Abstract
Several organizations—including the American Society of Clinical Oncology (ASCO) and the American Society for Reproductive Medicine (ASRM)—have developed guidelines for physicians and cancer care centers so they may more effectively educate patients regarding cancer-related fertility impairment as well as available treatment options. Despite this, studies of both cancer patients and oncologists reveal an information gap where many patients are not being informed of potential impairment or what can be done. Moreover, there is a lack of understanding of how these discussions between patients and oncologists unfold, what information is discussed, and what factors shape these conversations. Our aim in this chapter is to describe our efforts to gain a nuanced understanding of how women of reproductive age with cancer learn about the potential threats to their fertility and available fertility preservation options. Drawing on interviews with women diagnosed with breast cancer prior to 40 years of age, we identify five trajectories of experience among the respondents in our sample. These trajectories differentiate across respondents by whether or not the topic was discussed with their oncologist, who initiated the topic (patient or oncologist), and whether or not fertility preservation treatment options were discussed. We also examine barriers/facilitators to the exchange of this information, including patient knowledge and empowerment and an oncologist’s network with fertility specialists. We suggest future research directions and considerations for best-practice guidelines, including greater examination of the networks between oncologists and fertility specialists, determinants of patient empowerment, and potential sources of inequality in the exchange of fertility-related information.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Cancer-related infertility has become an increasingly discussed topic in both the medical and cancer advocacy communities due to the growing awareness that some cancer treatments (e.g., radiation and chemotherapy) can impair future fertility—including treatments for nonreproductive cancers. Continuing advances in assisted reproductive technologies that may be applied to preserve the fertility potential of those afflicted with cancer have also helped to highlight the issue [1, 2]. Organizations including the American Society of Clinical Oncology (ASCO) [3] and the American Society for Reproductive Medicine (ASRM) [4] have developed guidelines to help oncologists and cancer centers integrate discussions of fertility impairment and fertility preservation treatment options early into the diagnosis and treatment process. Most experts agree that the most effective fertility preservation options (e.g., embryo freezing and sperm banking) are those that are made available to cancer patients before treatment begins. ASCO [3] suggests “Patients who are interested in fertility preservation should consider their options as soon as possible to maximize the likelihood of success.” (p. 2922). In the New England Journal of Medicine article by Jeruss and Woodruff [2], the authors contend that, “A discussion about the threat treatment poses to fertility is a critical part of the care of young patients with cancer, in order to allay concerns or offer options for preserving fertility.” (p. 905). ASRM [4] also affirms that, “Unless patients are informed or properly referred before treatment, options for later reproduction may be lost.” (p. 1623).
Yet despite these calls-to-action within the medical and advocacy communities, survey research has shown that many cancer patients, both pediatric and adult, do not recall having any discussion with a physician regarding potential fertility impairment or preservation options prior to treatment [1, 5–7]. In developing the ASCO guidelines [3], Lee et al. found that “recent surveys of male and female cancer survivors of reproductive age concur that at least half have no memory of a discussion of fertility at the time of their treatment disposition.” (p. 2926). Moreover, they concluded that, “Even when patients do recall infertility discussions, many are dissatisfied with the quality and amount of information provided.” (p. 2926). Surveys with physicians (most often oncologists) have similarly found that doctors do not always inform patients of fertility-preserving treatment options, even those that are fairly routine and effective, such as sperm banking [8]. Moreover, research conducted since 2006 has found that, “the majority of physicians are not following [the ASCO] guidelines.” (p. 338) [9].
While the information gap regarding fertility preservation is well recognized, we lack a nuanced understanding of what information is exchanged during patient–physician discussions, how these discussions evolve, and how patients experience this information exchange. We wanted to examine how discussions about treatment unfold between women of reproductive age with cancer and their oncologists, with the goals of improving best practice fertility preservation guidelines and shaping future research. We conducted interviews with women who had been diagnosed with breast cancer during their reproductive years. Although most research in this area has focused on whether or not a discussion regarding infertility has taken place, we found that the issue is more complicated than a “yes” or “no” answer. We identified five trajectories of experience among our respondents that describe not only if the topic of infertility was raised, but also the depth to which it was discussed. By looking at clinical discussions of fertility preservation from the perspective of women who have experienced a breast cancer diagnosis, we also identified key factors that facilitated or inhibited such discussions.
