), Yoko Yokoyama, Kenji Watanabe and Shiro Nakamura (Hyogo College of Medicine), Hiroshi Nakase (Sapporo Medical University, School of Medicine), Masanori Nojima (The University of Tokyo), Norimasa Fukata and Kazuichi Okazaki (Kansai Medical University), Sachiko Ouchi (Steel Memorial Hirohata Hospital), Hirotake Sakuraba (Hirosaki University), Masayuki Saruta (The Jikei University School of Medicine), Makoto Sasaki (Aichi Medical University), Takeshi Sugaya (Japan Red Cross Ashikaga Hospital), Yasuo Suzuki (Toho University Sakura Medical Center), Fuminao Takeshima (Nagasaki University), Hiroyuki Tamaki (Takamatsu Red Cross Hospital), Shinji Tanaka (Hiroshima University), Satoshi Tanida and Tsutomu Mizoshita (Nagoya City University), Keiichi Tominaga (Dokkyo Medical University), Masakazu Nagahori and Mamoru Watanabe (Tokyo Medical and Dental University), Masaki Yamashita (St. Marianna University School of Medicine), Atsushi Yoshida (Ofuna Central Hospital), and Naoki Yoshimura (Tokyo Yamate Medical Center).
Funding
Grant from the Ministry of Health, Labour and Welfare of Japan (“Investigation and research for intractable inflammatory bowel disease”).
Author information
Authors and Affiliations
Consortia
Contributions
Concept and design of the study (TH, HN, KW, TM, YS, MW, TH), acquisition of data (SK, RK, MM, MN, SM, ME, NF, SI, TS, HS, FH, MN, TK), analyses and interpretation of data (TH, HN, KW, TM, MN), drafting of the manuscript (TH, HN, KW, TM, MN), critical revision of the manuscript for important intellectual content (YS, MW, TH), statistical analyses (MN) and study supervision (YS, MW, TH).
Corresponding author
Ethics declarations
Conflict of interest
T Hisamatsu: Honoraria: EA pharma Co. Ltd., AbbVie GK, Celgene K.K., Janssen Pharmaceutical K.K., Pfizer Inc., Takeda Pharmaceutical Co. Ltd., Mitsubishi Tanabe Pharma Corporation, Kyorin Pharmaceutical Co. Ltd., JIMRO Co. Ltd., Mochida Pharmaceutical Co., Ltd., Nichi-lko Pharmaceutical Co., Ltd. Commercial research funding: EA pharma Co. Ltd., AbbVie GK, Daiichi-Sankyo Co. Ltd., Takeda Pharmaceutical Co. Ltd., Pfizer Inc., Mochida Pharmaceutical Co., Ltd, Nippon Kayaku Co. Ltd., Kyorin Pharmaceutical Co. Ltd., JIMRO Co. Mochida Pharmaceutical Co., Ltd., Astellas Pharma Inc., Asahi Kasei Medical Co., Ltd., ZERIA Pharmaceutical Co. Ltd. S. Kato: Honoraria: Mistubishi Tanabe Pharma Corporation, Janssenn Pharma K,K. R. Kunisaki: Honoraria: AbbVie GK, EA pharma Co. Ltd., Janssen Pharmaceutical K.K., JIMRO Co. Ltd., Kissei Pharmaceutical Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Kyowa Hakko Kirin Co. Ltd., Nioppon Kayaku Co. Ltd., Mitsubishi Tanabe Pharma Corporation, Takeda Pharmaceutical Co. Ltd., ZERIA Pharmaceutical Co. Ltd. Commercial research funding: AbbVie GK, EA pharma Co. Ltd., Janssen Pharmaceutical K.K., JIMRO Co. Ltd., Kissei Pharmaceutical Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Kyowa Hakko Kirin Co. Ltd., Mitsubishi Tanabe Pharma Corporation, RPM Co. Ltd, Takeda Pharmaceutical Co. Ltd. M. Matsuura: Honoraria: AbbVie GK, Mitsubishi Tanabe Pharma Corporation, EA pharma Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Mochida Pharmaceutical Co., Ltd., Janssen Pharmaceutical K.K., Nioppon Kayaku Co. Ltd., Kissei Pharmaceutical Co. Ltd. Commercial research funding: AbbVie GK, Mitsubishi Tanabe Pharma Corporation, EA pharma Co. Ltd., Mochida Pharmaceutical Co., Ltd., Nioppon Kayaku Co. Ltd., JIMRO Co. M. Nagahori: Honoraria: Kissei Pharmaceutical Co. Ltd., Takeda Pharmaceutical Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Mochida Pharmaceutical Co., Ltd., AbbVie GK, Mitsubishi Tanabe Pharma Corporation, Nioppon Kayaku Co. Ltd., Asahi Kasei Medical Co., Ltd., ZERIA Pharmaceutical Co. Ltd., Astellas Pharma Inc., Nichi-lko Pharmaceutical Co., Ltd., Janssen Pharmaceutical K.K. S. Motoya: Honoraria: Eisai Corporation, AbbVie GK, Mitsubishi Tanabe Pharma Corporation, Takeda Pharma Corporation, Mochida Pharma Corporation, Janssen Pharmaceutical K.K. M. Esaki: Honoraria: AbbVie, Mitsubishi Tanabe Pharma Corporation. Commercial research funding: EA pharma Co. Ltd., AbbVie GK, Mitsubishi Tanabe Pharma Corporation. N. Fukata: no conflict of interest. S. Inoue: no conflict of interest. T. Sugaya: no conflict of interest. H. SAKURABA: