Abstract
Background
Methotrexate (MTX) combination therapy with biological agents has gained increasing interest. Here, we assessed the efficacy and tolerability of the MTX combination therapy in patients with Crohn’s disease (CD).
Methods
We performed a multicenter observational study with 185 patients with CD with MTX and biologics combination therapy; the patients were recruited from three IBD Clinics in Korea. We evaluated the outcomes of the MTX combination therapy and examined the predictive factors of clinical and endoscopic remission.
Results
MTX was administered orally to 62.7% of patients; the mean dose was 15.5 mg per week, and the mean treatment duration was 36 months. Of the 169 patients treated with MTX combination therapy for over 6 months, the steroid-free clinical remission rates were 34.3%, 26.0%, 29.8%, and 32.7% at 4, 12, 18, and 24 months, respectively. Previous thiopurine use was a significant negatively associated independent factor (p < 0.001), and a higher dose of MTX (≥ 15 mg/week) was a positively associated independent factor of steroid-free clinical remission (p = 0.035). Ninety-six patients underwent follow-up endoscopy after 28 months, and 36 (37.5%) achieved endoscopic remission. Longer disease duration (p = 0.006), ileocolonic type of Montreal location (p = 0.036), and baseline C-reactive protein (CRP) level of more than 5 mg/L (p = 0.035) were significant negatively associated independent factors and a higher dose of MTX (≥ 15 mg/week) was a positively associated independent factor of endoscopic remission (p = 0.037).
Conclusions
MTX combination therapy with biologics was effective and tolerable in patients with CD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, biological therapies are the mainstay of induction and maintenance treatments for moderate to severe Crohn’s disease (CD) [1]. Studies have suggested that combination therapy with biological agents and immunomodulators decreases anti-drug antibody formation and minimizes the immunogenicity of the biological agents [2]. The comparative efficacy of a combination of infliximab and azathioprine was superior to that of infliximab monotherapy in inducing clinical remission in the “Study of Biologic and Immunomodulators Naïve Patients in Crohn’s Disease (SONIC)” trial for CD and “Comparison of the Efficacy and Safety of Infliximab, as Monotherapy or in Combination With Azathioprine, Versus Azathioprine Monotherapy (SUCCESS)” trial for ulcerative colitis (UC) [1, 3]. A recent prospective observational personalized antitumor necrosis factor (TNF) therapy in a CD study (PANTS) showed that infliximab combination therapy contributed to both clinical remission induction and immunogenicity reduction, whereas adalimumab combination therapy failed to facilitate clinical remission but contributed to immunogenicity reduction [4].
Methotrexate (MTX) is mostly used as an alternative drug in cases of intolerance to or occurrence of side effects after thiopurine therapies, such as azathioprine and 6-mercaptopurine (6-MP). However, the Adverse Event Reporting System of the Food and Drug Administration (FDA) reported that concomitant infliximab and thiopurine therapy for young male patients with CD was significantly associated with a risk of developing hepatosplenic T-cell lymphoma [5, 6]. Cytopenia was more frequently associated with thiopurines than with MTX. In particular, myelosuppression was reported to occur in 56.4% of Korean patients with IBD after treatment with maximal doses of azathioprine and 6-MP, which is considerably higher than that reported in Western studies [7, 8]. MTX is increasingly used because of its shorter duration of action, lower cost, and lower risk of malignancy than thiopurines [9, 10].
In the “Combination of Maintenance of Methotrexate-Infliximab Trial (COMMIT),” patients with CD who received MTX concomitantly were less likely to develop antibody formation to infliximab (ATI) than those who received infliximab alone (4% vs. 20%, p = 0.01) [11]. Vermeire et al. found that the incidence of ATI did not differ between the MTX and azathioprine groups (44% vs. 48%) [12]. Kennedy et al. also suggested that concomitant immunomodulator use contributed to reduced immunogenicity of biological agents; however, there was no difference between thiopurines and methotrexate [4]. Combination therapies have shown potential pharmacokinetic and immunogenic benefits. Although the utility of the combination of MTX with biological agents has been gaining increasing interest, few studies have evaluated the clinical outcomes of MTX-biologics combination therapy in real-world IBD practice. We aimed to investigate the effectiveness and safety of MTX combination therapy with biologics and analyze the prognostic factors associated with clinical and endoscopic remission in patients with CD.
