Abstract
Purpose
Cyclophosphamide is a commonly used cancer agent that is metabolically activated by polymorphic enzymes. This study aims to investigate the association between predicted activity of candidate pharmacogenes with severe toxicity during cyclophosphamide treatment.
Methods
Genome-wide genetic data was collected from an institutional genetic data repository for CYP2B6, CYP3A4, CYP2C9, CYP2C19, GSTA1, GSTP1, ALDH1A1, ALDH3A1, ABCC1, ABCB1, and ERCC1. Treatment and toxicity data were retrospectively collected from the patient’s medical record. The a priori selected primary hypothesis was that patients who have CYP2B6 reduced metabolizer activity (poor or intermediate (PM/IM) vs. normal (NM) metabolizer) have lower risk of severe toxicity or cyclophosphamide treatment modification due to toxicity.
Results
In the primary analysis of 510 cyclophosphamide-treated patients with available genetic data, there was no difference in the odds of severe toxicity or treatment modification due to toxicity in CYP2B6 PM/IM vs. NM (odds ratio = 0.97, 95% Confidence Interval: 0.62–1.50, p = 0.88). In an exploratory, statistically uncorrected secondary analysis, carriers of the ALDH1A1 rs8187996 variant had a lower risk of the primary toxicity endpoint compared with wild-type homozygous patients (odds ratio = 0.31, 95% Confidence Interval: 0.09–0.78, p = 0.028). None of the other tested phenotypes or genotypes was associated with the primary or secondary endpoints in unadjusted analysis (all p > 0.05).
Conclusion
The finding that patients who carry ALDH1A1 rs8187996 may have a lower risk of cyclophosphamide toxicity than wild-type patients contradicts a prior finding for this variant and should be viewed with skepticism. We found weak evidence that any of these candidate pharmacogenetic predictors of cyclophosphamide toxicity may be useful to personalize cyclophosphamide dosing to optimize therapeutic outcomes in patients with cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cyclophosphamide is a chemotherapy agent used in patients with several tumor types including breast and ovarian cancer and lymphoma. Cyclophosphamide treatment is associated with common toxicities including febrile neutropenia and oral mucositis. As a prodrug, cyclophosphamide requires metabolic activation by CYP2B6, CYP3A4, CYP2C9, and CYP2C19 to several intermediate metabolites and its active metabolite, phosphoramide mustard. These intermediate and active metabolites also undergo detoxification by phase II enzymes including GSTP1, ALDH1A1, and ALDH3A1 [1, 2].
The field of pharmacogenetics has been particularly successful at finding clinically useful genetic biomarkers for prodrugs [3], such as clopidogrel and irinotecan. The enzymes involved in cyclophosphamide activation and detoxification have polymorphisms that are known to affect enzyme activity, and may affect systemic concentrations of the active metabolites and treatment-related outcomes. Indeed, several prior studies have reported associations for polymorphisms in the genes encoding these enzymes and in other pharmacogenes relevant to cyclophosphamide pharmacokinetics or DNA repair including ABCB1, ABCC1, and ERCC1.[4,5,6,7,8,9,10,11,12,13] In particular, polymorphisms in CYP2B6 have been reported to affect cyclophosphamide pharmacokinetics and toxicity risk across disease states [5, 6, 10, 12, 14,15,16,17].
Although potential genetic biomarkers of cyclophosphamide toxicity risk have been reported, none has been consistently replicated across studies. Additionally, prior studies have investigated individual polymorphisms without considering the combined effects of many polymorphisms on the overall metabolic activity phenotype (i.e., poor, intermediate, or normal metabolizer) of the enzymes of interest. The objective of this study was to investigate the independent and combined effects of polymorphisms in candidate genes, particularly CYP2B6, with the risk of severe cyclophosphamide toxicity in an independent cohort of cyclophosphamide-treated patients with cancer. Successful replication of the previously reported associations could warrant translational studies that personalize cyclophosphamide dosing to optimize therapeutic outcomes in patients with cancer receiving cyclophosphamide treatment.
