Abstract
Background
Management of head and neck cancers requires a multidisciplinary approach where surgery followed by radio and chemotherapy is the mainstay of treatment. The above-mentioned treatment can cause mucositis, a severely debilitating side effect. This can have a significant impact on quality of life. A recent advancing mode of drug delivery is the bioadhesive system. This interacts with mucosa by adhering to it and thereby improving the efficacy of the therapeutic agent delivered.
Aim and objective
The purpose of this systematic review is to evaluate the effectiveness of bioadhesives in reducing oral mucositis and relieving pain associated with mucositis in head and neck cancer patients receiving radio-chemotherapy.
Materials and method
Studies assessing the effectiveness of bioadhesives for the treatment of radiation-induced oral mucositis were retrieved from specialized databases (PubMed/MEDLINE, Scopus, ProQuest, Google Scholar, LILACS, OpenGrey) as well as institutional repositories. Data on incidence, pain reduction, resolution, and improvement of oral mucositis using bioadhesive were compiled. A Cochrane tool was used for randomized controlled trials and a JBI tool for non-randomized controlled trials and observational studies to assess the quality of included studies. Based on the eligible study data, a meta-analysis was conducted with STATA version 16, 2019 software, and 95% confidence intervals and p values greater than 0.05.
Results
A total of 15 studies were included which assessed the effectiveness of bioadhesives in managing mucositis and its associated pain. Studies included in the review described either reduction, resolution, or incidence of oral mucositis respectively. A total of three meta-analyses were conducted to assess the incidence of oral mucositis and the pain associated with it, as well as the reduction in incidence. Bioadhesives showed statistically significant differences in the incidence of severe mucositis (p = 0.04). A meta-analysis comparing bioadhesives efficacy in reducing mucositis and pain associated with it found no statistically significant differences (p = 0.36).
Conclusion
Bioadhesives are emerging as a novel drug delivery method for treating radio-chemotherapy-induced oral mucositis because of their rapid absorption and easy application. Regardless of its benefits, clinical trials comparing it with conventional treatment methods are necessary to assess its efficacy in treating oral mucositis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancers (HNC) are the sixth most common cancer, with more than 800,000 diagnosed cases 2016 [1]. More than 90% of malignant tumors arise from the mucosal epithelium in the oral region known as squamous cell carcinomas (OSCC) while others include salivary minor glands, melanomas, and lymphomas. The development of oral cancer is primarily associated with smoking tobacco including smokeless tobacco and heavy alcohol consumption [2]. HNC has a 5-year survival rate of less than 50% after diagnosis, making it a disfiguring disease with a poor prognosis [3].
Locally advanced HNC often requires radiotherapy and concurrent systemic treatment (platinum-based chemotherapy) or surgery followed by radiotherapy with or without systemic therapy [4]. The cytotoxic effects of these therapies are not only limited to tumor cells but also act on normal tissues with high cell turnover [5]. The following adverse events have an impact on a patient’s quality of life: oral mucositis (OM), hyposalivation, loss of taste, dental caries, osteoradionecrosis, and trismus.
Ninety percent of HNC patients receiving standard radiotherapy and chemoradiotherapy will develop oropharyngeal mucositis [6]. Lesions occur commonly in non-keratinized oral mucosa, such as lip and buccal mucosa, lateral and anterior mucosa of the tongue, the floor of the mouth, and the soft palate [7]. Radiation therapy-induced OM depends on the dose administered, the fraction of the dose administered, the volume of the tissue treated, and the type of radiation used. Infections like HIV, collagen vascular disease, alcohol-based mouth rinses, and smoking habits can all contribute to the development of OM [8,9,10].
After radiation therapy, radio-induced OM typically lasts between 2 and 6 weeks [11, 12]. Radiation doses of 10 Gy cause hyperkeratinized lesions, and doses of 20 Gy cause erythema as an early sign of OM. A dose equal to or greater than 30 Gy leads to pseudomembrane-covered ulcers susceptible to super-infection due to bacterial colonization [11, 12]. Chemotherapy-induced OM is typically more aggressive than radiotherapy-induced OM. Erythema appears 5–8 days after treatment, followed by edema and ulceration 2 days later [11]. The symptoms of OM from both radiotherapy and chemotherapy can decrease the quality of life (QOL) of patients with HNC. OM can lead to great discomfort, pain, inability to eat, and secondary infections.
According to the Multinational Association for Supportive Care in Cancer and the International Society of Oral Oncology (MASCC/ISOO), the treatment for oral mucositis consists primarily of pain control, nutritional support, oral decontamination, palliation of dry mouth, and therapeutic interventions [13]. It has become paramount in clinical practices to design therapeutic interventions aimed at reducing the intensity or preventing OM. These interventions include a variety of agents such as cryotherapy [14], growth factors [15], anti-inflammatory agents [16], antioxidants [17], and photobiomodulation (low-level laser therapy) [18]. Although many treatment options exist to prevent and treat mucositis, there is no gold-standard protocol [19].
Oral mucoadhesive drug delivery is a promising alternative to conventional systems as it acts by the efficiency and residence time of the active compound at the absorption site through interaction with mucous layers. Oral mucoadhesive systems provide higher bioavailability and are ideal for preventing first-pass metabolism, allowing for direct and painless administration, and limiting undesirable systemic effects. There are various forms of these drugs available, such as tablets, semisolids, which are usually dissolved in aqueous or non-aqueous solutions, and liquids that can be applied orally throughout the buccal cavity [20].
This systematic review evaluated the efficacy of bioadhesives in reducing OM and relieving pain associated with oral mucositis in patients undergoing treatment for HNC. This systematic review will address the following questions.
-
1.
Can bioadhesives aid with pain relief in patients with OM caused by radio/chemotherapy for HNC?
-
2.
Do bioadhesives prevent/protect patients who are undergoing HNC therapy from developing OM?
