Abstract
Purpose
Fertility preservation is an important issue for premenopausal cancer patients; however, not all patients receive counseling about chemotherapy-induced infertility and potential mitigation strategies. We aimed to identify characteristics of premenopausal breast cancer patients less likely to receive fertility counseling. We also investigated patient recall of chart-documented fertility discussions and patient attitudes toward fertility preservation.
Methods
The study was approved by our institution’s Institutional Review Board. All female patients with invasive primary breast cancer of any type, aged 40 or younger at the time of diagnosis, who were diagnosed during or up to 5 years prior to the study period were eligible. The study was conducted between February 2012 and October 2013. Enrolled patients completed an anonymous survey, and their medical charts were subsequently reviewed to identify provider documentation of fertility discussions, referral to fertility specialists, or implementation of fertility preservation. Patient comments regarding their fertility were solicited and examined thematically.
Results
Forty-nine patients consented to participate. Fertility discussions were documented by providers in 55 % of patients. Patients aged over 35 and multiparous patients were significantly less likely than their counterparts (p < 0.01 in both cases) to have had chart-documented fertility discussions. Only 52 % of patients with chart-documented discussions recalled having had such a conversation. Patient comments highlighted the difficulty of considering fertility at the time of diagnosis and also the risks and obstacles facing fertility preservation.
Conclusions
Despite increasing awareness, fertility is not universally discussed with premenopausal breast cancer patients at the time of diagnosis; older and multiparous patients are at particular risk of not receiving fertility counseling. Even when such discussions are documented, only about half of patients recall the conversation. Patient-reported barriers to fertility preservation include lack of education combined with the stress of diagnosis, financial costs, and perceived treatment toxicities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Therapeutic advances in recent decades have increased survival rates for breast cancer significantly, with 5-year survival rates improving from 75 % in the 1970s to 90 % in the present era [1, 2]. Women under the age of 40 comprise 5 % of all new diagnoses of invasive breast cancer annually, and the incidence of new cases in this population is rising in both the US and Europe [3, 4]. Treating cancer in patients of reproductive age raises a unique set of issues because of the potential of fertility compromise. Rates of chemotherapy-induced infertility range from 12 to over 90 % depending on age, chemotherapy regimen, and total dose [5–7]. There are 50 to 60 % of young breast cancer patients who desire children at the time of diagnosis, and studies have shown that premenopausal cancer patients may be willing to modify treatment regimens to lower their risk of infertility [8–10]. Several options exist for women interested in preserving their fertility, including embryo cryopreservation and administration of gonadotropin-releasing hormone agonists [11–13]. Timely referral to reproductive specialists, specifically before the receipt of chemotherapy, may enhance the success of fertility preservation, increase coping mechanisms, and decrease patients’ decisional conflict [14–16].
To facilitate these referrals, both the American Society of Clinical Oncology and the European Society for Medical Oncology have recommended that medical and surgical oncologists discuss infertility with all eligible patients at the time of diagnosis [17, 18]. Studies based on patient recall show variability in the frequency of these discussions, with rates ranging from 34 to 72 % [8, 9, 19–21]. One such study has demonstrated lower patient-reported rates of fertility discussions among patients with lower educational levels, age over 35, or previous children at the time of diagnosis [22]. However, studies using patient-reported outcomes are limited by the fact that patients may not process or recall fertility discussions during the stressful time of a cancer diagnosis [19, 23, 24]. In contrast, studies using documentation in patients’ medical charts are presumably less susceptible to recall bias. Previous studies have used medical records data to investigate referral patterns to fertility specialists [14, 25–27]; however, to our knowledge, no previous studies have used medical documentation to investigate rates of fertility discussions between patients and their oncologists.
Our goals with this study were threefold. We first sought to use medical records to investigate the rates of fertility discussions between young breast cancer patients and their outpatient medical providers. We additionally aimed to analyze the concordance rates between patient recall and chart documentation using a combination of patient-completed surveys and medical chart reviews. Lastly, we also aimed to investigate patient attitudes toward fertility consideration and fertility preservation modalities. We performed this single-site study at our multidisciplinary outpatient clinic, which specializes in breast pathology and is accredited by the American College of Surgery. Our breast cancer patients can be seen by medical oncologists, surgical oncologists, radiation oncologists, social workers, and other clinical professionals during the course of their treatment and follow-up; any of these professionals can place referrals to our reproductive endocrinology clinic, which is physically located on the same campus as our oncology clinic. Given these factors as well as the rising attention toward ‘oncofertility’ in the scientific community [28], we expected a high overall rate of chart documentation regarding fertility discussions. Because patient memories may be inaccurate during the stressful time of a cancer diagnosis [19, 23, 24], we expected low rates of concordance between patient recall and chart documentation.