Methods
Patients and toxicity data
This study was a retrospective pharmacogenetic study of patients with a diagnosis of cancer who were treated with cyclophosphamide as part of their chemotherapy regimen at Michigan Medicine from January 2011 through December 2020. All patients who received at least one cycle of cyclophosphamide for cancer treatment and had available genetic data were included in the study. The study protocol was approved by the Institutional Review Board (IRB#HUM 00161844).
Clinical data were retrospectively collected from the patients’ electronic medical records by an investigator who was blinded to genetic data. Collected clinical data included individual demographics, cancer type, tumor stage and grade, chemotherapy regimen including dose, frequency, and treatment duration, and prophylactic use of colony-stimulating factor (G-CSF or GM-CSF). Toxicity data were collected retrospectively from physician notes for all cyclophosphamide treatment cycles and graded by a blinded investigator based on the Common Terminology Criteria for Adverse Events version 5.0. Only toxicities believed to result from cyclophosphamide treatment, based on the known toxicities of cyclophosphamide, were included in the analysis. Treatment modification was defined by any change in the cyclophosphamide treatment including dose discontinuation, reduction, or delay that were attributed to toxicity based on the physician notes.
Genotype data
Genetic data were obtained from the Michigan Genomics Initiative (MGI) institutional genetic data repository, which conducts genome-wide genotyping and imputation, as previously described [18,19,20]. Briefly, germline DNA was genotyped on customized Illumina Infinium CoreExome-24 bead arrays and genotype calling was performed using Illumina GenomeStudio software. Standard quality control was conducted to remove samples with low call rate (< 99%), high contamination, or a kinship coefficient > 0.45 with another sample. Cleaned genotype data is used for imputation using the TOPMed reference panel via the TOPMed imputation server (https://imputation.biodatacatalyst.nhlbi.nih.gov/#!), filtering out poorly imputed variants (R2 < 0.3) [21]. Patients with no genetic data were excluded from the analysis.
All genotype calls were obtained for CYP2B6, CYP3A4, CYP2C9, CYP2C19, GSTA1, GSTP1, ALDH1A1, ALDH3A1, ABCC1, ABCB1, and ERCC1. These eleven enzymes and transporters were selected based on prior studies reporting associations with cyclophosphamide pharmacokinetics or toxicity [9,10,11, 13]. Genotype calls were translated into metabolic phenotypes (i.e., ultrarapid (UM), rapid (RM), normal (NM), intermediate (IM), or poor (PM) metabolizer) for each patient for CYP2B6, CYP3A4, CYP2C9, and CYP2C19 via an automated process. Briefly, “best-guess” single nucleotide polymorphisms and short insertion-deletions imputed in MGI were used as input for Stargazer v1.15 to generate star allele inferences [22] (Supplementary Table 1). Of note, MGI cannot detect CYP2B6 K262R, the variant necessary to differentiate CYP2B6*6 (K262R, Q172H) from other alleles that share the Q172H polymorphism. All patients who carry CYP2B6*6, CYP2B6*7, CYP2B6*9, or CYP2B6*37 are called CYP2B6*9, which is assigned to carriers of only Q172H. All of these are decreased function alleles and are handled similarly in CYP2B6 phenotype assignment systems, so this misclassification has no effect on phenotype assignment. Each patient’s diplotype was then translated into metabolic phenotypes consistent with Clinical Pharmacogenetics Implementation Consortium (CPIC) recommendations using the translation tables from PharmGKB, or PyPGx (v0.1.37, https://github.com/sbslee/pypgx) (Supplementary Table 2). Quality of genotype data was evaluated by comparing frequencies of inferred star alleles with frequencies observed in European individuals as reported by PharmGKB (Supplementary Table 3, note the higher frequency of CYP2B6*9 is due to the inclusion of CYP2B6*6 and other alleles that share Q172H). [23, 24] Patients were then classified into two groups for comparison, those with reduced enzyme activity (e.g., PM or IM) and others (e.g., NM, RM, and UM, depending on the enzyme). For the remaining genes, which do not have consensus systems for star nomenclature or phenotypic activity, patients were categorized for individual variants and using a gene-based composite of all variants. In either analysis, patients were categorized as variant carriers if they carried at least one variant and were compared with patients carrying only wild-type alleles. The following variant alleles were included in the analysis: GSTA1(rs3957357, rs3957356 [note, alleles were completely concordant]), GSTP1(rs1695), ALDH1A1(rs8187996, rs3764435, rs63319), ALDH3A1(rs2228100), ABCC1(rs903880, rs16967126, rs4148350), ABCB1(rs1128503, rs1045642), ERCC1(rs3212986, rs11615). Additional information for these alleles can be found in Supplementary Table 1 and comparison of allele frequencies with those seen in the 1000 Genomes Project European ancestry samples can be found in Supplementary Table 4 [25].