Commercial research funding: Bristol-Myers Squibb, AbbVie GK, MSD Inc., Daiichi-Sankyo Co. Ltd., ZERIA Pharmaceutical Co. Ltd. F. Hirai: Honoraria: EA Pharma CO. Ltd, AbbVie GK, Mitsugishi Tanabe Pharma, Eisai CO.,Ltd. K. Watanabe: Honoraria: EA Pharma Co. Ltd., AbbVie, Mitsubishi Tanabe Pharma Corporation, Kyorin Pharmaceutical Co. Ltd., JIMRO Co. Ltd., Mochida Pharmaceutical Co. Ltd., Janssen Pharmaceutical K.K, Takeda Pharmaceutical Co. Ltd. Commercial research funding: EA Pharma Co. Ltd., AbbVie, Mitsubishi Tanabe Pharma Corporation, Kyorin Pharmaceutical Co. Ltd., JIMRO Co. Ltd., Astellas Pharma Inc. T. Kanai: Honoraria: EA pharma Co. Ltd., AbbVie GK, Janssen Pharmaceutical K.K., Pfizer Inc., Mitsubishi Tanabe Pharma Corporation, Kyorin Pharmaceutical Co. Ltd., Yakult Honsha Co., Ltd., ZERIA Pharmaceutical Co. Ltd., Miyarisan Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Astellas Pharma Inc., Sumitomo Dainippon Pharma Co. Ltd. Commercial research funding: Eisai Corporation, JIMRO Co. Ltd., Nippon Kayaku Co. Ltd., Daiichi-Sankyo Co. Ltd., Tsumura & Co., Taiho Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., EN Otsuka Pharmaceutical Co. Ltd., Ezaki Glico Co. Ltd., RPM Co. Ltd., Yakult Bio-Science Foundation.M. Naganuma: Honoraria: EA Pharma Co. Ltd. Commercial research funding: EA Pharma Co. Ltd., ZERIA, Mochida Pharmaceutical CO. Ltd. H. Nakase: Honoraria: Mitsubishi Tanabe Pharma Corporation, Mochida Pharmaceutical CO. Ltd., Janssen Pharmaceutical K.K, AbbVie GK. Commercial research funding: Hoya group Pentax Medical. Boehringer Ingelheim GmbH, Daticho-Sankyo Co. Ltd. Y. Suzuki: Honoraria: AbbVie GK, Mitsubishi Tanabe Pharma Corporation, ZERIA Pharmaceutical Co. Ltd., Mochida Pharmaceutical Co. Ltd., Kyorin Pharmaceutical Co. Ltd., EA pharma Co. Ltd., Janssen Pharmaceutical K.K. Commercial research funding: AbbVie GK, Mitsubishi Tanabe Pharma Corporation, EA pharma Co. Ltd., JIMRO Co. Ltd., Mochida Pharmaceutical Co. Ltd., Nippon Kayaku Co. Ltd., KISSEI. M. Watanabe: Honoraria: Mitsubishi Tanabe Pharma Corp., Eisai Co. Ltd., Kyorin Pharmaceutical Co. Ltd., JIMRO Co. Ltd., AbbVie GK, Takeda Pharmaceutical Co. Ltd., Kyowa Hakko Kirin Co. Ltd., ZERIA Pharmaceutical Co. Ltd., Asahi Kasei Medical Co. Ltd., EA Pharma Co. Ltd., Astellas Pharma Inc., Mochida Pharmaceutical Co. Ltd., Janssen Pharmaceutical Co. Ltd., Gilead Sciences, Inc., Celgene Corp., Kissei Pharmaceutical Co. Ltd. Commercial research funding: Asahi Kasei Medical Co. Ltd., AbbVie GK, EA Pharma Co. Ltd., Eisai Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Mitsubishi Tanabe Pharma Corp., Otsuka Pharmaceutical Co. Ltd., Kyowa Hakko Kirin Co. Ltd., ZERIA Pharmaceutical Co. Ltd., JIMRO Co. Ltd., Takeda Pharmaceutical Co. Ltd., Nippon Kayaku Co. Ltd., Mochida Pharmaceutical Co. Ltd., Daiichi-Sankyo Co. Ltd., Astellas Pharma Inc., MSD K.K., Dainippon Sumitomo Dainippon Pharma Co. Ltd., Bristol-Myers, K.K, Chugai Pharmaceutical Co. Ltd., Gilead Sciences Inc., Pfizer Inc., Miyarisan Pharmaceutical Co. Ltd., Kissei Pharmaceutical Co. Ltd., Taiho Pharmaceutical Co. Ltd. T. HIBI: Honoraria: Mitsubishi Tanabe Pharma CO., AbbVie GK, EA Pharma Co., Ltd. M. Nojima: no conflict of interest. T. Matsumoto: Honoraria: Mitsubishi Tanabe Pharma Corporation, AbbVie GK, EA pharma Co. Ltd., Janssen Pharmaceutical K.K. Commercial research funding: Mitsubishi Tanabe Pharma Corporation, EA pharma Co. Ltd., Nippon Kayaku Co. Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the group are listed in Acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2019_1582_MOESM4_ESM.tif
Supplemental Figure 3. Proportion of patients with triple remission at week 52. Triple remission was defined as CFCR, endoscopic remission (SES-CD ≤2), and serological remission (CRP ≤0.10 mg/dl). Statistical analyses were by Welch’s t-test. Con: continue group; D: discontinue group. (TIFF 48 kb)
Rights and permissions
About this article
Cite this article
Hisamatsu, T., Kato, S., Kunisaki, R. et al. Withdrawal of thiopurines in Crohn’s disease treated with scheduled adalimumab maintenance: a prospective randomised clinical trial (DIAMOND2). J Gastroenterol 54, 860–870 (2019). https://doi.org/10.1007/s00535-019-01582-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-019-01582-w