Methods
The study was approved by our institution’s Institutional Review Board, and all study materials were available in both English and Spanish. Our study design consisted of an anonymous survey instrument to be distributed to eligible patients, followed by a systematic protocol for reviewing the medical charts of enrolled patients. Our survey instrument included demographic questions about age, cancer treatment information, parity, relationship status, and insurance information. Patients were also asked, “Did anyone explain to you how cancer treatment affects your ability to have children?” Additional space was provided at the conclusion of the survey instrument for patients to add comments about their experiences with fertility. All survey questions were optional, anonymous, and contained ‘unsure’ as a response option where appropriate. Expert advice from oncofertility and biostatistics specialists was used to design the survey. Although the survey instrument did not undergo pilot testing, all questions were independently reviewed (in both their English and Spanish formulations) for clarity and ease of understanding by nurses, medical students, and physicians not affiliated with our study.
All female patients with invasive primary breast cancer of any type who were aged 40 or younger at the time of initial diagnosis were eligible to enroll in our study. Inclusion criteria included a new diagnosis of breast cancer during our study period or up to 5 years prior to study initiation. Patients with in situ tumors were excluded. We attempted to enroll all such patients who were being seen for treatment appointments, follow-up appointments, or chemotherapy infusions at the single-site Breast Health Center of Women and Infants Hospital (Providence, Rhode Island, USA) between February 2012 and October 2013. Eligible patients were approached by the study authors before scheduled provider appointments or chemotherapy infusions. Patients who agreed to participate completed our survey instrument after providing informed consent. Consent forms were stored separately from completed survey instruments to maintain patient anonymity; patients’ individual medical providers were not asked to assist with patient enrollment and were not permitted to view study data.
After patient enrollment, a detailed chart review was performed of all entries in that patient’s chart authored by any healthcare provider (medical oncologist, gynecologist, breast surgeon, genetic counselor, social worker, or reproductive endocrinologist). Specifically, all chart entries between the time of referral to our center and the completion of at least one cycle of chemotherapy were reviewed. Our hospital system uses a fully integrated electronic medical record that enables a thorough review of chart entries and referrals without concern for missing records or illegible penmanship. Each chart entry was manually reviewed by one of the study authors (RB) in search of any mention of a discussion of the infertility risks of chemotherapy, acknowledgement of a patient’s fertility preferences or feasibility (e.g., prior tubal ligation), discussion regarding the possibility of consultation with a fertility specialist, actual referral to a fertility specialist, or any fertility preservation intervention (e.g., gonadotropin-releasing agonist administration). If any of the above criteria were met at least once, the patient was classified as having had a chart-documented fertility discussion. Tumor Board letters were not classified as fertility discussions because their contents reflected Board recommendations and not actual interactions with patients.
Once all data were compiled, results were analyzed in aggregate and with regard to age at diagnosis, multiparity, cancer stage, receptor status, ethnicity, partner status, insurance status, and educational level. Relative risks and two-tailed statistical tests were calculated to determine statistical significance using a predetermined alpha value of 0.05. Concordance rates regarding fertility discussions were compiled by comparing results from patient surveys to their chart review results. For patients with chart-documented fertility discussions, concordance rates were further analyzed with regard to each of the above eight characteristics and also with regard to the time interval between the patient’s diagnosis and her completion of the survey. For those patients who opted to leave comments regarding their experience with cancer treatment or fertility, their responses were compiled separately and analyzed in a post hoc fashion for demographic patterns and thematic elements.
Results
We identified 73 eligible patients and were able to approach 49 patients in person (67 % of the eligible population), all of whom consented to participate in our study. Patient characteristics are summarized in Table 1. The median age at diagnosis was 37, and the median parity was two children. The majority of patients (57 %) had stage II disease. Seventy-seven percent of the tumors were estrogen/progesterone-receptor positive while 18 % were triple-negative. Forty-nine percent of enrolled patients completed their surveys within a year of their initial breast cancer diagnosis. With regard to socioeconomic characteristics, most of our patients were white (65 %) and married or with a long-term partner (82 %). Seventy-one percent were privately insured, whereas 14 % were uninsured or unsure of their insurance status. Our population’s highest educational level was distributed between high school (24 %), some college (35 %), a four-year degree (20 %), and graduate studies (20 %).