Statistical analysis
The primary endpoint was a composite of grade 3 + toxicity or treatment modification due to the toxicity at any time during cyclophosphamide treatment. Each of the endpoints that composed the composite primary endpoint was analyzed individually as secondary endpoints. The a priori defined primary hypothesis was that CYP2B6 PM/IM patients had a lower rate of grade 3 + toxicity or treatment modification due to toxicity compared with NM/RM. Secondary analyses were conducted for each of the genes with the primary and secondary endpoints without statistical correction for multiple comparisons. All statistical associations were tested using logistic regression analysis. Significant univariate associations were then adjusted for relevant clinical covariates including age (continuous), race according to the electronic medical record (white vs. other), sex (male vs. female), tumor type (breast cancer vs. other), chemotherapy regimen (AC (doxorubicin/cyclophosphamides) vs. other), starting cyclophosphamide dose (continuous), and prophylactic use of colony-stimulating factor (Yes v. No) in multivariable models. Analyses were conducted in R version 4.0.3.
Results
Patients and toxicity
Among the 846 patients who received cyclophosphamide between January 2011 and December 2020, 510 received cyclophosphamide for cancer treatment and had genetic data available and were included in this analysis (Fig. 1). The majority of patients were white (90%) with a median age of 52.9 years, 86% were women, and the most prevalent diagnosis was breast cancer (72%) (Table 1). The primary outcome of grade 3 + toxicity or treatment modification due to toxicity was recorded in 101 (20%) patients, including 72 (14%) with toxicity and 97 (19%) with treatment modification. Individual grade 3 + cyclophosphamide toxicities are reported in Table 1. All cyclophosphamide toxicities of any grade and the types of treatment modifications are reported in Supplementary Tables 5 and 6, respectively. The distribution of genetic categories used in the analysis is also reported in Table 1 and the numbers for each metabolic phenotype or polymorphism are reported in Supplementary Table 7.
Genetic association with clinical outcomes
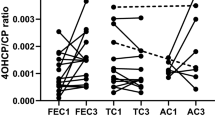
In the primary analysis, patients with CYP2B6 PM/IM phenotype did not have a lower odds of toxicity or treatment modification than NM (odds ratio (OR) = 0.97, 95% Confidence Interval (95% CI): 0.62–1.50, p = 0.88, Table 2, Fig. 2). Similarly, there was no difference in occurrence of either of the secondary toxicity endpoints (both p > 0.05).