Methodology
Eligibility criteria
By establishing inclusion and exclusion criteria, the population, intervention, comparison, outcome, and study design (PICOS) strategy was used to define the eligibility criteria as described in Table 1. Studies, where interventional trials were conducted with or without controls, either non-randomized or randomized, observational studies, and publications pertaining to the above-mentioned study design in scientific journals and gray literature that describe the patients undergoing chemotherapy and radiotherapy for HNC with OM treated with a bioadhesive.
Information sources
An extensive search was conducted in the following databases and repositories for articles relevant to the title and research question until 31st July 2022. Search engines such as PubMed/Medline, Google Scholar, ProQuest, Scopus, OpenGrey, Tamil Nadu Dr. MGR Medical University repository, Rajiv Gandhi University of Health Sciences repository, and KLE Academy of Higher Education and Research repository were sought. A literature search was performed on the topic by two independent researchers, JP and VK, with studies restricted to the English language. Literature saturation was also ensured by searching reference lists of included studies.
Search strategy
A combination of Boolean operators “AND” and “OR” specific to databases is used to match the medical subject headings (MeSH) and text words related to head and neck cancer, radiotherapy, chemotherapy, and oral mucositis with bioadhesives as separate search term. According to respective databases, the following filters were applied: PubMed–Human; Scopus–Full text; LILACS–All text; ProQuest–Full text and peer-reviewed/dissertations and thesis + scholarly articles + English language.
Selection process
The included studies were assessed by two observers, JP and VK, to determine whether they met the eligibility criteria. The full-text articles were read thoroughly, and any disputes were resolved by a third reviewer, VJ. In order to remove duplicates and manage references and bibliographies, Mendeley desktop application version 1.19.8 was used.
Data collection process and data items
The review team developed standardized data extraction sheet in Microsoft Excel (2007) format that were used independently by JP and VK to collect data from each study. Data items like author name, year of publication, sample size, age group, study design, control group, interventional group, reduction of mucositis and mucositis pain assessed using various grades or scales, the incidence of mucositis, resolution of mucositis, and adverse effects reported were recorded.
Study risk of bias assessment
Risk of bias assessment for included studies was done by JP and VJ. The Cochrane Handbook of Randomized Controlled Trials Tool was used in the RevMan application for studies using randomized controlled trials [21]. The Joanna Briggs Institute (JBI) critical appraisal checklist developed by the Faculty of Health Sciences at the University of Adelaide was used to assess bias in non-randomized controlled trials [22] and observational studies [23]. To resolve any disagreement, a third reviewer (VK) was consulted.
Effect measures
The standardized mean difference (SMD) of reduction in oral mucositis and pain associated with it was utilized as the main effect measure. This meta-analysis included the studies which provided mean and standard deviation values for weekly or overall reduction between control and treatment groups. According to data provided regarding the incidence of mucositis in both control and treatment groups, the relative risk (RR) was calculated. Meta-analysis for incidence of non-severe oral mucositis (WHO grades 0, 1, 2 and RTOG/EORTC grades 1, 2) and severe oral mucositis (WHO grades 3, 4 and RTOG/EORTC grades 3, 4) was carried out. The other relevant data were described and used for narrative synthesis.
Synthesis methods
The meta-analysis was conducted with STATA (Software for statistics and data science by StataCorp LLC, Texas, USA version 16, 2019) provided that at least 2 studies fell under the particular analysis category.
I-squared (I2) statistics were utilized to assess heterogeneity between the included studies with a 95% confidence interval (95% CI). In the meta-analysis, the incidence of mucositis, reduction of mucositis, and pain associated with mucositis were compared between the intervention (bioadhesives) and control group. Studies’ consistency can be affected by variations in participants, outcomes, interventions, or evaluation methods of interventions, resulting in heterogeneity. Therefore, a fixed-effect model that represents a typical intervention effect or a random-effect model that presents the average intervention effect will be used in the meta-analysis.
Reporting bias assessment
A funnel plot analysis was used to assess publication bias. The substantial bias in meta-analysis is assessed by analyzing how the studies are distributed either symmetrical or asymmetrical within the inverted funnel, where they are expected to lie without heterogeneity and reporting biases.
Certainty assessment
To determine whether the true effect is within a particular range or relative to the threshold, Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) was used. Using the GRADE [24] approach, we assessed the certainty of the evidence, formulated recommendations, and checked the applicability in evidence-based medicine.
Results
The search strategy yielded 97,842 results from 7 databases and 2 university repositories. A total of 49 articles were selected after screening all the titles, excluding those that had other study designs, titles unrelated to the present review, articles with inappropriate outcome measures, articles that were published in other categories (case report, case series, etc.), and articles not written in English. It was found that 24 articles were non-retrievable. After removing the duplicates, the total was reduced to 25 articles. The abstracts of 25 articles were read, of which 7 articles were excluded (2 animal studies that examined mucoadhesiveness and drug release properties in mice; one study used frozen pig buccal mucosa; two in vitro studies were conducted—one using various incubation mixtures to evaluate bioadhesiveness of chitosan and melatonin and another using rheometers, tension tests, and saliva samples of an admixture paste to evaluate viscosity, adhesiveness, and elution; 2 studies were review articles), resulting in 18 articles. A full-text screening of 18 articles excluded 3 articles related to other neoplasms including HNC. Based on the results of this systematic review, 15 articles met the eligibility criteria, and 8 studies were included in the meta-analysis (Fig. 1).
Study characteristics
Based on the search strategy, 15 eligible articles were included in this review (Table 2); 9 [25,26,27,28,29,30,31,32,33] were histopathologically confirmed cases of HNC, including oral squamous cell carcinoma, malignant lymphoma, and nasopharyngeal carcinoma.
A total of 11 studies [25, 29, 30, 32,33,34,35,36,37,38,39] mentioned the site of HNC as the tongue, buccal mucosa, oropharynx, nasopharynx, hypopharynx, and salivary gland, whereas 4 studies [26,27,28, 31] did not mention the site of the tumor. Based on the number of subjects included by site, 172 cases of oral cancer have been reported, 47 have been reported as tongue cancer, 38 have been reported as laryngeal carcinoma, 127 have been reported as oropharyngeal carcinoma, 20 hypopharyngeal carcinomas, and 38 have been reported as carcinoma of the nasopharynx.