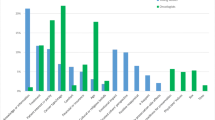
The results of our chart review are summarized in Table 2. Fertility discussions were documented in 27 patients or 55 % of our patient population. After these discussions, referrals to our reproductive endocrinology clinic were placed in 12 cases (24 % of the total population). Patients aged over 35 at the time of diagnosis were significantly less likely than patients 35 or younger to have chart-documented fertility discussions (36 versus 81 % discussion rates, relative risk 0.44, p < 0.01). Multiparous patients at the time of diagnosis were also significantly less likely than patients with 0 or 1 children to have chart-documented fertility discussions (31 versus 83 % discussion rates, relative risk 0.37, p < 0.01). Patients with any number of children had a lower rate of chart-documented fertility discussions compared to nulliparous patients (50 versus 69 % discussion rates, relative risk 0.72, p = 0.23); however, this difference was not statistically significant. Cancer stage, receptor status, ethnicity, partner status, insurance status, and educational status were not linked to statistically significant differences in fertility discussion rates.
We subsequently compared patient recall of fertility discussions to chart documentation of such discussions. Of the 27 patients with chart-documented discussions, 14 patients (52 %) recalled such a discussion, 8 (30 %) denied such a discussion, and 5 (18 %) were unsure. Of the 22 patients for whom no chart documentation of a fertility discussion was found, 4 patients (18 %) denied such a discussion, 13 (59 %) endorsed such a discussion, and 5 (23 %) were unsure. We performed a subset analysis of the 27 patients with chart-documented discussions, the results of which are summarized in Table 3. Of these 27 patients, those with cancers diagnosed fewer than 12 months before the time of their completion of the survey were significantly less likely to recall fertility conversations compared to those for whom this interval exceeded 12 months (35 versus 80 % recall rates, relative risk 0.44, p = 0.02). No significant differences in recall were found with stratification by age, parity, cancer stage, receptor status, ethnicity, partner status, insurance status, and educational status.
The comments provided by patients are transcribed in Table 4. Eleven patients (22 % of our enrolled population) opted to leave comments on their surveys; 6 of these 11 patients were multiparous while 5 of these 11 patients were aged over 35. Qualitative analysis of their comments revealed three overarching themes. Five patients endorsed contemplation of fertility issues but, in some cases, cited incomplete or distorted information regarding the feasibility of fertility preservation. Representative quotes include: “I am an educated woman, but I thought my diagnosis destroyed any hope of having a third child,” and “In the roller coaster of emotions I was going through at the time, I did not stop to think that I actually did have options.” For those patients who had pursued fertility preservation options, recognition of the risks and obstacles facing fertility preservation emerged as a second theme. Two patients mentioned the cost of embryo preservation, with one patient writing, “Until insurance companies categorize women undergoing treatment in the ‘infertile’ category, a lot of women will not be able to preserve embryos/eggs.” Another patient underwent complications from embryo freezing including ovarian hyperstimulation syndrome and wrote: “I’m still glad I did it, but would have liked to know and understand the complications better, as well as ways to prevent them prior to undergoing the treatment.” As a third and final theme, three patients who purposefully did not pursue fertility preservation left comments elaborating their reasoning; one patient cited disinterest in parenthood while two noted that they had previously underwent tubal ligation procedures.
Discussion
The importance of addressing fertility concerns with young cancer patients cannot be understated. Fifty to 60 % of young breast cancer patients may desire children at the time of diagnosis [8, 10], and even cancer patients who are initially ambivalent about fertility may desire children after treatment [29]. Discussing fertility issues with all young cancer patients at the time of diagnosis is paramount, as prompt referral to fertility specialists may both reduce decisional conflict and improve fertility preservation outcomes [14–16]. In our study, however, providers documented fertility discussions in only 55 % of cases. This figure is concordant with prior data based on patient recall [8, 9, 19–21] but is concerning given the close collaboration, shared interests, and physical proximity between the oncology and reproductive endocrinology departments at our institution. Older and multiparous patients were less likely to receive fertility counseling than their peers; this finding is consistent with prior surveys of oncologists showing that age and parity may factor into providers’ decisions about whether or not to discuss fertility with their patients [30–32]. However, the magnitude of this difference in our data is stark—women over age 35 or women with at least two children were less than half as likely as their study counterparts to have these discussions, a fact that underscores the potential for certain premenopausal cancer patients to receive subpar fertility counseling.