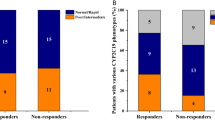
Each gene with sufficient genetic variability was included in secondary analyses. There were insufficient patients with CYP3A4 PM/IM phenotype or composite ALDH1A1 wild-type genotype to conduct these analyses (Supplementary Table 7). In a statistically uncorrected exploratory analysis, patients carrying ALDH1A1 rs8187996 had lower odds of grade 3 + toxicity or treatment modification due to toxicity (OR = 0.31, 95% CI: 0.09–0.78, p = 0.028, Fig. 3). This result maintained significance after adjustment for race, sex, cancer type, regimen, dose, and colony-stimulating factor use (adjusted OR (aOR) = 0.30, 95% CI: 0.09–0.77, p = 0.026). When separated by secondary endpoint, the association was only with grade 3 + toxicity (OR = 0.22, 95% CI: 0.44–0.74, p = 0.040, aOR = 0.19, 95% CI: 0.03–0.67, p = 0.028), and there was no difference in treatment modification due to toxicity (p = 0.20). Due to the low number of patients with homozygous variant genotype (n = 1), other genetic models (i.e., additive or dominant) could not be explored. None of the other tested phenotypes or genotypes was associated with the primary or secondary endpoints in unadjusted analysis (all p > 0.05).
Discussion
Cyclophosphamide is a prodrug metabolized by several enzymes to the toxic metabolite phosphoramide mustard to elicit its therapeutic effect. Polymorphisms in drug-metabolizing enzymes or drug transporters may affect pharmacokinetics of cyclophosphamide or its active metabolites, which could affect treatment efficacy or toxicity. We investigated the effect of polymorphisms in eleven pharmacogenes on cyclophosphamide treatment–related toxicity, with a particular focus on CYP2B6 based on prior evidence of the effect of CYP2B6 polymorphisms on cyclophosphamide pharmacokinetics and toxicity risk. [5, 6, 10, 12, 14,15,16,17] Our primary analyses found no evidence of a decrease in toxicity in patients with reduced CYP2B6 activity. In an exploratory, statistically uncorrected secondary analysis, carriers of the ALDH1A1 rs8187996 variant had lower odds of cyclophosphamide toxicity or treatment modification due to toxicity.
A prior pharmacogenetic analysis reported that patients with breast cancer who carried ALDH1A1 rs8187996 had higher hematological toxicity risk when receiving doxorubicin/cyclophosphamide (AC) [11]. This statistically uncorrected secondary analysis of the prospective SWOG 0221 clinical trial was the basis for inclusion of this polymorphism within our analysis. However, our results suggest that carriers of this variant have lower odds of cyclophosphamide toxicity, which is in the opposing direction and should not be considered replication. Aldehyde dehydrogenase (ALDH) enzymes, including ALDH1A1 and ALDH3A1, are responsible for inactivating the intermediate metabolite aldophosphamide to carboxyphosphamide [13]. In silico analyses indicate that ALDH1A1 variants could affect aldophosphamide metabolism [26]; however, clinical pharmacokinetics studies have not investigated the effect on aldophosphamide, carboxyphosphamide, or phosphoramide mustard concentrations to our knowledge and no effect has been detected on concentrations of the parent cyclophosphamide compound or the upstream metabolite 4-hydroxycyclophosphamide [13]. The discrepant findings from pharmacogenetic analyses with toxicity, combined with the lack of studies investigating an association with concentrations of active cyclophosphamide metabolite concentrations, suggest a potential false positive finding and do not support a clinically useful pharmacogenetic association, though further investigation is warranted, including determination of whether rs8187996 is functionally consequential or is merely tagging another functional causative variant.