Study Design
We gathered data from interviews with 67 women who were diagnosed with breast cancer prior to 40 years of age (with 88.1 % being most recently diagnosed within the past 3 years and all diagnosed within the past 5 years; Table 1.1). Data collection took place between March 2008 and October 2009. The sample was recruited through advertisements placed in breast cancer advocacy organization newsletters (print and e-newsletters), email lists, and message boards aimed at cancer patients. We were initially concerned that the resulting sample would be much more politicized than the general population of younger women with breast cancer. To explore this possibility, we specifically asked women about their level of participation in breast cancer advocacy organizations and support groups. We found that only a few women in our sample could be classified as highly involved in such networks or groups. Since being involved in the cyber community (such as joining an email list from an advocacy group or occasionally checking a message board) involves minimal, if any, commitment, we do not think the sample over represents those who are very immersed in the breast cancer advocacy community. In some cases, the respondent had no involvement in any advocacy organization, and a friend or family member forwarded the recruitment advertisement onto them. The sample was characterized by high educational attainment and health insurance coverage, and included both married and single respondents as well as parents and nonparents (Table 1.1).
Interview Procedure
We conducted semi-structured phone interviews averaging 60 min in length; all respondents were read an IRB-approved statement of informed consent before agreeing to participate in the study. Interviewers were well versed on the topic of breast cancer as well as fertility preservation and all had completed IRB training. Interview topics included family background, diagnosis experiences, treatment concerns and decisions, and future family plans.
Data Analysis
We examined—from the patient’s perspective—the interactions between a patient and her oncologist regarding discussions of infertility and fertility preservation. While cancer patients can learn about treatments and make treatment decisions based on interactions with a wide range of healthcare workers and interested parties, including family members, our focus was on the relationship between a patient and her oncologist. Most of our respondents identified their oncologist as their main information source and most survey work and fertility-preservation guidelines have identified this clinical exchange as vital for patients to learn about fertility impairment and potential treatment options.
Information about cancer and fertility runs the gamut, from how soon after adjuvant treatment can one start trying to conceive to whether or not a future pregnancy will lead to a reoccurrence of breast cancer. Our analysis, however, focused on two distinct issues:
-
1.
The potential of breast cancer treatment to impair fertility.
-
2.
The availability of fertility preservation treatment options (both standard treatments such as embryo banking and investigational treatments such as ovarian cryopreservation).
We limit our focus to these two topics because it is the exchange of this information that is considered necessary for those facing cancer to make effective choices to safeguard their fertility prior to beginning cancer treatment.
Coding and Development of Five Trajectories
We took an inductive approach to data analysis—meaning that we did not start with set hypotheses of how these discussions evolve. Rather, our respondents’ narratives led to the identification of the five trajectories of experience we identified. The trajectories schema emerged through a three-stage coding process as described below (Fig. 1.1).
-
Stage 1: Was fertility impairment discussed?
We first determined if a conversation regarding potential fertility impairment took place prior to the patient starting potentially damaging cancer treatment. Respondents were asked if they discussed cancer-related infertility with their oncologist, and if so, when this discussion took place. “Fertility Discussed” indicates a discussion took place prior to treatment and “Fertility Not Discussed” indicates that no discussion took place prior to treatment. The latter group was categorized as Trajectory 1.
-
Stage 2: Who initiated the discussion?
During the coding for Stage 1, we found that, among those who had discussed cancer-related fertility issues, who brought up the topic differed. For some, the patient initiated the topic and, for others, their oncologist had. Since this point of comparison seemed to be a primary difference in the experience of discussing or learning about fertility preservation, we coded interviews as either “Oncologist-Initiated” or “Patient-Initiated.” During their interviews, respondents who had discussed fertility preservation with their oncologist were asked who brought up the topic. Respondents were also asked if they discussed the issue with any other healthcare workers, such as nurses, before starting cancer treatment. The vast majority did not. In a couple cases, the issue was brought up by another healthcare worker (e.g., a breast surgeon), which then prompted the patient to approach her oncologist. Respondents who initiated the conversation were categorized in Trajectories 4 or 5; those who indicated that their oncologist started the conversation were categorized in Trajectories 2 or 3.
-
Stage 3: Were fertility preservation options discussed?