In total, 763 patients participated in this study, including 302 in the control group and 461 in the intervention group. In these included studies, the age group of patients was in the range of 18–59 years where 487 were males and 189 were females. Based on the geographic location of the studies, 3 each were carried out in Japanese [32, 38, 39] population; 2 studies each were conducted in Iranian [27, 28] and Spanish [26, 29] populations; 1 study each in Chinese [33], Indian [30], Italian [34], Bulgarian [37], Brazilian [31], American [25], and British [35] population and a multicentric study [36] involving French, German, Spanish, and American population.
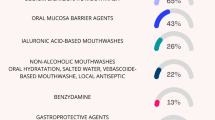
As part of the intervention group, bioadhesive barriers were provided as gel [25, 26, 29, 31, 34, 35], spray [33], adhesive film [27, 28, 32], tablet [36], mouthwash [25, 35, 38], and wafer [30]. As interventions, Episil® [33, 38, 39], Mucotrol™ [30], Tetracaine [33], MuGard [25], Melatonin [29], Clonidine [36], Propolis [31], Gelclair [35], Chlorhexidine [26], Triamcinolone acetonide [27, 28], MF-5232 [30], and CAM2028-Benzydamine [37] were used.
The site of the irradiation was mentioned in a single study [38]. There is a direct correlation between radiation doses and their duration in the development of OM. All the studies included the conventional or hyperfractionization method. A range of doses was given five times per week including 1.2 to 1.5 Gy [34], 1.8 Gy [31], 1.8 to 2.2 Gy [36], 2 Gy [27, 28, 32, 38], and 2 to 2.2 Gy [25, 29].
In order to deliver radiation to the tissues, a variety of radiation delivery techniques were employed. 3DCRT (three-dimensional conformal radiation therapy) was utilized in 3 studies [36, 38, 39]; IMRT (intensity-modulated radiation therapy) was utilized in 3 studies [36, 38, 39]; two-dimensional cobalt-based therapy was utilized in 2 studies [27, 28]; Brachytherapy was utilized in 1 study [32]; VMAT-SIB (Volumetric Modulated Arc Therapy-Simultaneous Integrated Boost) was utilized in 2 studies [29, 33]; External beam photon therapy was utilized in 3 studies [25, 30, 33]; conventional fractional therapy was utilized in 2 studies [26, 34].
In addition to radiotherapy, various chemotherapeutic agents were utilized in 11 studies [25,26,27, 29, 30, 32,33,34, 36, 38, 39]. Cisplatin was administered at 30 mg/m2 [33, 34, 36, 38, 39], 50 mg/m2 [30], and 100 mg/m2 [26, 29]. Tegafur-gimeracil-oteracil-potassium was administered at 80 mg/m2 [33, 38]. Cetuximab was administered at 400 mg/m2/w and 250 mg/m2/w [29, 38]. Peplomycin 5 mg was administered intravenously [32]. UFT was administered at 200 mg/day [33]; 5-fluorouracil [34] and carboplatin [34, 39] were also administered. The primary outcomes were the reduction in pain associated with OM and the incidence or reduction of OM.
The safety of the interventions provided was evaluated based on their potential to cause local or systemic adverse effects in the studies that were included. In two studies, there were no adverse effects [32, 34]. Several local adverse effects have been reported, such as xerostomia [29, 33, 36], burning sensation [34, 40], mild inflammation, and stinging in the mouth [35].
There were several systemic adverse effects associated with the therapy, including nausea [25, 29, 33, 36, 37, 39], vomiting [25, 29, 33, 36, 37], dysphagia [36], diarrhea [25, 29, 36], constipation [25, 29, 36]; blood-related disorders such as neutropenia [25, 29, 33, 36], leukopenia [36], thrombocytopenia [33], and anemia [29]; metabolic disorders such as dehydration [38] and weight loss [36]; and infectious complications, such as oral candidiasis [36], fungal infection [36], and other infections [26, 36].
According to various studies, compliance with bioadhesives is measured in terms of tolerability and factors contributing to discontinuation. Several studies stated that the application of the product was difficult [31, 34, 38]; there were also reports of dysgeusia [34, 38] and a dislike of the smell [38] product. Lack of compliance and patient decision resulted in discontinuing the treatment [29]. Some studies did not measure patients’ compliance with the treatment provided [26,27,28, 30, 33, 35, 39].
Risk of bias in studies
JP and VJ independently assessed the quality of included studies. In case of disagreement, VK acted as a moderator whenever there was a disagreement.
Quality assessment of randomized controlled trials
A total of 15 studies were included, of which 10 were randomized controlled trials [25,26,27,28,29,30, 35,36,37, 39]. In order to perform Cochrane’s tool for randomized controlled trials, RevMan software was used (version 5.4.1). It consists of the following domains.
Selection bias
All the included studies [25,26,27,28,29,30, 35,36,37, 39] showed adequate randomization methods resulting in a low risk of bias. Regarding allocation concealment, three types were used: sealed envelopes [26], an open-labeled method [39], and a code system [36], while allocation concealment was not clearly mentioned in 3 studies [25, 30, 35] and allocation concealment was not carried out in 4 studies [27,28,29, 39].
Performance bias
In 8 studies [25,26,27,28,29,30, 36, 37], both participants and personnel were blinded, whereas blinding only participants was carried out in a study [35], thereby revealing a low risk of bias in 9 out of 10 included studies. There was no blinding in the study [39], leading to a high risk of bias.
Detection bias
Except for one article where the outcome assessment was blinded [36], we judge that the outcome measurement was unlikely to be influenced by the lack of blinding of outcome assessment in 3 studies [27, 28, 37]. Six studies [25, 26, 29, 30, 35, 39] have not mentioned blinding of outcome assessment thereby indicating a high risk of bias.
Attrition bias
There was no reported risk of bias in any of the included studies because all participants completed the clinical trial [25,26,27,28,29,30, 35,36,37, 39].