Even in the cases where providers did document fertility discussions with their patients, only one half of patients remembered the conversation while almost one third denied recollection of any such discussion at all. This finding, potentially due to cancer-related negative recall bias [23], highlights a limitation of patient-reported data in this setting. Interestingly, we found that correct recall of chart-documented discussions was significantly less likely in patients surveyed less than a year after being diagnosed compared to patients who had been diagnosed earlier. One study has found that breast cancer patients report worse depressive symptoms in the first year of treatment compared to later in their survivorship course [33]. Untreated depression can potentiate negative recall bias [23], which may have led to the lower recall rates seen in our study. Alternatively, given that premenopausal breast cancer patients suffer a decline in cerebral white-matter integrity during treatment, the “chemobrain” phenomenon may have contributed to this finding [34, 35]. In any case—given the benefits of early referral to fertility specialists [14–16]—our findings suggest that periodic reinforcement of fertility discussions in newly diagnosed patients may be beneficial because they may otherwise have difficulty recalling these conversations.
Patient perceptions of fertility preservation run the gamut from disinterest to regret to measured relief, as demonstrated by the comments left by patients in our study. For patients who are not interested in future parenthood (for example, patient status post tubal ligation), a detailed discussion of chemotherapy-induced infertility may be irrelevant. Nevertheless, identification of this patient subset is contingent upon knowing a patient’s fertility status and preferences—as such, it remains appropriate to discuss infertility as one of chemotherapy’s risks with all premenopausal patients. The consequences of neglecting this conversation are clear in the subset of patients who left comments about “the shock of my diagnosis” and the “roller coaster of emotions I was going through.” Earlier qualitative studies of young breast cancer patients have similarly highlighted how stressful a new cancer diagnosis can be [24, 36], underscoring the importance of an oncologist’s role in navigating women through discussions about their fertility preferences.
One theme that emerged in the comments of those women who had undergone fertility preservation was an acknowledgment of clinical and financial toxicities. Ovarian hyperstimulation syndrome and pulmonary emboli, as what happened to one patient in our study, are unfortunately potential complications of assisted reproductive technology [37]; women who undergo fertility preservation should understand the benefits and risks of different preservation options to allow them to make an informed decision. The patients who commented on monetary issues regarding fertility preservation highlight the ambiguities and inequities regarding insurance coverage for assisted reproductive technology in this setting. Part of the difficulty lies in the traditional definition of infertility, a sustained inability to conceive after 1 year of regular and unprotected intercourse, which does not apply to many young cancer patients at the time of diagnosis [38]. Treating fertility preservation as a standard component of cancer treatment or focusing on infertility as an iatrogenic treatment complication are two potential mitigation strategies, although regulations vary by insurance carrier and state and—as described by two of our patients—insurance coverage often falls short [38].
Limitations of this study include its small sample size, with 49 patients at a single institution. A larger multisite study could potentially detect fertility discussion patterns for which our study was underpowered; similarly, surveying women about their memory of fertility discussions at fixed points during and after treatment would have strengthened the validity of our findings regarding patient recall. We enrolled patients by approaching them in person during chemotherapy sessions and follow-up appointments; as such, the 33 % of our target population who were not enrolled tended to be patients who frequently missed or arrived late to scheduled appointments. To prevent introducing bias into our study design, we continued to attempt to approach these patients ourselves during appointments rather than asking their respective oncologists for assistance with study recruitment. We did not review the medical charts of patients who did not provide informed consent to enroll in our study, and so we are unable to comment on rates of fertility discussions in the subset of patients whom we could not enroll.