Throughout the coding of Stages 1 and 2, it was evident that fertility preservation options were not routinely discussed even if fertility impairment was. Therefore, we further coded interviews where fertility was discussed into two categories—“Options Discussed” and “Options Not Discussed.” We defined fertility preservation treatment options as procedures performed prior to radiation and chemotherapy, where the goal is to preserve fertility functioning; procedures included standard options (e.g., oocyte/embryo freezing) as well as investigational options (e.g., ovarian cryopreservation; see [2] for further discussion.) “Options Discussed” included situations where respondents recalled their oncologist discussing some range of fertility-preserving options and/or referred the respondent to a fertility specialist prior to treatment to explore available procedures. “Options Not Discussed” included experiences where a respondent did not remember being told about any fertility-preserving options, was not sent to a fertility specialist prior to the start of her treatment, and/or was told not to worry about the issue until after her treatment was completed. Consistent with the description by Jeruss and Woodruff [2], even when respondents discussed options with their oncologist, rarely were they given the complete range of existing and investigational fertility preservation options and alternatives to biological parenthood such as adoption. Nonetheless, this distinction was meant to determine if respondents were told that cancer-related infertility was a potential roadblock to future family goals or that it was a situation that they could be proactive about prior to treatment.
Patient Trajectories
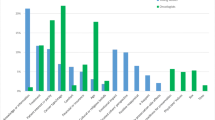
All of the respondents were assigned one of five distinct trajectories of experience (Fig. 1.1). While a small number of respondents (Trajectory 1–11.9 %) did not discuss the topic at all with their oncologists, most patients did (88.1 %). However, we found that for women who did discuss the topic with their oncologist, there was a range of experience in both the depth of information received and whether or not respondents felt that their concerns were adequately addressed. In 47.8 % of cases, oncologists brought up the subject and over half of this group did go on to discuss a range of potential options (Trajectory 3; 26.9 % of overall sample). Yet, even if an oncologist did bring up the topic of potential fertility impairment, a discussion of options was not guaranteed, with 20.9 % of the overall sample falling into Trajectory 2. Though most guidelines have focused on the importance of oncologists to broach the topic of fertility, our respondents frequently initiated this discussion (40.3 %). As with oncologist-initiated discussions, there was a range of ways in which the topic was discussed, from in-depth conversations regarding the options available (Trajectory 5–22.4 % of overall sample) to instances where an oncologist told a patient that she should not worry about fertility until after she was cancer free as in Trajectory 4 (17.9 % of overall sample).
Inhibiting and Facilitating Factors
We also examined patterns and common characteristics of how these conversations evolved or abruptly ended. Figure 1.2 identifies inhibiting and facilitating factors related to the patients, their oncologists, and their relationship that shaped the experiences of our respondents.
Oncologist Interest and Knowledge
Although this was a study of patients’ experiences, a fundamental question is whether or not oncologists feel responsible for raising the topic of fertility and have detailed knowledge about fertility preservation options. There were several cases in which respondents described very proactive oncologists who either took the lead in the conversation or were very open to discussing the matter further. But there were as many instances in which patients described that their physicians were not interested in the topic; in these cases, the oncologists made it clear that their main goal was battling the patient’s cancer first and foremost, or they offered information that was inaccurate/vague, or they simply responded that they did not know what would happen to fertility or where the patient could go for help.
Oncologists’ Networks with Fertility Specialists
One factor that influenced whether or not a fertility impairment discussion progressed to a discussion of fertility preservation treatment options was the presence of a network connecting oncologists with fertility specialists. This relationship was a primary way in which patients were able to learn about their fertility preservation options. In some cases, respondents felt their oncologists passed them off to a fertility specialist, while others reported a close collaboration between their physician and fertility specialists. These experiences stand in stark contrast to those who specifically asked their oncologists directly for a referral, but were told that their oncologist did not know any fertility specialists; unfortunately, this was a common occurrence among our respondents. For example, JoAnne (Trajectory 2), a 37-year-old married mother of one, was shocked when her oncologist informed her that chemotherapy could impact her fertility. She then recalled a discussion about the odds of her resuming menstruation after chemotherapy and a very cursory mention from her doctor that women sometimes freeze eggs. So while she was informed of the threat of potential fertility impairment, JoAnne felt there was no discussion of options beyond the vague comments from her doctor, and she did not receive guidance on where to go for further information:
It was very brief and really he said, ‘I’ve known there are women who have gotten eggs harvested. If you want to look into that, you need to go do it now.’ That was about the extent of the entire conversation about that. And then I really felt kind of on my own. I said, ‘Great, do you know any?’ And his answer was really no. I mean that kind of—we felt kind of left off on our own of how to figure that out.