CYP2B6, CYP2C9, CYP2C19, and CYP3A4 activate cyclophosphamide to 4-hydroxycyclophosphamide [27]. Several prior studies have reported that patients carrying reduced-activity polymorphisms in these drug-metabolizing enzymes have lower bioactivation of cyclophosphamide [5,6,7], leading to our hypothesis that patients with reduced metabolic activity would have lower risk of cyclophosphamide toxicity. Our study could not identify any effect of CYP2B6 metabolic phenotypes on cyclophosphamide-induced toxicity. A prior study from Tsuji et al. reported that carriers of the reduced-activity CYP2B6*6 allele had lower risk of severe neutropenia [10], which is consistent with the reduced cyclophosphamide activation in these patients [5, 12]. A direct attempt to replicate this finding is not possible in this study due to our inability to differentiate CYP2B6*6 (Q172H, K262R) from CYP2B6*9 (Q172H) and other alleles containing Q172H. Alternatively, Bray et al. reported that patients with breast cancer who carried CYP2B6*2 or CYP2B6*5 had higher risk of doxorubicin/cyclophosphamide dose delay, indicating higher toxicity risk [14]. PharmGKB classifies CYP2B6*2 and CYP2B6*5 as normal function alleles, so these associations are either false positives or there may be a specific effect of these variants on increasing cyclophosphamide metabolic activation [28]. Our inability to replicate these prior associations for CYP2B6 may also be due to differences in our endpoint, which included all cyclophosphamide toxicity, not just neutropenia or treatment delay, or differences in clinical practice such as prophylactic use of colony stimulating factor at our institution. However, retrospective pharmacogenetic analyses of large prospective clinical trials have also been unable to validate these associations [8]. This inconsistent replication suggests that this association, if it is real, can only be identified in certain patient cohorts, potentially based on their cyclophosphamide dose or the other components of their combination chemotherapy regimen. We were also unable to replicate other previously reported associations with cyclophosphamide toxicity for patients who carry variants in other non-CYP pharmacogenes including GSTP1, [8, 9] ERCC1, [10] ABCB1, [4] and ABCC1 [11].
Our results indicate that patients who inherit germline variants in ALDH1A1 may have lower risk of cyclophosphamide toxicity. Validation of this association in independent cohorts of cyclophosphamide-treated patients would warrant investigation into cyclophosphamide dose individualization to optimize therapeutic outcomes. Interestingly, ALDH1A1 overexpression has also been implicated in tumor resistance to cyclophosphamide treatment [29], indicating that germline ALDH1A1 variants may affect both toxicity and efficacy of cyclophosphamide treatment, and both would need to be considered when adjusting treatment [30]. Further work is needed to confirm the effect of ALDH1A1 polymorphisms on cyclophosphamide metabolism and treatment outcomes to warrant translational studies that can use this information to optimize clinical outcomes in cyclophosphamide-treated patients.
This study had several limitations that should be considered. First, retrospective collection of toxicity data may contribute to errors in classifying outcome events, particularly for toxicities that may be attributed to cyclophosphamide or other drugs used within combination chemotherapy regimens. Second, this study had a modest small sample size, which may have caused insufficient power to identify some true associations. Also, we may have missed some actual associations due to assuming dominant genetic effects for individual alleles and assuming that all variants in genes for which we created “composite gene variables” had similar directions of effect. Relatedly, although combining individual polymorphisms into a predicted activity phenotype is standard practice within pharmacogenetics, there may be substrate-specific allelic effects [28] that are not properly accounted for in genotype-to-phenotype translation systems or automated tools including Stargazer and PyPGx. Lastly, the putative association between ALDH1A1 rs8187996 and cyclophosphamide toxicity was identified in a statistically uncorrected exploratory secondary analysis and we could not demonstrate any plausible mechanism underlying this association due to the lack of pharmacokinetic data for these patients.
In conclusion, CYP2B6 metabolic phenotype was not associated with cyclophosphamide toxicity in this cohort. Patients who carry ALDH1A1 rs8187996 may have lower risk of cyclophosphamide-induced toxicity, though this association should be viewed skeptically given the discrepant direction of effect with a prior study and the lack of a clear mechanistic rationale for this association. Confirmation of this association in independent cohorts of cyclophosphamide-treated patients is necessary to justify translational studies evaluating the effect of genotype-guided cyclophosphamide dosing on treatment toxicity and efficacy, which may optimize therapeutic outcomes in patients with cancer.