Our use of chart documentation as a surrogate variable for the presence of actual provider-patient fertility discussions has its own limitations. Specifically, 59 % of the patients for whom no chart documentation of fertility could be found stated that a discussion had taken place. While our data separately demonstrate that patient recall of fertility discussions can be inaccurate and while patients may have answered affirmatively to avoid portraying their oncologists in a negative light, this finding could alternatively be interpreted to suggest that chart reviews may not have captured all such fertility discussions. However, a more intensive approach such as the direct audio recording of provider-patient conversations would likely have influenced discussion rates through the Hawthorne effect. Furthermore, consensus guidelines call for documentation of fertility discussions with cancer patients; to quote a common adage, “if it wasn’t documented, it wasn’t done.” [18, 39].
In any case, better systemic solutions are needed to help practitioners understand and convey the fertility preservation options available to their patients. One 2012 survey of oncologists, for instance, revealed that only 18 % of oncology practices possess printed information about chemotherapy-induced infertility or hire healthcare professionals such as social workers to approach at-risk patients [40]. To help convey treatment information more comprehensively and durably for patients, personalized survivorship care plans that include information about treatment toxicities (including, in this case, premature ovarian failure) should be distributed to patients at the time of diagnosis and may become the standard of care for cancer patients in the near future [41]. Outside the clinic, patients should be made aware of relevant expert-reviewed patient-friendly websites including fertilehope.org (now part of livestrong.org) or myoncofertility.org [42, 43]. Online resources also include patient decision aids, which help patients to arrive at a decision about whether or not to pursue fertility preservation based on tumor characteristics, moral values, costs, and other variables [44]. From the standpoint of medical providers, implementing system-wide algorithms to automatically refer eligible patients for reproductive health assessments without prior referral is another promising solution [45].
In summary, our study adds to the existing pool of data that illustrate the low rates of fertility counseling surrounding the diagnosis of breast cancer. In particular, our data further demonstrate that older and multiparous women are more likely to ‘fall through the cracks’ with regard to fertility counseling. To our knowledge, this is the first study to compare patient recall rates to chart documentation regarding fertility preservation in breast cancer patients; the poor correlation between the two variables underscores the limitations of patient-recollection-based data for fertility research and highlights the importance of reinforcing fertility discussions with eligible patients. Increased awareness and outreach about treatment-induced infertility and potential fertility preservation options, whether directed at patients or at providers, will enhance the quality of the provider-patient relationship and will improve the quality of life of breast cancer survivors.
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A (2014) Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 64:252–271. doi:10.3322/caac.21235
Siegel R, Ma J, Zhou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64:9–29. doi:10.3322/caac.21208
DeSantis C, Ma J, Bryan L, Jemal A (2014) Breast cancer statistics, 2013. CA Cancer J Clin 64(1):52–62. doi:10.3322/caac.21203
Kasum M, Beketic-Oreskovic L, Peddi PF, Oreskovic S, Johnson RH (2014) Fertility after breast cancer treatment. Eur J Obstet Gynecol Reprod Biol 173:13–18. doi:10.1016/j.ejogrb.2013.11.009
Petrek JA, Naughton MJ, Case LD, Paskett ED, Naftalis EZ, Singletary SE, Sukumvanich P (2006) Incidence, time course, and determinants of menstrual bleeding after breast cancer treatment: a prospective study. J Clin Oncol 24(7):1045–1051. doi:10.1200/JCO.2005.03.3969
Partridge AH, Burstein HJ, Winer EP (2001) Side effects of chemotherapy and combined chemohormonal therapy in women with early-stage breast cancer. J Natl Cancer Inst Monogr 30:135–142
Christinat A, Pagani O (2012) Fertility after breast cancer. Maturitas 73(3):191–196. doi:10.1016/j.maturitas.2012.07.013