Materials and Methods
Study Population
From June 2007 to December 2022, all consecutive patients administered MTX for CD treatment were enrolled in this multicenter, retrospective cohort study. A total of 311 patients were administered MTX for the treatment of CD at three tertiary referral hospitals: the IBD Clinic of Severance Hospital, Yonsei University College of Medicine (Seoul, Korea); Gangnam Severance Hospital (Seoul, Korea); and Seoul National University Bundang Hospital (Seongnam, Korea). The inclusion criteria were as follows: (i) age 18 years or older, (ii) a definite diagnosis of CD according to endoscopic, histological, or radiological criteria, and (iii) administration of MTX with a biologic agent as combination therapy (concomitant use of 5-aminosalicylates or corticosteroids was allowed). Not only patients who started biologics and MTX at the same time but also cases where MTX was added while using biologics were included. The exclusion criteria were as follows: (i) those treated with MTX monotherapy (n = 94), (ii) those treated less than 4 months (n = 22), (iii) those treated to control joint pain (n = 3), and (iv) those finally diagnosed with intestinal Behçet’s disease (n = 7) (Fig. 1). The patients were identified using the electronic medical record system for all patients with IBD at each institution.
A total of 185 patients with CD were treated with MTX and other biological agents. This study was approved by the Institutional Review Boards of Severance Hospital, Yonsei University, and Seoul National University Bundang Hospital (IRB No: 4-2022-0386, B-2206-764-103).
Treatment Protocol and Outcome Measures
The patients received various doses of MTX, which were administered either subcutaneously or orally on a weekly basis at the discretion of the physicians. Infliximab was administered at 5 mg/kg intravenously at weeks 0, 2, and 6 and then every 8 weeks. Adalimumab was administered subcutaneously at a dose of 160 mg at week 0, 80 mg at week 2, and 40 mg every other week. The complete blood count (CBC) and serum aminotransferase levels were monitored. Vedolizumab was administered intravenously at a dose of 300 mg at weeks 0, 2, and 6 and then every 8 weeks. Ustekinumab was administered intravenously in weight-based dosage regimens of 260 mg (less than 55 kg), 390 mg (> 55 kg, less than 85 kg), and 520 mg (> 85 kg). After the loading dose, ustekinumab was administered subcutaneously at a dose of 90 mg at week 8 and then every 8 or 12 weeks. Dose escalation of the biological agents was allowed in this study.
The primary outcome of interest was corticosteroid-free clinical remission at 4 months, defined as clinical remission with a Crohn’s Disease Activity Index (CDAI) score ≤ 150 and complete withdrawal of corticosteroids [11, 13]. Secondary end points were corticosteroid-free clinical remission at 12, 18, and 24 months, the mean change in serum C-reactive protein (CRP) levels, adverse events, and endoscopic remission, which was defined as with a Simple Endoscopic Score for Crohn Disease (SES-CD) score ≤ 2 [14].
Data Collection
We retrospectively collected the following data from the electronic medical records of the patients: sex, age, smoking history, weight, body mass index (BMI), disease duration, Montreal classification of location and behavior, presence of perianal lesions, history of bowel surgery, previous medications before enrollment, concomitant medications at enrollment, C-reactive protein (CRP) level, hemoglobin level, albumin level, MTX administration route, MTX dose, indication of MTX, reason of MTX discontinuation, and adverse events of MTX.
Statistical Analysis
Mean and standard deviation or median and range were calculated for all continuous variables, as appropriate. Multivariate logistic regression analyses were performed to identify the independent risk factors for clinical remission after MTX combination therapy at 4 months with adjustment for various confounders, including age, sex, disease duration, smoking history, BMI, disease location and behavior, perianal lesion, history of intestinal resection, previous medications, concomitant medications, CRP level, hemoglobin level, albumin level, MTX administration route, and MTX dose. Cox proportional hazards analyses were performed to reveal the independent risk factors of endoscopic remission after MTX combination therapy. Variables in univariate analysis were entered into multivariate analysis if the p value was < 0.05 (considered statistically significant). All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 23.0; SPSS Inc., Armonk, NY, USA).