Reporting bias
Considering all of the included studies reported every planned outcome including primary as well as secondary outcomes, the results were adjudged to be low in bias [25,26,27,28,29,30, 35,36,37, 39].
Other bias
There was a low risk of bias in all the included studies due to the lack of other sources of bias [25,26,27,28,29,30, 35,36,37, 39].
The overall risk of bias
The overall risk of bias was low for 1 study [36], unclear risk of bias for 1 study [37], and high risk of bias (because of selection bias, performance bias, and detection bias) for 8 studies [25,26,27,28,29,30, 35, 39]. Review of authors’ judgments about each risk of bias item appears as percentages in Fig. 2, illustrated as a graph of risk of bias. Figure 3 presents the summary of bias judgments made by the review authors about each included study’s risk of bias item.
Quality assessment of non-randomized controlled trials and observational studies
Critical appraisal tool from the Joanna Briggs Institute (JBI) was used for non-randomized controlled trials [22] and observational studies [23]. Positive responses that were under 49% were considered to have a high risk of bias and low quality; those between 50% and 69% were considered to have a moderate risk of bias and moderate quality, and those above 80% were considered to have a low risk of bias with high quality. Considering the above-mentioned criteria, three non-randomized controlled trials [32, 33, 38] and two observational studies [31, 34] are of high quality as depicted in Table 3.
Results of synthesis
It was found that 8 articles were eligible for meta-analysis. Meta-analysis was conducted using standardized mean difference for 2 studies and risk ratios for the remaining 6 studies. The random-effect method and the fixed-effect method will give identical results when there is no heterogeneity among the studies. Since there is considerable heterogeneity, a random-effect meta-analysis will award relatively more weight to smaller studies than a fixed-effect meta-analysis. This systematic review used a random-effect model, as heterogeneity was not considered. There is evidence that triamcinolone acetonide mucoadhesive films reduce OM grading more effectively than placebo in two randomized controlled trials [27, 28]. Despite the high heterogeneity and no statistically significant differences, the experimental group demonstrated a significant reduction in OM (p = 0.36; SMD = 0.49; 95% CI = −0.55, 1.52; I2 = 87%) as depicted in Fig. 4.
In another meta-analysis, triamcinolone acetonide mucoadhesive films were compared to a placebo for relieving pain associated with OM [27, 28]. Results indicated a favorable outcome for the experimental group as depicted in Fig. 5, yet no statistically significant difference was found between the experimental and control group (p = 0.36; SMD = 0.77; 95% CI = −0.87, 2.40; I2 = 94%).
Six studies were reviewed to determine whether experimental groups containing various bioadhesives had greater success in detecting severe OM compared to control groups [21, 26, 29, 32, 33, 36] which demonstrated statistically significant differences with considerable heterogeneity (p=0.04; RR=1.23; 95% CI=1.01, 1.49; I2=57%) as shown in Fig. 6.
Reporting biases
For studies that assessed the incidence of OM, a funnel plot was generated using fixed effects, which indicated some asymmetry caused by the small study effects or by publication bias, as shown in Fig. 7.
Certainty of evidence
According to the GRADE method, when comparing bioadhesives with placebos and matched controls, the overall probability of the evidence was moderate. Based on Table 4, it shows that bioadhesives can serve as an alternative to conventional treatment methods by showing a close match with the estimated effect, which proves that bioadhesives are an effective alternative. The quality of the evidence was assessed for each study, and three studies [27, 28, 31] were found to have high certainty of evidence. Eight studies [20,21,22,23,24,25, 32, 33] were rated as moderate in the certainty of evidence because of bias, i.e., allocation concealment not mentioned [20, 22,23,24,25], detection bias [20,21,22,23,24,25], and measurement of outcome [32, 33]. A low certainty of the evidence was reported in four studies [26, 29, 30, 34] as shown in Table 5.
Discussion
The incidence of oral cancer is among the top ten most common cancers in the world, with late clinical detection, a poor prognosis, specific biomarkers for the disease, and costly therapeutic alternatives [39]. Combining radiation therapy and chemotherapy is the most widely used intervention for the management of oral and HNC. It is well known that these treatments improve the QOL and extend the life expectancy of the patients; however, they are often associated with adverse effects [40]. One of the most painful and debilitating adverse effects of radiation and chemotherapy is OM [41, 42]. In severe cases, OM also causes unrelenting pain, inability to eat or drink, weight loss, and reduced QOL [43, 44]. This is caused by oxidative damage, which releases reactive oxygen species (ROS) that cause inflammatory cytokines to activate causing DNA damage and resulting in cell death [45].
Mucositis is managed with an intensive oral care protocol, antimicrobial, anti-inflammatory, cytoprotective agents, dietary supplements, biostimulants, and natural and homeopathic agents [46,47,48,49]. In order to increase the effectiveness of a variety of therapeutic agents, a new method of localized drug delivery was developed in the form of bioadhesives or mucoadhesives that adhere to the oral mucosa upon application.
Current MASCC/ISOO guidelines do not address the efficacy of bioadhesive barrier-forming oral liquids. It is because there is insufficient proof that using these products reduces the severity of OM, although some of these oral care products provide comfort to patients [49]. A topical oral mucosal protectant such as Caphosol®, MuGard®, Oralife®, Gelclair®, and Episil® is suggested by the European Oral Care in Cancer Group and the UK Oral Mucositis in Cancer Group for mild to moderate OM [50, 51].
A gel formulation is a semisolid mucoadhesive that has several advantages, including rapid drug release, ease of preparation and administration, increased biocompatibility, and easy dispersal throughout the oral mucosa, allowing it to adhere to the oral mucosa and reducing the risk of irritative or allergic reactions [52]. Six of the 15 included studies [21, 25, 26, 29, 34, 35] used bioadhesive gel to treat OM. According to two studies [26, 35], the intervention was equally effective in managing OM and reducing pain as standard therapy. There was a consistent reduction in OM incidence in a phase II trial [29]. In the remaining studies [25, 34], bioadhesive gels were found to be safe in delaying the progression of OM and improving its symptoms.