Data availability
Data will be made available upon reasonable request to the corresponding author.
Code availability
Code will be made available upon reasonable request to the corresponding author.
References
Dirven HA, van Ommen B, van Bladeren PJ (1994) Involvement of human glutathione S-transferase isoenzymes in the conjugation of cyclophosphamide metabolites with glutathione. Cancer Res 54(23):6215–6220
Sládek NE (1999) Aldehyde dehydrogenase-mediated cellular relative insensitivity to the oxazaphosphorines. Curr Pharm Des 5(8):607–625
Begg EJ, Helsby NA, Jensen BP (2012) Pharmacogenetics of drug-metabolizing enzymes: the prodrug hypothesis. Pharmacogenomics 13(1):83–89. https://doi.org/10.2217/pgs.11.134;10.2217/pgs.11.134
Ikeda M, Tsuji D, Yamamoto K, Kim YI, Daimon T, Iwabe Y et al (2015) Relationship between ABCB1 gene polymorphisms and severe neutropenia in patients with breast cancer treated with doxorubicin/cyclophosphamide chemotherapy. Drug Metab Pharmacokinet 30(2):149–153. https://doi.org/10.1016/j.dmpk.2014.09.009
Helsby NA, Hui CY, Goldthorpe MA, Coller JK, Soh MC, Gow PJ et al (2010) The combined impact of CYP2C19 and CYP2B6 pharmacogenetics on cyclophosphamide bioactivation. Br J Clin Pharmacol 70(6):844–853. https://doi.org/10.1111/j.365-2125.010.03789.x
Helsby N, Yong M, Burns K, Findlay M, Porter D (2021) Cyclophosphamide bioactivation pharmacogenetics in breast cancer patients. Cancer Chemother Pharmacol 88(3):533–542. https://doi.org/10.1007/s00280-021-4307-0
Timm R, Kaiser R, Lotsch J, Heider U, Sezer O, Weisz K et al (2005) Association of cyclophosphamide pharmacokinetics to polymorphic cytochrome P450 2C19. Pharmacogenomics J 5(6):365–373
Yao S, Barlow WE, Albain KS, Choi JY, Zhao H, Livingston RB et al (2010) Gene polymorphisms in cyclophosphamide metabolism pathway, treatment-related toxicity, and disease-free survival in SWOG 8897 clinical trial for breast cancer. Clin Cancer Res 16(24):6169–6176. https://doi.org/10.1158/078-0432.CCR-10-281
Zhang BL, Sun T, Zhang BN, Zheng S, Lü N, Xu BH et al (2011) Polymorphisms of GSTP1 is associated with differences of chemotherapy response and toxicity in breast cancer. Chin Med J (Engl) 124(2):199–204
Tsuji D, Ikeda M, Yamamoto K, Nakamori H, Kim YI, Kawasaki Y et al (2016) Drug-related genetic polymorphisms affecting severe chemotherapy-induced neutropenia in breast cancer patients: a hospital-based observational study. Medicine (Baltimore) 95(44):e5151. https://doi.org/10.1097/MD.0000000000005151
Yao S, Sucheston LE, Zhao H, Barlow WE, Zirpoli G, Liu S et al (2014) Germline genetic variants in ABCB1, ABCC1 and ALDH1A1, and risk of hematological and gastrointestinal toxicities in a SWOG Phase III trial S0221 for breast cancer. Pharmacogenomics J 14(3):241–247. https://doi.org/10.1038/tpj.2013.32
Nakajima M, Komagata S, Fujiki Y, Kanada Y, Ebi H, Itoh K et al (2007) Genetic polymorphisms of CYP2B6 affect the pharmacokinetics/pharmacodynamics of cyclophosphamide in Japanese cancer patients. Pharmacogenet Genomics 17(6):431–445
Ekhart C, Doodeman VD, Rodenhuis S, Smits PH, Beijnen JH, Huitema AD (2008) Influence of polymorphisms of drug metabolizing enzymes (CYP2B6, CYP2C9, CYP2C19, CYP3A4, CYP3A5, GSTA1, GSTP1, ALDH1A1 and ALDH3A1) on the pharmacokinetics of cyclophosphamide and 4-hydroxycyclophosphamide. Pharmacogenet Genomics 18(6):515–523. https://doi.org/10.1097/FPC.0b013e3282fc9766