Results
Patient Baseline Characteristics
A total of 185 patients with CD who attended the IBD Clinic of Severance Hospital, Yonsei University College of Medicine (Seoul, Korea), Gangnam Severance Hospital (Seoul, Korea), and Seoul National University Bundang Hospital (Seongnam, Korea) were treated with MTX concomitantly with biological agents as part of combination therapy. Mean age at initiation of combination therapy of MTX was 28.5 ± 11.7 years; 128 patients (69.2%) were male, and the mean disease duration was 6.7 ± 6.6 years (Table 1). The main locations of CD were the terminal ileum and colon (130 patients, 70.3%). CD was inflammatory in 85 (45.9%), stricturing in 38 (20.5%), and penetrating in 62 (33.5%) patients. Perianal lesions were present in 113 patients (61.1%) and bowel surgery was previously performed in 61 patients (33.0%). One hundred and twenty-four (67.0%) patients had been treated with thiopurines and 108 (58.4%) had been treated with biologic agents before enrollment.
Characteristics of Patients at the Time of Combination Therapy with MTX
MTX was administered orally (62.7%) or parenterally (37.3%) (Table 1). The mean dose of MTX was 15.5 ± 5.8 mg per week (median, 15.0 mg/week; range, 5.0–25.0 mg/week) during the induction period and 113 patients (61.1%) were treated with high dose MTX (≥ 15 mg/week) (Table 1). Of the 185 patients, 109 (58.9%) received infliximab, 56 (30.3%) received adalimumab, 15 (8.1%) received ustekinumab, and 5 (2.7%) received vedolizumab at the time of initiation of MTX combination therapy. The mean duration of the use of MTX with biological agents was 34.9 months (median, 27.0 months; range 4.0–108.0 months) (Table 1).
The main indication for combination therapy was failure of biological agent monotherapy (n = 71; 38.4%) (Table 2). Other indications included thiopurine intolerance (9.7%), thiopurine ineffectiveness (6.5%), intolerance to a combination of a biological agent and thiopurine (7.0%), ineffectiveness of a combination of a biologic agent and thiopurine (21.1%), and initial use in immunomodulator-naïve patients (17.3%).
Adverse Events During Combination Therapy with MTX
At least one adverse effect was reported in 39 patients (21.1%). Nausea was reported in 14 patients (7.6%); of these, 11 patients required discontinuation of MTX. Liver enzyme abnormalities were reported in 7 patients (3.8%) and of these, 5 patients required discontinuation of MTX. Cytopenia was reported in 4 patients (2.0%); of these, 3 patients required discontinuation of MTX. Other adverse events included intra-abdominal abscesses (n = 6, 3.2%), fatigue (n = 4, 2.2%), rash (n = 2, 1.1%), cystitis (n = 2, 1.1%), herpes zoster (n = 1, 0.5%), and abdominal pain (n = 1, 0.5%) (Table 2).
Clinical Outcomes After Combination Therapy with MTX
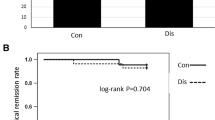
A total of 169 patients who were treated with combination therapy with MTX and followed up for over 6 months were considered eligible for statistical analysis after induction. Steroid-free clinical remission was achieved in 58 of 169 (34.3%) patients at 4 months, 41 of 158 (26.0%) patients at 12 months, 37 of 124 (29.8%) patients at 18 months, and 33 of 101 (32.7%) patients at 24 months (Fig. 2A). Mean CRP levels were 9.9 ± 14.2 mg/L, 6.6 ± 17.8 mg/L, 4.8 ± 11.3 mg/L, and 2.8 ± 6.1 mg/L at 0, 6, 12, and 24 months, respectively (Fig. 2B). There was no statistically significant difference of steroid-free clinical remission rates at 4 months between standard and escalated dose of biologics agents (28.3% vs. 31.2%; p = 0.736).
Logistic regression analysis was used to examine the impact of different variables on the induction of clinical remission at 4 months; previous use of thiopurine was a significant independent factor associated with poor outcomes (odds ratio [OR] 0.202, 95% confidence interval [CI] 0.082–0.494, p < 0.001; Table 3). Also, a higher dose MTX (≥ 15 mg/week) was a significant independent factor associated with corticosteroid-free clinical remission of MTX combination therapy at 4 months (OR 2.687, 95% CI 1.071–6.738, p = 0.035; Table 3). Among the patients on combination therapy with biologics, no statistically significant difference of steroid-free clinical remission rates at 4 months was found according to type of biologics (30.7% [31/101] for infliximab, 21.6% [11/51] for adalimumab, 33.3% [4/12] for ustekinumab, and 25.0% [1/4] for vedolizumab; p = 0.330).