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP (2004) Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22(20):4174–4183. doi:10.1200/JCO.2004.01.159
Ruddy KJ, Gelber SI, Tamimi RM, Ginsburg ES, Schapira L, Come SE, Borges VF, Meyer ME, Partridge AH (2014) Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol 32(11):1151–1156. doi:10.1200/JCO.2013.52.8877
Senkus E, Gomez H, Dirix L, Jerusalem G, Murray E, Van Tienhoven G, Westenberg AH, Bottomley A, Rapion J, Bogaerts J, Di Leo A, Neskovic-Konstantinovic Z (2014) Attitudes of young patients with breast cancer toward fertility loss related to adjuvant systemic therapies. EORTC study 10002 BIG 3–98. Psychooncology 23(2):173–182. doi:10.1002/pon.3384
Matthews ML, Hurst BS, Marshburn PB, Usadi RS, Papadakis MA, Sarantou T (2012) Cancer, fertility preservation, and future pregnancy: a comprehensive review. Obstet Gynecol Int 2012:953937. doi:10.1155/2012/953937
Blumenfeld Z, Katz G, Evron A (2014) ‘An ounce of prevention is worth a pound of cure’: the case for and against GnRH-agonist for fertility preservation. Ann Oncol 25(9):1719–1728. doi:10.1093/annonc/mdu036
Tomasi-Cont N, Lambertini M, Hulsbosch S, Peccatori AF, Amant F (2014) Strategies for fertility preservation in young early breast cancer patients. Breast 23(5):503–510. doi:10.1016/j.breast.2014.05.024
Lee S, Ozkavukcu S, Heytens E, Moy F, Oktay K (2010) Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol 28(31):4683–4686. doi:10.1200/JCO.2010.30.5748
Treves R, Grynberg M, Parco S, Finet A, Poulain M, Fanchin R (2014) Female fertility preservation in cancer patients: an instrumental tool for the envisioning a postdisease life. Future Oncol 10(6):969–974. doi:10.2217/fon.13.265
Kim J, Mersereau JE (2014) Early referral makes the decision-making about fertility preservation easier: a pilot survey study of young female cancer survivors. Support Care Cancer. doi:10.1007/s00520-014-2526-3
Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, Pentheroudakis G, Group EGW (2013) Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl 6):vi160–170. doi:10.1093/annonc/mdt199
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K, American Society of Clinical O (2013) Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31(19):2500–2510. doi:10.1200/JCO.2013.49.2678
Duffy CM, Allen SM, Clark MA (2005) Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol 23(4):766–773. doi:10.1200/JCO.2005.01.134
Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T (2012) Patient satisfaction with physician discussions of treatment impact on fertility, menopause and sexual health among pre-menopausal women with cancer. J Cancer 3:217–225. doi:10.7150/jca.4408
Vadaparampil ST, Christie J, Quinn GP, Fleming P, Stowe C, Bower B, Pal T (2012) A pilot study to examine patient awareness and provider discussion of the impact of cancer treatment on fertility in a registry-based sample of African American women with breast cancer. Support Care Cancer 20(10):2559–2564. doi:10.1007/s00520-012-1380-4
Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, Rosen MP (2012) Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer 118(18):4579–4588. doi:10.1002/cncr.26649
Gorman JR, Malcarne VL, Roesch SC, Madlensky L, Pierce JP (2010) Depressive symptoms among young breast cancer survivors: the importance of reproductive concerns. Breast Cancer Res Treat 123(2):477–485. doi:10.1007/s10549-010-0768-4
Perz J, Ussher J, Gilbert E (2013) Loss, uncertainty, or acceptance: subjective experience of changes to fertility after breast cancer. Eur J Cancer Care 23(4):514–522. doi:10.1111/ecc.12165
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, Keefe DL, Albrecht TL (2009) Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol 27(35):5952–5957. doi:10.1200/JCO.2009.23.0250
Kim J, Oktay K, Gracia C, Lee S, Morse C, Mersereau JE (2012) Which patients pursue fertility preservation treatments? A multicenter analysis of the predictors of fertility preservation in women with breast cancer. Fertil Steril 97(3):671–676. doi:10.1016/j.fertnstert.2011.12.008
Bastings L, Baysal O, Beerendonk CCM, Braat DDM, Nelen WLDM (2014) Referral for fertility preservation counselling in female cancer patients. Hum Reprod 29(10):2228–2237. doi:10.1093/humrep/deu186
Lambertini M, Pinto AC, Del Mastro L (2014) Fertility issues in young breast cancer patients: what women want. J Thorac Dis 6(6):584–588. doi:10.3978/j.issn.2072-1439.2014.06.12