Bray J, Sludden J, Griffin MJ, Cole M, Verrill M, Jamieson D et al (2010) Influence of pharmacogenetics on response and toxicity in breast cancer patients treated with doxorubicin and cyclophosphamide. Br J Cancer 102(6):1003–1009
Shu W, Guan S, Yang X, Liang L, Li J, Chen Z et al (2016) Genetic markers in CYP2C19 and CYP2B6 for prediction of cyclophosphamide’s 4-hydroxylation, efficacy and side effects in Chinese patients with systemic lupus erythematosus. Br J Clin Pharmacol 81(2):327–340. https://doi.org/10.1111/bcp.12800
Veal GJ, Cole M, Chinnaswamy G, Sludden J, Jamieson D, Errington J et al (2016) Cyclophosphamide pharmacokinetics and pharmacogenetics in children with B-cell non-Hodgkin’s lymphoma. Eur J Cancer 55:56–64. https://doi.org/10.1016/j.ejca.2015.12.007
Rocha V, Porcher R, Fernandes JF, Filion A, Bittencourt H, Silva W, Jr., et al (2008) Association of drug metabolism gene polymorphisms with toxicities, graft-versus-host disease and survival after HLA-identical sibling hematopoietic stem cell transplantation for patients with leukemia. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK
Fritsche LG, Gruber SB, Wu Z, Schmidt EM, Zawistowski M, Moser SE et al (2018) Association of polygenic risk scores for multiple cancers in a phenome-wide study: results from the Michigan Genomics Initiative. Am J Hum Genet 102(6):1048–61. https://doi.org/10.1016/j.ajhg.2018.04.001
Shakeel F, Fang F, Kwon JW, Koo K, Pasternak AL, Henry NL et al (2021) Patients carrying DPYD variant alleles have increased risk of severe toxicity and related treatment modifications during fluoropyrimidine chemotherapy. Pharmacogenomics 22(3):145–155. https://doi.org/10.2217/pgs-020-0154
Zawistowski M, Fritsche LG, Pandit A, Vanderwerff B, Patil S, Schmidt EM et al (2021) The Michigan Genomics Initiative: a biobank linking genotypes and electronic clinical records in Michigan Medicine patients. medRxiv. https://doi.org/10.1101/2021.12.15.21267864
Taliun D, Harris DN, Kessler MD, Carlson J, Szpiech ZA, Torres R et al (2021) Sequencing of 53,831 diverse genomes from the NHLBI TOPMed Program. Nature 590(7845):290–299. https://doi.org/10.1038/s41586-021-03205-y
Lee SB, Wheeler MM, Patterson K, McGee S, Dalton R, Woodahl EL et al (2019) Stargazer: a software tool for calling star alleles from next-generation sequencing data using CYP2D6 as a model. Genet Med 21(2):361–372. https://doi.org/10.1038/s41436-018-0054-0
Klein TE, Chang JT, Cho MK, Easton KL, Fergerson R, Hewett M et al (2001) Integrating genotype and phenotype information: an overview of the PharmGKB project. Pharmacogenetics Research Network and Knowledge Base. Pharmacogenomics J 1(3):167–70. https://doi.org/10.1038/sj.tpj.6500035
Relling MV, Klein TE, Gammal RS, Whirl-Carrillo M, Hoffman JM, Caudle KE (2020) The clinical pharmacogenetics implementation consortium: 10 years later. Clin Pharmacol Ther 107(1):171–175. https://doi.org/10.1002/cpt.651
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al (2015) A global reference for human genetic variation. Nature 526(7571):68–74. https://doi.org/10.1038/nature15393
Verma H, Silakari O (2020) Investigating the role of Missense SNPs on ALDH 1A1 mediated pharmacokinetic resistance to cyclophosphamide. Comput Biol Med 125:103979. https://doi.org/10.1016/j.compbiomed.2020.103979
Roy P, Yu LJ, Crespi CL, Waxman DJ (1999) Development of a substrate-activity based approach to identify the major human liver P-450 catalysts of cyclophosphamide and ifosfamide activation based on cDNA-expressed activities and liver microsomal P-450 profiles. Drug Metab Dispos 27(6):655–666