A total of 96 patients underwent endoscopy after 28.0 months (median, 16.1 months; range 6.0–99.0 months). Among them, 36 patients (37.5%) achieved endoscopic remission after MTX combination therapy. Using the Cox proportional hazard analysis, a longer disease duration (hazards ratio [HR] 0.826, 95% CI 0.720–0.948, p = 0.006), ileocolonic type of Montreal location compared to ileal type of Montreal location (HR 0.358, 95% CI 0.158–0.942, p = 0.036), and baseline CRP level more than 5 mg/L (HR 0.396, 95% CI 0.167–0.941, p = 0.036) were significant independent factors negatively associated with endoscopic remission of MTX combination therapy (Table 4). A higher dose MTX (≥ 15 mg/week) was a statistically significant independent factor positively associated with endoscopic remission of MTX combination therapy (HR: 3.180, 95% CI: 1.074–9.411, p = 0.037; Table 4).
Seventy-four patients discontinued MTX combination therapy, and the main reason for discontinuation of combination therapy was intolerance (44.6%). Other reasons for discontinuation of combination therapy were de-escalation (28.4%), clinical ineffectiveness (12.2%), pregnancy plans (4.1%), and self-discontinuation (10.8%) (Table 2).
Discussion
MTX was first used in patients with IBD in 1987, and it had a significant beneficial effect on induction and maintenance in patients with IBD as per a recent Cochrane review [11, 15, 16]. Nevertheless, azathioprine is preferentially used over MTX as the mainstream treatment for IBD [17]. The reasons might be the lack of studies on MTX, its non-oral administration route, and the considerable side effects of high-dose MTX in patients with cancer [18]. The COMMIT trial appeared disappointing in terms of the clinical benefits of MTX combination therapy [11]. Moreover, MTX was not effective in treating UC [19]. MTX in combination with infliximab did not show any clinical benefit compared with infliximab alone (30.6% vs. 29.8%, p = 0.63) in a randomized trial, despite the favorable effects of MTX on ATI (20.0% vs. 4.0%, p = 0.01) [11]. We hypothesized that the corticosteroids administered to every patient in the COMMIT trial for active symptoms might have obscured the benefits of MTX. It is still possible that the significant reduction in the development of ATI by MTX may translate into long-term benefits of combination therapy with MTX, which was not explored in COMMIT [20]. Therefore, we investigated the effectiveness and safety of the combination of MTX and a biological agent for the induction and maintenance of steroid-free clinical remission in CD. To our knowledge, this is the first real-life clinical outcome study using a combination of MTX and a biological agent for patients with CD, particularly in East Asia.
Two retrospective studies aimed to optimize the dose of MTX combination therapy in patients with IBD, with conflicting results. Colman et al. conducted a single-center retrospective study to investigate the maintenance of clinical remission with MTX combination therapy in 73 patients with IBD (54 patients with CD) [21]. Of them, 22 patients (29%) were prescribed a higher dose MTX (≥ 15 mg/week) with combination therapy and 55 patients (75%) were administered MTX orally [21]. A higher dose MTX (≥ 15 mg/week) combination therapy was better for the maintenance of clinical remission compared to low dose MTX in this study, but they did not confirm the effectiveness of MTX dose combination therapy in terms of endoscopic outcome. Borren et al. conducted a single-center retrospective study to investigate the maintenance of clinical remission with MTX combination therapy in 222 patients with IBD (163 patients with CD). Of these, 159 patients (72%) were prescribed high-dose MTX (≥ 15 mg/week) and 123 patients (55%) were administered MTX orally [22]. There was no difference in the clinical effectiveness of MTX combination therapy according to the MTX dose in this study. We conducted a multicenter, retrospective study of only patients with CD, 61% of whom were prescribed a higher dose MTX (≥ 15 mg/week) combination therapy, and 63% were administered orally. We found that a higher dose MTX (≥ 15 mg/week) combination therapy was positively associated with induction of steroid-free clinical remission, and by extension, endoscopic remission, compared to a lower dose MTX in patients with CD. The initial administration route (parenteral vs. oral) or type of concomitant biological agent (anti-TNFs vs. other biological agents) was not associated with the clinical outcomes of MTX combination therapy in patients with CD. Also, among a total of 169 patients who were treated with combination therapy with MTX and followed up for over 6 months, 105 patients (62.1%) were treated with higher dose of MTX (> 15 mg/week) and the other 64 patients (37.9%) treated with lower dose of MTX (< 15 mg/week), and the adverse event proportion was not different between the high-dose (13/105 patients, 12.4%) and low-dose groups (14/64 patients, 21.9%) (p = 0.130). The effectiveness of a higher dose of MTX was evident in our study, in addition to the modulation of immunogenicity. Further follow-up studies with prospectively adjusted doses and controlled variables are necessary.