Patches and films are semisolid preparation that comes in an elliptical shape and can range from 1 to 3 cm in size, and they are used to deliver drugs directly to the mucosal membrane [53]. There were three studies [27, 28, 32] that used mucoadhesive patches or films, two of which contained triamcinolone acetonide [27, 28]. Triamcinolone acetonide film was proven to be effective in reducing the OM grade and associated pain with it. Film-based adhesives were effective at relieving pain when topical anesthetics and antibiotics were combined in a water-soluble film [32].
Lipid-based solutions such as phospholipid and diglycerides can effectively relieve intraoral pain due to their unique bioadhesive properties [54]. The Episil® is a bioadhesive lipid-based solution containing soybean lecithin and diolein which forms a protective barrier within five minutes upon contact with oral mucosa, thereby having a local analgesic effect [38]. The results of three studies [33, 38, 39] utilizing Episil® showed that it effectively improved OM and the pain it causes. A study that used CAM-2028 [37] demonstrated clinically significant pain relief for up to eight hours.
Drug-loaded wafers can provide a mucoadhesive layer while providing prolonged and stable drug release [55]. A study [30] concluded Mucotrol™ (MF 5232), a polyherbal formulation containing Polygonum cuspidatum, Angelica sp., Camellia sinensis, Cyamopsis tetragonolobus, Centella asiatica, and Aloe sp. and glycyrrhizin. Beneficial activity in OM is owing to its antioxidant, analgesic, immunomodulatory, and wound healing properties.
Tablets are a solid form of mucoadhesive system that can be applied both topically and systemically. Bioadhesive polymers can be used to form a matrix for drug delivery that incorporates the active ingredient into the tablet [56]. According to a study [36], mucoadhesive tablet containing Clonidine which is known for its anti-hypertensive and anti-inflammatory activity showed a favorable effect on OM severity and course.
This systematic review included studies with a variety of study designs. According to the quality assessment, a study [36] had a low risk of bias and was of high quality. Similarly, a study [37] carried an unclear risk of bias as the participants, presenter, and outcome assessor were not blinded. The remaining 8 [25,26,27,28,29,30, 35, 39] out of 10 studies were judged to have a high risk of bias due to insufficient information regarding methods for assigning patients to experimental and control groups and the absence of blinding of participants, personnel, or outcome assessor. A total of three studies that were non-randomized [32, 33, 38] and two studies that were observational [31, 34] have been found to be of high quality. Therefore, studies included with their results can be considered for potential clinical significance.
The findings of this systematic review and meta-analysis have several strengths, including a comprehensive literature search, the inclusion of studies conducted using different bioadhesive systems, and the results of qualitative and quantitative synthesis. It is important to note, however, certain limitations apply to the results of this systematic review. Studies published in the English language were included in this review with results obtained in other languages being excluded leading to selection bias.
Limitations
The heterogeneity among the included studies is one of the limitations of this systematic review. There were heterogeneities noted in the study design, sample size, radiation delivery method, pain assessment tools, data presentation regarding OM, and adverse effects. It was important to note that different types of study designs were utilized in this systematic review. In most of the included studies, randomized or non-randomized controlled trials were used while only a few were observational studies. An evidence-based approach places randomized controlled trials at the top of the pyramid as the ideal study design for comparing the effectiveness of two different interventions, but studies other than these can have an impact on the outcome as well.
The limited sample size is another factor that should be considered as 2 out of 15 included studies used a sample size of 15 or fewer patients. It was also noted that experimental and control samples were distributed unequally, which could contribute to heterogeneity. Mucositis may be influenced by the method of radiation delivery to the patient. There are differences between radiotherapy methods in the included studies, which range from larger fields of treatment using conventional or cobalt machines to a smaller field using IMRT, which raises the question whether this is a confounding factor.
In this systematic review, the efficacy of various bioadhesive systems was compared. The treatment group contains various forms of bioadhesives, such as gels, wafers, and films, having a control group in a similar form to that of the intervention provided should be used for accurate comparison. Furthermore, differences in the duration of intervention and control contribute to heterogeneity.
Assessment of OM uses various scales like WHO, RTOG, and NCI, and assessment of pain due to OM was measured using WHO, Likert, VAS, and RTOG scales, which may result in heterogeneity. In included studies, data were presented on the incidence of severe OM, reduction in OM, reduction or improvement of pain, and number of days until OM and pain associated with it resolved, as well as improvement of pain or OM with intervention. As a result, heterogeneity can be observed as different methods of measurement were used to present the data.
The studies included did not precisely describe how secondary outcomes, such as adverse reaction and interruptions of radiotherapy, were measured. The efficacy of the intervention as well as adverse effects of the treatment was not assessed through long-term follow-ups of the patients. Also, the clinical and oncological safety of the bioadhesives was not assessed.
A major limitation of this systematic review was the methodological quality of the studies that were included in it. Even though 6 out of the 15 studies included in this review were of high quality, selection, performance, and detection bias compromises the internal validity of results in remaining 9 studies, which subsequently makes it difficult to draw a robust conclusion from these studies.
Suggestions
Studies in the future should have a randomized controlled study design with improved sample size and similar forms of bioadhesives both in the treatment and control groups. In order to evaluate the effectiveness of bioadhesive systems for the reduction of mucositis or the relief of pain, two different bioadhesive systems utilizing the same intervention agent should be compared. For assessment of the recurrence of the lesion or adverse effects, a longer follow-up period of the patient’s post-intervention or treatment duration is required.
In order to avoid heterogeneity, common assessment tools can be used to assess OM and pain associated with it. A single tool can be used for assessing the incidence of OM or reduction in OM for the purposes of evaluating the efficiency of bioadhesives in relation to pain associated with OM. As an alternative and promising therapeutic modality for the management of OM in patients with HNC, cost-effectiveness regarding the manufacturing of various adhesive systems and accessibility are factors that should be considered.