Marcath LA, Pasternak AL, Hertz DL (2019) Challenges to assess substrate-dependent allelic effects in CYP450 enzymes and the potential clinical implications. Pharmacogenomics J 19(6):501–515. https://doi.org/10.1038/s41397-019-0105-1
Narendra G, Raju B, Verma H, Silakari O (2021) Identification of potential genes associated with ALDH1A1 overexpression and cyclophosphamide resistance in chronic myelogenous leukemia using network analysis. Med Oncol 38(10):123. https://doi.org/10.1007/s12032-021-01569-9
Hertz DL, Ramsey LB, Gopalakrishnan M, Leeder JS, Van Driest SL (2021) Analysis approaches to identify pharmacogenetic associations with pharmacodynamics. Clin Pharmacol Ther 110(3):589–94. https://doi.org/10.1002/cpt.2312
Acknowledgements
The authors acknowledge the Michigan Genomics Initiative participants, Precision Health at the University of Michigan, the University of Michigan Medical School Central Biorepository, and the University of Michigan Advanced Genomics Core for providing data and specimen storage, management, processing, and distribution services, and the Center for Statistical Genetics in the Department of Biostatistics at the School of Public Health for genotype data curation, imputation, and management in support of the research reported in this publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: Daniel Hertz and Faisal Shakeel; methodology: Mary Hwang, Brett Vanderwerff, Matt Zawistowski, Faisal Shakeel, Kelley Kidwell, and Daniel Hertz; formal analysis and investigation: Sarah Medley and Kelley Kidwell; writing—original draft preparation: Mary Hwang; writing—review and editing: Sarah Medley and Daniel Hertz; supervision: Daniel Hertz, Matt Zawistowski, and Kelley Kidwell.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study protocol was approved by the Institutional Review Board (IRB#HUM 00161844) at the University of Michigan.
Consent to participate
All patients agreed to participate in the Michigan Genomics Initiative, including permission to use their genetic and healthcare data for genetic analyses.
Consent for publication
No individual data or images are included in this publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
520_2022_7118_MOESM1_ESM.xlsx
Supplementary file1 (XLSX 28 KB) Supplementary Table 1: Alleles tested in each candidate gene. Supplementary Table 2: Metabolic phenotypes for each diplotype for each candidate gene. Supplementary Table 3: Allele frequency for each allele in the Michigan Genomics Initiative (MGI) cohort and reported in PharmGKB for each allele for each candidate gene. Supplementary Table 4: Allele frequency for each allele in the Michigan Genomics Initiative (MGI) cohort and reported in the 1,000 Genomes Project each allele for each candidate gene. Supplementary Table 5: Type and grade of each toxicity reported that was included in the analysis. Supplementary Table 6: Type of treatment alterations that were included in the analysis. Supplementary Table 7: Allele and phenotype frequencies for each candidate gene.
Rights and permissions
About this article
Cite this article
Hwang, M., Medley, S., Shakeel, F. et al. Lack of association of CYP2B6 pharmacogenetics with cyclophosphamide toxicity in patients with cancer. Support Care Cancer 30, 7355–7363 (2022). https://doi.org/10.1007/s00520-022-07118-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07118-y