Our study included patients who did not respond to thiopurines and/or biological agents, whereas most previous studies enrolled biological agent-naïve patients. Using multivariate Cox regression analysis, we found that previous thiopurine use was negatively associated with steroid-free clinical remission after MTX combination therapy in patients with CD. This result suggests that the mechanism of action of MTX combination therapy on CD involves not only the reduction in the immunogenicity of biologic agents but also a synergistic effect with the immunosuppressive properties of MTX itself. Moreover, since the mean disease duration of our study was 6.7 ± 6.6 years, which is quite long, there is a limitation in not knowing the results of MTX combination therapy in patients with early CD. Nevertheless, in our study, a short disease duration was positively associated with endoscopic remission, suggesting that the effect of MTX combination therapy could be further improved in patients with early CD. Taken together, thiopurine-naïve patients with early CD are expected to show good responsiveness to MTX combination therapy.
An elevated baseline CRP level of more than 5 mg/L was negatively associated with endoscopic remission in our study, which is consistent with the results of previous studies. CRP is a useful serum biomarker for predicting severe clinical outcomes in CD [23]. Ileocolonic type of Montreal location compared to ileal type of Montreal location was negatively associated with endoscopic remission in our study. Compared to isolated colonic involvement, isolated ileal involvement and ileocolonic involvement were associated with higher risk for change in disease behavior, developing intestinal complications, but they were significantly less likely to achieve a response or remission. However, there are few studies comparing the clinical outcomes of ileocolonic CD and ileal CD. Also, in our study, ileocolonic CD was negatively associated with endoscopic remission compared to ileal CD.
One of the biggest concerns of combination therapy is the potential for increased adverse events, such as severe infections and malignancies. Of a total of 185 patients who were treated with MTX combination therapy, 33 patients (17.8%) discontinued MTX due to intolerance, and this result was comparable to the results of previous studies that evaluated azathioprine. Colombel et al. reported that 20.7% of patients who received infliximab and azathioprine combination therapy had to stop treatment due to adverse side effects or non-response [24]. Alessandro et al. reported that 27 of 126 patients (21.4%) experienced adverse events during follow-up, but only 11.1% of them (14 of 126) discontinued treatment due to adverse events [25]. Of the 185 patients treated with MTX combination therapy, 7.6% complained of nausea, 3.8% had increased liver enzyme levels, and 2.0% complained of cytopenia. MTX could be a safer drug than thiopurines for treating nausea and cytopenia, which is consistent with the results of previous studies [8, 10, 26]. In particular, MTX should be used as first-line treatment in patients with NUDT15 mutations [27]. Nausea, which occurred in about 2.0–19.0% of patients in previous studies, can be reduced by the use of folic acid [28, 29]. Liver toxicity, which was reported in 14.3–25.0% of patients in previous studies, appears to occur less frequently in IBD than in other inflammatory disorders such as psoriasis [30, 31]. MTX, an analog of folic acid and aminopterin, can also cause myelosuppression, but significant cytopenia occurs uncommonly; it was 0–4.5% in previous Western studies [31,32,33]. However, given the possible side effects, regular treatment monitoring is recommended in these guidelines [34,35,36].