Implications for practice and research
The bioadhesive drug delivery system appears to be one of the most promising systems as it has shown positive preliminary results. Based on the data from included studies, it is predicted that the outcome of this study will be positive. This is due to the substantial reduction in the incidence of OM, associated pain, and the frequency of OM in the bioadhesive group compared to the placebo in this study. Moreover, the certainty evidence revealed a higher degree of certainty providing valuable insight regarding the potential use of these modalities in the treatment of OM and other oral mucosal lesions.
Conclusion
The findings of this multiendpoint systematic review indicate that bioadhesives can be used as an alternative treatment option for patients with OM caused by radiotherapy or chemotherapy in the treatment of HNC in most cases. Several clinical outcomes suggest that bioadhesives can considerably reduce pain and OM while being less likely to cause adverse effects compared to systemic therapy. However, due to the observed heterogeneity of the results, it is recommended to conduct further well-designed studies with long-term treatment and follow-up on the subjects.
References
Fitzmaurice C (2018) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 2006 to 2016: a systematic analysis for the Global Burden of Disease study. Clin Oncol 20(36):1568–1568. https://doi.org/10.1200/jco.2018.36.15_suppl.1568
Mehanna H, Paleri V, West CML, Nutting C (2011) Head and neck cancer-part 1: epidemiology, presentation, and preservation. Clin Otolaryngol 36:65–68. https://doi.org/10.1111/j.1749-4486.2010.02231.x
Pignon J-P, le Maître A, Maillard E, Bourhis J (2009) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiat Oncol J 92:4–14. https://doi.org/10.1016/j.radonc.2009.04.014
Lo Nigro C, Denaro N, Merlotti A, Merlano M (2017) Head and neck cancer: improving outcomes with a multidisciplinary approach. Cancer Manag Res 9:363–371. https://doi.org/10.2147/cmar.s115761
D’Hondt L, Lonchay C, Andr M, Canon J-L (2006) Oral mucositis induced by anticancer treatments: physiopathology and treatments. Ther Clin Risk Manag 2:159–168. https://doi.org/10.2147/tcrm.2006.2.2.159
Kin-fong Cheng K, Ka Tsui Yuen J (2006) A pilot study of chlorhexidine and benzydamine oral rinses for the prevention and treatment of irradiation mucositis in patients with head and neck cancer. Cancer Nurs 29:423–430. https://doi.org/10.1097/00002820-200609000-00012
Stokman MA, Spijkervet FKL, Boezen HM, Schouten JP, Roodenburg JLN, de Vries EGE (2006) Preventive intervention possibilities in radiotherapy- and chemotherapy-induced oral mucositis: results of meta-analyses. J Dent Res 85:690–700. https://doi.org/10.1177/154405910608500802
Rubenstein EB, Peterson DE, Schubert M et al (2044) Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer 101(8):1921–1921. https://doi.org/10.1002/cncr.20664
Khammissa RAG, Wood NH, Meyerov R, Lemmer J, Raubenheimer EJ, Feller L (2011) primary oral tuberculosis as an indicator of HIV infection. Pathol Res Pract 2011(20):1–4. https://doi.org/10.4061/2011/893295
Hejna M, Köstler WJ, Raderer M, Steger GG, Brodowicz T, Scheithauer W et al (2001) Decrease of duration and symptoms in chemotherapy-induced oral mucositis by topical GM-CSF. Eur J Cancer 37:1994–2002. https://doi.org/10.1016/s0959-8049(01)00132-0
Sonis ST (2004) The pathobiology of mucositis. Nat Rev Cancer 4:277–284. https://doi.org/10.1038/nrc1318
Lanzos I, Herrera D, Santos S, Connor A, Pena C, Lanzos E et al (2010) Mucositis in irradiated cancer patients: effects of an antiseptic mouthrinse. Medicina Oral Patología Oral y Cirugia Bucal, pp e732–e738. https://doi.org/10.4317/medoral.15.e732
Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. dental clinics of North America. 2008;52(1):61–77. https://doi.org/10.1016/j.cden.2007.10.002
Riley P, Glenny A-M, Worthington HV, Littlewood A, Clarkson JE, MG MC (2015) In: Riley P (ed) Interventions for preventing oral mucositis in patients with cancer receiving treatment: oral cryotherapy. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd011552
Raber-Durlacher JE, von Bültzingslöwen I, Logan RM, Bowen J, Al-Azri AR et al (2012 Sep 18) Systematic review of cytokines and growth factors for the management of oral mucositis in cancer patients. Support Care Cancer 21(1):343–355. https://doi.org/10.1007/s00520-012-1594-5
Ariyawardana A, Cheng KKF, Kandwal A, Tilly V, Al-Azri AR et al (2019) Systematic review of anti-inflammatory agents for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3985–3995. https://doi.org/10.1007/s00520-019-04888-w
Raza A, Karimyan N, Watters A, Emperumal CP, Al-Eryani K, Enciso R (2022 Jun 10) Efficacy of oral and topical antioxidants in the prevention and management of oral mucositis in head and neck cancer patients: a systematic review and meta-analyses. Supportive Care in Cancer 30(11):8689–8703. https://doi.org/10.1007/s00520-022-07190-4
Campos TM, do Prado Tavares Silva CA, APT S, Sobral SS, MFSD R, Bussadori SK et al (2020) Photobiomodulation in oral mucositis in patients with head and neck cancer: a systematic review and meta-analysis followed by a cost-effectiveness analysis. Support Care Cancer 28(12):5649–5659. https://doi.org/10.1007/s00520-020-05613-8
De Sanctis V, Bossi P, Sanguineti G, Trippa F, Ferrari D, Bacigalupo A et al (2016) Mucositis in head and neck cancer patients treated with radiotherapy and systemic therapies: literature review and consensus statements. Crit Rev Oncol Hematol 100:147–166. https://doi.org/10.1016/j.critrevonc.2016.01.010