Armuand GM, Wettergren L, Rodriguez-Wallberg KA, Lampic C (2014) Desire for children, difficulties achieving a pregnancy, and infertility distress 3 to 7 years after cancer diagnosis. Support Care Cancer 22(10):2805–2812. doi:10.1007/s00520-014-2279-z
Forman EJ, Anders CK, Behera MA (2009) Pilot survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. J Reprod Med 54(4):203–207
King JW, Davies MC, Roche N, Abraham JM, Jones AL (2012) Fertility preservation in women undergoing treatment for breast cancer in the UK: a questionnaire study. Oncologist 17(7):910–916. doi:10.1634/theoncologist.2012-0064
Adams E, Hill E, Watson E (2013) Fertility preservation in cancer survivors: a national survey of oncologists’ current knowledge, practice and attitudes. Br J Cancer 108(8):1602–1615. doi:10.1038/bjc.2013.139
Ancoli-Israel S, Liu L, Rissling M, Natarajan L, Neikrug AB, Palmer BW, Mills PJ, Parker BA, Sadler GR, Maglione J (2014) Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer 22(9):2535–2545. doi:10.1007/s00520-014-2204-5
Deprez S, Amant F, Smeets A, Peeters R, Leemans A, Van Hecke W, Verhoeven JS, Christiaens MR, Vandenberghe J, Vandenbulcke M, Sunaert S (2012) Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. J Clin Oncol 30(3):274–281. doi:10.1200/JCO.2011.36.8571
Ganz PA (2012) Doctor, will the treatment you are recommending cause chemobrain? J Clin Oncol 30(3):229–231
Kirkman M, Winship I, Stern C, Neil S, Mann GB, Fisher JR (2014) Women’s reflections on fertility and motherhood after breast cancer and its treatment. Eur J Cancer Care 23(4):502–513. doi:10.1111/ecc.12163
Vloeberghs V, Peeraer K, Pexsters A, D’Hooghe T (2009) Ovarian hyperstimulation syndrome and complications of ART. Best Pract Res Clin Obstet Gynaecol 23(5):691–709. doi:10.1016/j.bpobgyn.2009.02.006
Campo-Engelstein L (2010) Consistency in insurance coverage for iatrogenic conditions resulting from cancer treatment including fertility preservation. J Clin Oncol 28(8):1284–1286
Day L (2009) What is documentation for? Am J Crit Care 18(1):77–80. doi:10.4037/ajcc2009419
Duffy C, Allen SM, Dube C, Dickersin K (2012) Oncologists’ confidence in knowledge of fertility issues for young women with cancer. J Cancer Educ 27(2):369–376. doi:10.1007/s13187-011-0304-1
Mayer DK, Nekhlyudov L, Snyder CF, Merrill JK, Wollins DS, Shulman LN (2014) American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. J Oncol Pract 10(6):345–351
Balthazar U, Deal AM, Fritz MA, Kondapalli LA, Kim JY, Mersereau JE (2012) The current fertility preservation consultation model: are we adequately informing cancer patients of their options? Hum Reprod 27(8):2413–2419. doi:10.1093/humrep/des188
Jona K, Gerber A (2010) MyOncofertility.org: a web-based patient education resource supporting decision making under severe emotional and cognitive overload. Cancer Treat Res 156:345–361. doi:10.1007/978-1-4419-6518-9_26
Garvelink MM, ter Kuile MM, Fischer MJ, Louwe LA, Hilders CG, Kroep JR, Stiggelbout AM (2013) Development of a decision aid about fertility preservation for women with breast cancer in The Netherlands. J Psychosom Obstet Gynaecol 34(4):170–178. doi:10.3109/0167482X.2013.851663
Patel A, Roston A, Uy A, Radeke E, Roston A, Keith L, Zaren HA (2015) Reproductive health and endocrine disruption in women with breast cancer: a pilot study. Support Care Cancer 23(2):411–418. doi:10.1007/s00520-014-2381-2
Acknowledgments
The authors wish to acknowledge Patricia Nolan, MD, MPH (Brown University School of Public Health, Providence, RI) for statistical assistance and for reviewing early drafts of this manuscript.
Conflict of interest
The authors have no conflicts of interest (financial or otherwise) to disclose. The authors have full control of all primary data and willingly grant the journal permission to review original data if requested.
Ethical approval
The study was approved by the Institutional Research Board of Women and Infants Hospital in Providence, RI.
Previous poster presentation
Banerjee R, Tsiapali E. “Predictors of Lack of Fertility Discussions with Breast Cancer Patients.” 15th Annual Meeting, American Society of Breast Surgeons (Las Vegas, NV). May 2, 2014.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Banerjee, R., Tsiapali, E. Occurrence and recall rates of fertility discussions with young breast cancer patients. Support Care Cancer 24, 163–171 (2016). https://doi.org/10.1007/s00520-015-2758-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2758-x