This study had several limitations. First, it was a retrospective, cross-sectional study based on a review of medical records. The dose and route of MTX administration were not consistent among the institutions in the study. Nevertheless, we were able to identify the predictive factors related to the clinical outcomes of MTX combination therapy by analyzing a large number of well-organized databases containing laboratory data. Second, the endoscopic response was evaluated only in some patients at inconsistent time points. Third, we were not able to measure anti-drug antibody (ADA) and drug levels in this study. The reasons why ADA and drug levels could not be collected every time at a clinical site were: first, because this study was a retrospective study; and second, due to Korea’s insurance conditions, the measurements were covered by the National Insurance System only when biological agents were ineffective.
Our study showed that MTX combination therapy can be used in adult patients with IBD with an acceptable effectiveness and tolerability profile. Also, we found that a higher dose MTX (≥ 15 mg/week) combination therapy is superior in terms of clinical and endoscopic remission compared with MTX at lower doses.
Summary
Methotrexate (MTX) combination therapy with biological agents was effective and tolerable in patients with Crohn’s disease. Previous thiopurine use, MTX dose, disease duration, Montreal location, baseline C-reactive protein level were independent factors associated with clinical and endoscopic remission.
Abbreviations
- CD:
-
Crohn’s disease
- TNF:
-
Tumor necrosis factor
- MTX:
-
Methotrexate
- 6-MP:
-
6-Mercaptopurine
- FDA:
-
Food and Drug Administration
- ATI:
-
Antibodies to infliximab
- CBC:
-
Complete blood count
- CDAI:
-
Crohn’s Disease Activity Index
- CRP:
-
C-reactive protein
- SES-CD:
-
Simple Endoscopic Score for Crohn’s Disease
- BMI:
-
Body mass index
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
References
Torres J, Bonovas S, Doherty G et al. ECCO guidelines on therapeutics in Crohn’s disease: medical treatment. J Crohns Colitis. 2020;14:4–22.
Otake H, Matsumoto S, Mashima H. Long-term clinical and real-world experience with Crohn’s disease treated with anti-tumor necrosis factor-alpha antibodies. Intest Res. 2022;20:464–474.
Maser EA, Villela R, Silverberg MS, Greenberg GR. Association of trough serum infliximab to clinical outcome after scheduled maintenance treatment for Crohn’s disease. Clin Gastroenterol Hepatol. 2006;4:1248–1254.
Kennedy NA, Heap GA, Green HD et al. Predictors of anti-TNF treatment failure in anti-TNF-naive patients with active luminal Crohn’s disease: a prospective, multicentre, cohort study. Lancet Gastroenterol Hepatol. 2019;4:341–353.
Rosh JR, Gross T, Mamula P, Griffiths A, Hyams J. Hepatosplenic T-cell lymphoma in adolescents and young adults with Crohn’s disease: a cautionary tale? Inflamm Bowel Dis. 2007;13:1024–1030.
Mackey AC, Green L, Leptak C, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease: update. J Pediatr Gastroenterol Nutr. 2009;48:386–388.
Ansari A, Arenas M, Greenfield SM et al. Prospective evaluation of the pharmacogenetics of azathioprine in the treatment of inflammatory bowel disease. Aliment Pharmacol Ther. 2008;28:973–983.
Kim JH, Cheon JH, Kim WH. The frequency and the course of the adverse effects of azathioprine/6-mercaptopurine treatment in patients with inflammatory bowel disease. Korean J Gastroenterol. 2008;51:291–297.
Herfarth HH, Kappelman MD, Long MD, Isaacs KL. Use of methotrexate in the treatment of inflammatory bowel diseases. Inflamm Bowel Dis. 2016;22:224–233.
Gabbani T, Deiana S, Lunardi S, Manetti N, Annese V. Safety profile of methotrexate in inflammatory bowel disease. Expert Opin Drug Saf. 2016;15:1427–1437.
Feagan BG, McDonald JW, Panaccione R et al. Methotrexate in combination with infliximab is no more effective than infliximab alone in patients with Crohn’s disease. Gastroenterology. 2014;146:681–688.
Vermeire S, Noman M, Van Assche G et al. Effectiveness of concomitant immunosuppressive therapy in suppressing the formation of antibodies to infliximab in Crohn’s disease. Gut. 2007;56:1226–1231.