Massa S, Fouad A, Ebrahimi M, PLS M (2021) Emerging trends in oral mucoadhesive drug delivery for head and neck cancer. In: Early Detection and Treatment of Head & Neck Cancers. Springer, pp 199–217. https://doi.org/10.1007/978-3-030-69852-2_9
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj 18:343. https://doi.org/10.1136/bmj.d5928
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L (2019) Chapter 3: systematic reviews of effectiveness. JBI Reviewer’s Manual. https://doi.org/10.46658/jbirm-17-03
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetic R et al (2019) Chapter 7: systematic reviews of etiology and risk. JBI Reviewer’s Manual. https://doi.org/10.46658/jbirm-17-06
GRADE Working Group (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490. https://doi.org/10.1136/bmj.328.7454.1490
Allison RR, Ambrad AA, Arshoun Y, Carmel RJ, Ciuba DF, Feldman E et al (2014) Multi-institutional, randomized, double-blind, placebo-controlled trial to assess the efficacy of a mucoadhesive hydrogel (MuGard) in mitigating oral mucositis symptoms in patients being treated with chemoradiation therapy for cancers of the head and neck. Cancer 11(120):1433–1440. https://doi.org/10.1002/cncr.28553
Diaz-Sanchez RM, Pachon-Ibanez J, Marin-Conde F, Rodriguez-Caballero A, Gutierrez-Perez JL, Torres-Lagares D (2015) Double-blind, randomized pilot study of bioadhesive chlorhexidine gel in the prevention and treatment of mucositis induced by chemoradiotherapy of head and neck cancer. Medicina Oral Patología Oral y Cirugia Bucal, pp e378–e385. https://doi.org/10.4317/medoral.20338
Isfahani M, Pakravan F, Ghalayani P, Emami H, Noorshargh P (2019) A novel formulation for radiotherapy-induced oral mucositis: triamcinolone acetonide mucoadhesive film. J Res Med Sci 24:63. https://doi.org/10.4103/jrms.jrms_456_18
Ghalayani P, Emami H, Pakravan F, Nasr Isfahani M (2014) Comparison of triamcinolone acetonide mucoadhesive film with licorice mucoadhesive film on radiotherapy-induced oral mucositis: a randomized double-blinded clinical trial. Asia Pac J Clin Oncol 13(2):e48–e56. https://doi.org/10.1111/ajco.12295
Lozano A, Marruecos J, Rubió J, Farré N, Gómez-Millán J, Morera R et al (2021) Randomized placebo-controlled phase II trial of high-dose melatonin mucoadhesive oral gel for the prevention and treatment of oral mucositis in patients with head and neck cancer undergoing radiation therapy concurrent with systemic treatment. Transl Oncol 18(23):1801–1810. https://doi.org/10.1007/s12094-021-02586-w
Naidu MU, Ramana GV, Ratnam SV, Sudhavani T, Jaganath K, Naidu R, Roy P, Suresh P, Rani PU, Mohan IK (2005) A Randomised, double-blind, parallel, placebo-controlled study to evaluate the efficacy of MF 5232 (Mucotrol™), a concentrated oral gel wafer, in the treatment of oral mucositis. Drugs in R & D 6:291–298. https://doi.org/10.2165/00126839-200506050-00005
Noronha V, Araujo G, Gomes R, Iwanaga S, Barbosa M, Abdo E et al (2014) Mucoadhesive propolis gel for prevention of radiation-induced oral mucositis. Curr Clin Pharmacol 5(9):359–364. https://doi.org/10.2174/1574884709666140205210051
Oguchi M, Shikama N, Sasaki S, Gomi K, Katsuyama Y, Ohta S, Takei K, Arakawa K, Sone S (1998) Mucosa-adhesive water-soluble polymer film for treatment of acute radiation-induced oral mucositis. Int J Radiat Oncol Biol Phys 15(40):1033–1037. https://doi.org/10.1016/s0360-3016(97)00903-6
Wei J, Wu J, Wang H, Wang B, Zhao T, Meng L et al (2021) A bioadhesive barrier-forming oral liquid gel improved oral mucositis and nutritional status in patients with head and neck cancers undergoing radiotherapy: a retrospective single center study. Front Oncol 22:11. https://doi.org/10.3389/fonc.2021.617392
Alterio D, Jereczek-Fossa BA, Zuccotti GF, Leon ME, Omodeo Sale E, Pasetti M et al (2006) Tetracaine oral gel in patients treated with radiotherapy for head-and-neck cancer: final results of a phase II study. Int J Radiat Oncol Biol Phys 64:392–395. https://doi.org/10.1016/j.ijrobp.2005.07.301
Barber C, Powell R, Ellis A, Hewett J (2006) Comparing pain control and ability to eat and drink with standard therapy vs Gelclair: a preliminary, double centre, randomised controlled trial on patients with radiotherapy-induced oral mucositis. Support Care Cancer 28(15):427–440. https://doi.org/10.1007/s00520-006-0171-1
Giralt J, Tao Y, Kortmann R-D, Zasadny X, Contreras-Martinez J, Ceruse P et al (2020) Randomized phase 2 trial of a novel clonidine mucoadhesive buccal tablet for the amelioration of oral mucositis in patients treated with concomitant chemoradiation therapy for head and neck cancer. Int J Radiat Oncol Biol Phys 106:320–328. https://doi.org/10.1016/j.ijrobp.2019.10.023
Hadjieva T, Cavallin-Ståhl E, Linden M, Tiberg F (2014) Treatment of oral mucositis pain following radiation therapy for head-and-neck cancer using a bioadhesive barrier-forming lipid solution. Support Care Cancer 18(22):1557–1562. https://doi.org/10.1007/s00520-014-2117-3
Kabasawa Y, Ito K, Tokura S, Takazawa I, Yoshida N, Nakanishi T et al (2022) Clinical investigation of use of Episil® oral solution in oral mucositis during radiotherapy for head and neck cancer, vol 14. research square. https://doi.org/10.21203/rs.3.rs-1210506/v1
Soutome S, Yanamoto S, Kawashita Y, Yoshimatsu M, Murata M, Kojima Y et al (2021) Effects of a bioadhesive barrier-forming oral liquid on pain due to radiation-induced oral mucositis in patients with head and neck cancer: a randomized crossover, preliminary study. J Dent Sci 16:96–100. https://doi.org/10.1016/j.jds.2020.07.006