When the fertility specialist/oncologist link was lacking, patients had to be proactive to find a fertility specialist to consult. Several respondents were successful and received the desired information; however, JoAnne’s Internet research led her to believe that the only option was oocyte harvesting and that it would delay her treatment. Without much guidance, she and her husband decided just to “deal with the cards we were dealt” and hope her fertility would be unharmed. Those who recalled oncologists giving them referrals had a much easier time finding out desired information and were able to weigh their options more effectively. In fact, an important point of departure among those whose oncologist brought up the topic (Trajectories 2 and 3) and whether or not they discussed options was this existing link or relationship between their oncologist and a fertility specialist. Clearly, if an oncologist brought up fertility, they had at least some rudimentary knowledge of the issue and at least some sense of responsibility to discuss the issue (through self-initiative or in order to follow guidelines at their healthcare institution). Divergence in the progression of the discussion often came from whether or not the oncologist was able to offer a referral to a fertility specialist.
Patient Receptiveness
How receptive a patient is to fertility-related information is also an important factor that influences the progression of discussions with their oncologist. Women in this study varied in what their future family plans were and whether or not they wanted to have biological children. Of those patients whose doctors raised the subject of fertility but no options were relayed (Trajectory 2), several women said they were not interested in having future children or becoming first-time parents. These respondents were comfortable with their decision not to pursue the topic further, but they thought that it was information that women facing cancer should hear.
Patient Knowledge and Empowerment
A patient having some sense that infertility matters can change the discussion of fertility preservation, particularly if her oncologist does not bring up the topic. In our study, sometimes this knowledge was obtained through the patient’s occupation (such as being a physician themselves), occasionally it came from knowing someone else who had breast cancer, and sometimes it was just a gut instinct at the time of diagnosis. How much someone knows prior to being diagnosed with cancer matters as well. Respondents who were physicians and those in other health-related occupations knew (or heavily suspected) not only that their fertility may be at risk but also what follow-up questions to ask.
What is puzzling is why some women who had a feeling that fertility might have been an issue did not pursue the topic or did not push the topic further if they had unanswered questions. The level of self-efficacy that respondents described in their relationship with their oncologist shaped how empowered they felt to push the topic of infertility further. For example, Janet (Trajectory 4), a 32-year-old community college student and married mother of one child, had asked her oncologist about fertility issues prior to beginning treatment but described her concerns as being “dismissed” by her oncologist and that she was not offered any fertility preservation options. When asked about her role in her overall treatment, Janet presented herself as having a passive role, saying “I really had no choice.” Though she described not being happy with her oncologist overall, when we asked why she did not change doctors she replied, “He seemed to know what he was doing so I just stayed.”
Janet’s experience represents those of many respondents in Trajectories 1, 2, and 4. The women in these categories more often described themselves as following doctor’s orders in all aspects of their cancer care, even if they were not getting the information or treatment they desired. Other respondents, particularly those in Trajectory 5, described themselves as being proactive to the point of being pushy, at times even fighting what they perceived to be the ambivalence of their physicians and advocating in general to ensure they received the best treatment available. When Fiona (Trajectory 5), a 31-year-old single grant writer with no children, was diagnosed, she quickly suspected that radiation and chemotherapy could harm her future fertility. Fiona’s energies quickly turned to her fertility, “then almost my primary focus was fertility. Without a doubt. I was willing to forgo chemotherapy if it meant that I couldn’t have kids.” Fiona broached the topic of fertility and she felt her oncologist was less than enthusiastic about discussing the issue further:
Then, after doing a bit of research on the Internet, and I asked my oncologist directly about it. I had to bring it up … [My oncologist] reacted as if—I got the feeling that she didn’t want me thinking about that. I got the feeling that her focus was to keep me alive. And I got the feeling like maybe if I hadn’t brought it up, I’m not sure she would have mentioned it to me. But honestly knowing her, I think she would have told me because just to cover herself. But it wasn’t one of the first things—she wasn’t as concerned about it as I was, of course.