Carbonnel F, Colombel JF, Filippi J et al. Methotrexate is not superior to placebo for inducing steroid-free remission, but induces steroid-free clinical remission in a larger proportion of patients with ulcerative colitis. Gastroenterology. 2016;150:380–388.
Daperno M, D’Haens G, Van Assche G et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004;60:505–512.
Chande N, Wang Y, MacDonald JK, McDonald JW. Methotrexate for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2014;2014:CD006618.
Koh SJ, Hong SN, Park SK et al. Korean clinical practice guidelines on biologics for moderate to severe Crohn’s disease. Intest Res. 2022.
Hawthorne AB. Methotrexate: a useful alternative in Crohn’s disease? Gut. 2001;49:9–10.
Rampton DS. Methotrexate in Crohn’s disease. Gut. 2001;48:790–791.
Rosh JR. The current role of methotrexate in patients with inflammatory bowel disease. Gastroenterol Hepatol. 2020;16:43–46.
Narula N, Peyrin-Biroulet L, Colombel JF. Combination therapy with methotrexate in inflammatory bowel disease: time to COMMIT? Gastroenterology. 2014;146:608–611.
Colman RJ, Rubin DT. Optimal doses of methotrexate combined with anti-TNF therapy to maintain clinical remission in inflammatory bowel disease. J Crohns Colitis. 2015;9:312–317.
Borren NZ, Luther J, Colizzo FP et al. Low-dose methotrexate has similar outcomes to high-dose methotrexate in combination with anti-TNF therapy in inflammatory bowel diseases. J Crohns Colitis. 2019;13:990–995.
Henriksen M, Jahnsen J, Lygren I et al. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study. Gut. 2008;57:1518–1523.
Colombel JF, Sandborn WJ, Reinisch W et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–1395.
Armuzzi A, Pugliese D, Danese S et al. Long-term combination therapy with infliximab plus azathioprine predicts sustained steroid-free clinical benefit in steroid-dependent ulcerative colitis. Inflamm Bowel Dis. 2014;20:1368–1374.
Maeda T, Sakuraba H, Hiraga H et al. Long-term efficacy and tolerability of dose-adjusted thiopurine treatment in maintaining remission in inflammatory bowel disease patients with NUDT15 heterozygosity. Intest Res. 2022;20:90–100.
Kim YZ, Kang B, Kim ES, et al. Efficacy of combined initial treatment of methotrexate with infliximab in pediatric Crohn’s disease: a pilot study. Biomedicines. 2023;11.
Shea B, Swinden MV, Tanjong Ghogomu E et al. Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2013;2013:CD000951.
Reich K, Langley RG, Papp KA et al. A 52-week trial comparing briakinumab with methotrexate in patients with psoriasis. N Engl J Med. 2011;365:1586–1596.
Fournier MR, Klein J, Minuk GY, Bernstein CN. Changes in liver biochemistry during methotrexate use for inflammatory bowel disease. Am J Gastroenterol. 2010;105:1620–1626.
Saibeni S, Bollani S, Losco A et al. The use of methotrexate for treatment of inflammatory bowel disease in clinical practice. Dig Liver Dis. 2012;44:123–127.
Wahed M, Louis-Auguste JR, Baxter LM et al. Efficacy of methotrexate in Crohn’s disease and ulcerative colitis patients unresponsive or intolerant to azathioprine/mercaptopurine. Aliment Pharmacol Ther. 2009;30:614–620.
Seinen ML, Ponsioen CY, de Boer NK et al. Sustained clinical benefit and tolerability of methotrexate monotherapy after thiopurine therapy in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2013;11:667–672.
Park JJ, Yang SK, Ye BD et al. Second Korean guidelines for the management of Crohn’s disease. Intest Res. 2017;15:38–67.
Carter MJ, Lobo AJ, Travis SP, Ibd Section BSoG. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53:V1–V16.
Dignass A, Eliakim R, Magro F et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012;6:965–990.
Acknowledgments
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no competing interest.
Ethical considerations
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, J., Chun, J., Park, S.J. et al. Effectiveness and Tolerability of Methotrexate Combined with Biologics in Patients with Crohn’s Disease: A Multicenter Observational Study. Dig Dis Sci 69, 901–910 (2024). https://doi.org/10.1007/s10620-023-08237-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08237-0