Naidu MUR, Ramana GV, Rani PU, Mohan Iyyapu K, Suman A, Roy P (2004) Chemotherapy-induced and/or radiation therapy-induced oral mucositis-complicating the treatment of cancer. Neoplasia 6:423–431. https://doi.org/10.1593/neo.04169
Raber-Durlacher JE, Elad S, Barasch A (2010) Oral mucositis. Oral Oncol 46:452–456. https://doi.org/10.1016/j.oraloncology.2010.03.012
Sonis ST (2009) Mucositis: the impact, biology and therapeutic opportunities of oral mucositis. Oral Oncol 45:1015–1020. https://doi.org/10.1016/j.oraloncology.2009.08.006
Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein EB (2003) The burdens of cancer therapy. Cancer 18(98):1531–1539. https://doi.org/10.1002/cncr.11671
Nonzee NJ, Dandade NA, Markossian T, Agulnik M, Argiris A, Patel JD et al (2008) Evaluating the supportive care costs of severe radiochemotherapy-induced mucositis and pharyngitis. Cancer 15(113):1446–1452. https://doi.org/10.1002/cncr.23714
Yuan A, Sonis S (2014) Emerging therapies for the prevention and treatment of oral mucositis. Expert Opinion on Emerging Drugs 8(19):343–351. https://doi.org/10.1517/14728214.2014.946403
Worthington HV, Clarkson JE, Bryan G, Furness S, Glenny A-M, Littlewood A et al (2010) In: Worthington HV (ed) Interventions for preventing oral mucositis for patients with cancer receiving treatment, vol 8. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd000978.pub4
Kassab S, Cummings M, Berkovitz S, van Haselen R, Fisher P (2009) Homeopathic medicines for adverse effects of cancer treatments, vol 15. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd004845.pub2
Stokman MA, Spijkervet FKL, Boezen HM, Schouten JP, Roodenburg JLN, de Vries EGE (2006) Preventive intervention possibilities in radiotherapy- and chemotherapy-induced oral mucositis: results of meta-analyses. Dent Res J 85:690–700. https://doi.org/10.1177/154405910608500802
Quinn B, Botti S, Kurstjens M, Marguiles A, Orlando L, Potting C, et al. European oral care in cancer group oral care guidance and support contents. 1st ed
UK Oral Mucositis in Cancer Group Oral Mucositis Guidelines. (2015) Mouth care guidance and support in cancer and palliative care. http://www.ukomic.co.uk/documents/UK_OM_Guidelines.pdf. Accessed 27 Dec 2022
Murdock JL, Reeves DJ (2019) Chemotherapy-induced oral mucositis management: a retrospective analysis of MuGard, Caphosol, and standard supportive care measures. J Oncol Pharm Pract 29(26):521–528. https://doi.org/10.1177/1078155219850298
Fini A, Bergamante V, Ceschel GC (2011) Mucoadhesive gels designed for the controlled release of chlorhexidine in the oral cavity. Pharmaceutics 3:665–679. https://doi.org/10.3390/pharmaceutics3040665
Karki S, Kim H, Na S-J, Shin D, Jo K, Lee J (2016) Thin films as an emerging platform for drug delivery. Asian J Pharm Sci 11:559–574. https://doi.org/10.1016/j.ajps.2016.05.004
Barauskas J, Christerson L, Wadsäter M, Lindström F, Lindqvist A-K, Tiberg F (2014) Bioadhesive lipid compositions: self-assembly structures, functionality, and medical applications. Mol Pharmaceutics 27(11):895–903. https://doi.org/10.1021/mp400552u
Timur SS, Yüksel S, Akca G, Şenel S (2019) Localized drug delivery with mono and bilayered mucoadhesive films and wafers for oral mucosal infections. Int J Pharm 559:102–112. https://doi.org/10.1016/j.ijpharm.2019.01.029
Nokhodchi A, Raja S, Patel P, Asare-Addo K (2012) The role of oral controlled release matrix tablets in drug delivery systems. Bioimpacts 2:175–187. https://doi.org/10.5681/bi.2012.027
Funding
This was a self-funded systematic review and meta-analysis and did not receive any specific grants/funding from any funding agency in any of the sectors.
Author information
Authors and Affiliations
Contributions
Dr. Jayapriya T: conceptualization and protocol development, methodology, data collection and extraction, bias assessment, meta-analysis, and manuscript writing. Dr. Vaishali Keluskar: conceptualization, methodology, data collection and extraction, bias assessment, manuscript—review, and editing. Dr. Vasanti Lagali-Jirge: supervision, validation, visualization, bias assessment, manuscript—review, and editing. Dr. Sridhar M: data curation, supervision, writing review, and editing.
Corresponding author
Ethics declarations
Ethics approval
This is a systematic review and meta-analysis that involves assessment of studies, and hence, ethical clearance was not sought for.
Consent to participate
This is a systematic review and meta-analysis does not involve any human or animal intervention, and hence, consent was not mandatory.
Consent for publication
The authors declare that they are willing to publish this article and data will be shared upon reasonable request.
Competing interests
The authors declare no competing interests.
Additional information
Other information
Registration and protocol: Protocol for this systematic review was prepared before the start of the review and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) maintained by the Centre of Reviews and Dissemination, University of York, York, UK (Ref No. CRD42022340445), which can be accessed through (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022340445). The current systematic review was written in concordance with the preferred reporting items for the systematic review and meta-analysis (PRISMA) 2020 statement.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jayapriya, T., Keluskar, V., Lagali-Jirge, V. et al. Efficacy of bioadhesives in the management of oral mucositis in patients undergoing radio-chemotherapy for treatment of head and neck cancer—a systematic review and meta-analysis. Support Care Cancer 31, 470 (2023). https://doi.org/10.1007/s00520-023-07920-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07920-2