Despite this initial resistance, Fiona took charge by continuing to ask questions and she was able to set up consultations between her oncologist and a fertility specialist she found online. Fiona’s outcome was largely shaped by her own self-described pushiness and self-efficacy. Our point here is not to blame respondents for not learning about fertility impairment or options, but to point out that patients’ quality of knowledge concerning potential fertility impairment prior to diagnosis and the level of self-efficacy, or empowerment, they feel when interacting with their oncologist were key factors in the outcomes for our respondents.
Status Differences Between Patient and Physicians
So what shapes empowerment? One potential answer suggested by our data is the nature of the relationship between patient and doctor in terms of status similarity/difference. There are varying perspectives on what empowerment entails, see [10]. We use the definition of Linhorst et al. [11]: “having decision-making power, a range of options from which to choose and access to information.” (p. 427). Respondents who felt less empowered to pursue the topic of infertility were also those respondents for whom there was potentially the greatest social status difference between patient and physician in terms of occupation/education level and race/ethnicity. The empowered group that included Fiona (Trajectory 5) also included two physicians, a physician’s assistant, and a professor, whereas groups that described far less self-efficacy (Trajectories 1, 2, and 4) had occupations outside of healthcare as well as lower educational attainment. In Trajectories 3 and 5, where respondents described far higher levels of self-efficacy, fewer than 6 % of women did not have at least a Bachelor’s degree compared to over 21–25 % of respondents in Trajectories 1, 2, and 4. Occupation and education not only determine what a patient knows about the potential for fertility impairment, but also shape the relationship between patient and physician and influence the patient’s level of comfort with bringing up topics or even challenging their physician. Some research supports the idea that the likelihood of an oncologist discussing fertility preservation may be related to perceived status similarities between themselves and their patient. Rieker et al. [12] suggest that oncologists may be more likely to discuss the issue of sperm banking with patients who they believe to have a similar status (e.g., highly educated patients). Situations where there is a greater perceived social distance between patient and oncologist may impede fertility-related conversations.
Moreover, cultural background differences could exacerbate feelings of status differences. As shown in Fig. 1.2, Trajectories 1, 2, and 4 included most of the women in this study who were non-Caucasian and most of these women described their oncologists as being Caucasian. Differences in race and ethnicity could further inhibit self-efficacy on part of the patient or serve as barrier to the oncologist broaching the topic. This latter assertion is supported by Quinn et al. [9], who found that oncologists felt cultural and language differences with patients were barriers to the discussion of fertility preservation.
Research of oncologists’ behavior found that some are reluctant to bring up fertility preservation because of concerns about a patient’s ability to afford these procedures [8, 9]. While concerns over costs may not indicate issues related to social status differences, it does raise the possibility that how oncologists perceive patients and their class or socioeconomic position may influence whether or not the topic of fertility preservation gets discussed.
What Doesn’t Matter?
Within our sample, age of the patient did not seem to influence who was told what. We had thought that younger women would be given more options, either because they had no children yet or because of a general assessment that their fertility may be better to begin with. However, many younger patients were told to “just wait and see” what happens to their fertility posttreatment. Similarly, patients did not feel that oncologists withheld (or offered) information based on their partnership or parental status.
Also, the quality of the relationship between patient and physician from the patient’s perspective did not matter. Many who did not discuss fertility-related issues/options still described their overall relationship with their physician as good, even if they felt they would have made different choices had they been given more information. Conversely, oncologists who were described by their patients as motivated on the topic of infertility did not predict a good relationship overall.
Shaping Future Research and Guidelines
Our sample was disproportionately insured and highly educated, with many having professional occupations. Addressing a more diverse sample could reveal a greater number of trajectories of experience, including family-initiated discussions for groups where having children is seen as a community responsibility. Also, by focusing on a relatively privileged range of respondents, our findings may actually underestimate the lack of information received by the general population of younger women facing breast cancer. Among women who would seem to have the most access to personalized care, information, and financial resources for elective fertility-preservation procedures (which are not routinely covered by health insurance), many were not told that their fertility could be compromised nor were they given treatment options. It is likely that those lacking economic resources would have even less access to fertility-related information and options. Our study also focuses on women exclusively. Since men and women (as well as different cancer types) have different fertility risks, treatment options, and success rates for fertility preservation, a more in-depth look at the barriers and facilitators specific to men’s discussions of fertility with their oncologists as well as studies that include women with other types of cancer are needed. Nevertheless, the preliminary findings we describe here and the suggestions below will help guide future research regarding patient–oncologist communication on the topic of fertility preservation.
Moreover, our aim is not to conclude what percentage of female cancer patients experience a particular outcome versus another, but to understand what matters in how these discussions evolve, at what points the exchange of information breaks down, and where interventions could help facilitate more comprehensive conversations between patient and physician. Based on our respondents’ experiences, we suggest the following future research directions and considerations for the development of clinical guidelines:
Understanding the oncologist’s Role in Fertility Preservation
It is important that we further investigate what oncologists know about fertility issues, as well as available fertility preservation options. Several respondents were not confident about their oncologist’s knowledge regarding fertility impairment. Some even reported being given responses that were unclear at best and simply wrong and misleading at worst. Although relying on patients’ perspectives, there does seem to be the assumption in many discussions of fertility preservation that oncologists are well versed on the issue. However, Schover et al. [8] in a survey of 718 oncologists found that with regard to sperm banking, oncologists’ knowledge is largely “not up to date” (p. 1895). While the authors failed to find a significant correlation between knowledge and “how often they mentioned sperm banking to eligible patients” (p. 1892) [8], in a study of 16 oncologists, Quinn et al. [13] found that oncologists are not always well informed about fertility preservation and this influenced whether or not they felt comfortable with the topic and ultimately discussed the issue with patients (also see [9]). Quinn et al. [13] also reported that the physicians in their sample “were unaware of any guidelines, either for their specialty or for the institution regarding [fertility preservation]” (p. 152) and most had not received formal training on the issue (p. 152).
Moreover, studies of oncologists have found that patient characteristics such as the gender or marital status of a patient [8, 13], a patient’s prognosis [8, 9, 13], and other considerations such as the time available to meet with patients [8, 13], influenced the degree to which oncologists addressed fertility, if at all. Future research should also focus on oncologists and cancer centers who do integrate informed fertility preservation discussions into their care routines, to understand how they learn about and stay current on the topic, and how they implement best-practice guidelines and develop effective strategies for counseling patients on fertility preservation.
Examining the Role of Fertility Specialists
Access to fertility specialists was clearly an influential factor in how fertility discussions progressed for our responders. Several guidelines, including from ASRM and ASCO, discuss the importance of networks between oncologists and fertility specialists and how to encourage discussions across these specialties. However, Quinn et al. [14] found that less than half of physicians routinely refer patients of childbearing age to reproductive endocrinologists. Moreover, Schover et al. [8] found that the most cited barrier among the oncologists they surveyed for not referring men to sperm banking was “a hard time finding convenient banking facilities” (p. 1895). Our research also identified the relationship between fertility specialists and oncologists as critical for patients to receive desired information. It is imperative that future research explores when and how these networks emerge and when are they the most effective for patients. Moreover, future research should look to fertility specialists as subjects of interest. What do they know regarding cancer-related infertility? Are fertility specialists aware of investigational procedures such as ovarian cryopreservation?
What Factors Allow Patients to Raise Concerns?
Our respondents’ feelings of self-efficacy were often the determining factor in whether they obtained information on fertility. Future research should investigate factors within the patient–physician relationship that allow patients to share their concerns. Is it when patients feel more “comfortable” with their physician? Is it when the conversation of fertility is not touched upon in a laundry list of potential side effects? How does the presentation of fertility-related information (e.g., educational brochures versus physician talking points) influence whether or not a patient feels they can ask follow-up questions?
Empowerment Through Information
Women who did not discuss fertility or fertility preservation options with their oncologist often used the word “dismissed” to describe their experiences and concerns. It is impossible from our data to know how physicians assessed their individual cases and what potential options would have been available (if any). However, it is clear that all but one respondent who did not discuss the topic at all eventually learned about fertility impairment and treatment options after the fact, with most becoming upset that they were not more fully informed before starting treatment. Clinical guidelines could be explicit in that if standard fertility preservation options are not advised for a particular patient, physicians should offer some amount of explanation as to why. If women find out after the fact, their reactions to this unsettling information could affect their quality of life post-cancer. Having information—even if the answer is that standard options are not advised—is more empowering to patients than simply being kept in the dark. This conversation could also open the discussion to include other parenting options (e.g., surrogacy, adoption) as outlined by Jeruss and Woodruff [2].
Understanding Social Inequality and Barriers to Information
The most distressing part of our study was that some groups were less likely to receive fertility-related information, even when they directly asked about infertility. Fertility-preservation options prior to treatment (e.g., IVF) and posttreatment (e.g., adoption) can be costly, and economic and social resources will play a key role in determining which groups are able to become parents post-cancer. Here, we reveal that this potential inequality can be traced back to the initial patient–physician interaction, where inequality in access to vital information was tied to educational attainment, occupation, and even racial/ethnic background for many of our respondents. In their survey, Schover et al. [8] found that oncologists reported that they would be less likely to refer men for sperm banking who were HIV+ or openly homosexual (pp. 1894–5). Best-practice guidelines and researchers must address more openly how specific subsets of patients have been overlooked or may require more specialized educational techniques. For example, some racial/ethnic groups may be less likely to pursue a topic not initiated by their physician because of cultural and community differences in how to interact with experts and institutional agents such as physicians.
In this study, there was a clear distinction between those able to make a decision, even if that decision was to not pursue fertility preservation, and those who felt they were not allowed to make a choice. Clinical guidelines should not recommend that all patients have a biological child, but must ensure that cancer patients are informed about infertility as a potential side effect of cancer treatment and that patients are able to have an open dialogue with their healthcare team about possible fertility preservation options. Receiving information, feeling involved in medical decision making, and communicating openly with their physician shapes patient empowerment. A great deal of research has shown that patient empowerment can lead to “improvements in health status, increased satisfaction, and self-efficacy” ([10], p. 25) as well as better health and emotional outcomes, even for patients with potentially life-threatening illnesses like breast cancer [15, 16]. If a patient is unable or chooses not to take steps to preserve their future fertility, the feeling of being fully informed and capable of weighing options, and that their concerns are addressed would benefit cancer patients.
References
Snyder KA, Pearse W. Discussing fertility preservation options with patients with cancer. JAMA. 2011;306:202–3.
Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902–11.
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K. American society of clinical oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–31.
Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005;83:1622–8.
Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 2005;23:766–73.
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–83.
Thewes B, Meiser B, Taylor A, Phillips KA, Pendlebury S, Capp A, Dalley D, Goldstein D, Baber R, Friedlander ML. Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol. 2005;23:5155–65.
Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol. 2002;20:1880–9.
Quinn GP, Vadaparampil ST, King L, Miree CA, Wilson C, Raj O, Watson J, Lopez A, Albrecht TL. Impact of physicians’ personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009;77:338–43.
Bridges JFP, Loukanova S, Carrera P. Patient empowerment in health care. In: Heggenhougen K, Quah S, editors. International encyclopedia of public health, vol. 5. San Diego, CA: Academic; 2008. p. 17–28.
Linhorst DM, Hamilton G, Young E, Eckert A. Opportunities and barriers to empowering people with severe mental illness through participation in treatment planning. Soc Work. 2002;47:425–34.
Rieker PP, Fitzgerald EM, Kalish LA. Adaptive behavioral responses to potential infertility among survivors of testis cancer. J Clin Oncol. 1990;8:347–55.
Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, Wilson C, Munster P. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1:146–55.
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, Keefe DL, Albrecht TL. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–7.
Deadman JM, Leinster SJ, Owens RG, Dewey ME, Slade PD. Taking responsibility for cancer treatment. Soc Sci Med. 2001;53:669–77.
Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, Lakhani I, Salem B, Katz SJ. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Serv Res. 2005;40:745–67.
Acknowledgement
This work was supported by the Oncofertility Consortium NIH 5UL1DE019587 and RL1HD058296.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Snyder, K.A., Pearse, W. (2014). How Do Cancer Patients Learn About Fertility Preservation? Five Trajectories of Experience. In: Woodruff, T., Clayman, M., Waimey, K. (eds) Oncofertility Communication. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8235-2_1
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8235-2_1
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8234-5
Online ISBN: 978-1-4614-8235-2
eBook Packages: MedicineMedicine (R0)