Abstract
Purpose
The aim of this study was to explore associations between arthralgia and fear of recurrence in breast cancer patients treated by aromatase inhibitors (AI).
Method
We sent a set of questionnaires to 100 patients examining their pain characteristics, anxiety (STAI), depression (BDI-SF), quality of life (SF-36), fear of recurrence (FCRI), and representations of AI treatment (ad hoc questionnaire). Nonparametric tests were used to investigate between-group comparisons (arthralgia vs. nonarthralgia) in these domains as well as the associations between arthralgia and fear of recurrence.
Results
Of the 77 patients who returned the questionnaires (response rate = 77 %), 60 (78 %) reported arthralgia. The mean score of fear of recurrence exceeded the pathological threshold in the arthralgia group and was significantly higher than that in the nonarthralgia group (14.8 vs. 10.7, p < 0.01). Significant associations were observed between fear of recurrence and pain intensity (r = 0.274, p < 0.05) and pain relief (r = −0.409, p < 0.05). More than 80 % of the total sample declared that they were well informed about the aim of AI, their side effects, and the risk of developing arthralgia. Fear of recurrence did not appear to be associated with representations of AI.
Conclusion
The study revealed a close relationship between pain intensity and fear of recurrence. In particular, it showed that effective pain management was accompanied by a reduced fear of recurrence. Information, although essential, appeared insufficient to overcome patients' concerns about pain. Therefore, the implement of a systematic screening for arthralgia and the improvement of analgesic treatment are essential issues. New strategies for pharmacological and nonpharmacological treatment must be developed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of hormone therapy among women presenting tumors with positive hormone receptors (75 % of breast cancers) substantially reduced the risk of recurrence and increased survival rates without recurrence among these patients. Aromatase inhibitors (AI) (letrozole, anastrozole, and exemestane) have proved to be better at preventing recurrence than tamoxifen and are currently prescribed as the first line of treatment for menopausal women with a hormone-dependent breast cancer [1]. AI also have a different toxicity profile than tamoxifen [2], in particular joint and muscle pain are more frequent [3, 4].
Randomized tests of the effectiveness of AI thus report a prevalence of arthralgia varying between 5 and 35 % [5–8], with the women’s quality of life being globally satisfactory and without any real sign of psychological distress [9–13]. Nevertheless, the data derived from observational clinical studies contrast with these results by showing that arthralgia is more frequent (approximately one woman out of two) [14–19] and can significantly reduce the quality of life of women treated with AI [15]. Furthermore, the treatment of arthralgia is complex due to the absence of validated standards for professionals and the ongoing issue related to the physiological mechanisms involved [4].
It is known that among women treated for breast cancer, the persistence of pain after treatment is a risk factor for emotional distress and even depression [20, 21]. Pain is also associated with a fear of recurrence (FoR) which is the greatest and most frequent concern experienced by patients in remission of their breast cancer [22–24]. A young age, impairment of quality of life, and emotional distress are also factors that are predictive of FoR, which can persist for several years [25]. The theoretical models of FoR emphasize the central role of the patient’s cognitions [26, 27]. The importance of the representations associated with cancer and its treatments (in particular, the perceived necessity, side effects, and effectiveness) has also been highlighted by Corter et al. in explaining the variations in the intensity of FoR [28]. This study compared two groups of patients treated with AI (according to FoR) and showed that the interpretation of certain physical symptoms as being cancer-related appeared to be a factor of increased FoR.
Based on these data, we hypothesize that among patients treated with AI, the interpretation of arthralgia as a cancer-related symptom could increase FoR and consequently increase emotional distress.
The first aim of our study was therefore to determine the frequency of arthralgia among the population of women in remission for a breast cancer and receiving AI treatment and its effect on the quality of life and emotional state of these patients. Our second aim was to identify the links between the presence of arthralgia and FoR, in particular by determining whether the intensity of pain, the presence of pain medication, the degree of relief from pain, the interpretation of arthralgia as a side effect of AI treatment, and the understanding of the purpose of the treatment (to prevent recurrence) were associated with the intensity of FoR.
Patients and methods
Study population and design
ARTHRO-PSY was a cross-sectional descriptive and quantitative study promoted by the Supportive Care Department at Gustave Roussy Cancer Center (France). ARTHRO-PSY was conducted with the approval of the scientific committee of Gustave Roussy. Eligible patients were identified among those attending scheduled visits at the breast cancer unit from April to June 2010 on the basis of the following criteria: receiving treatment for a localized hormone-dependent cancer with an aromatase inhibitor for at least 1 year, aged 18–75 years. Exclusion criteria were as follows: aged more than 75 years (because joint pain risk factors increase with age), medical history involving chronic illnesses that can cause joint pain or affect physical ability or mental diseases (schizophrenia, bipolar disorder, recurrent depression). Eligible patients were then contacted by phone by a psychiatrist in order to present the study and to ask them if they would be interested in participating. An information letter, an informed consent form, a set of questionnaires, and a stamped-addressed envelope were sent to the patients who agreed to participate. Patients who did not return their questionnaires within 1 month were contacted again by phone.
Measurements
Medical data were mainly obtained from the patients’ medical files and were completed during the initial phone call with the patients: date of diagnosis, breast tumor characteristics, cancer treatments, hormone therapy characteristics, pain medication, other medication, and medical history.
The participants completed a set of self-administered questionnaires that included sociodemographic characteristics (age, marital status, children, educational level, and professional status); validated scales commonly used in oncology to assess quality of life, depression, anxiety and fear of recurrence, additional ad hoc items related to arthralgia and its treatment.
Quality of life was assessed using the Medical Outcomes Study 36-item Short Form Health Survey (SF-36) [29], which contains eight subscales: physical functioning, role-physical, role-emotional, bodily pain, social functioning, mental health, vitality, and general health perceptions. Responses for each dimension were transformed into a score from 0 to 100, with higher scores representing better levels of quality of life. Two summary scores were also calculating: the physical component summary (PCS) and the mental component summary (MCS).
Emotional state was evaluated with two specific scales. The Beck Depression Inventory Short Form (BDI-SF) [30] is a screening and a diagnostic instrument for depression in medical patients. Answers to the 13 items are rated on a four-point scale from 0 to 3. The resulting score ranges from 0 to 39, with higher scores reflecting a higher probability of depressive symptomatology. We used the cutoff of 9 for screening (13 is generally considered as more specific but less sensitive). The Spielberger State-Trait Anxiety Inventory (STAI) [31] was administered to assess anxiety. The questionnaire consists of 40 items that measure two types of anxiety: state anxiety (present experience) and trait anxiety (general experience). The global score for each form ranges from 20 to 80. Higher scores indicate severe levels of anxiety.
Fear of recurrence (FoR) was explored with the short form of the Fear of Cancer Recurrence Inventory (FCRI) [32]. This contains nine items specifically designed to assess the severity of FoR through questions about the frequency and the duration of thoughts or pictures associated with the idea of cancer recurrence. Each item is scored from 0 to 4 and the global score varies from 0 to 36. A global score greater than 13 indicates a pathological level of fear.
Arthralgia-related details were collected through six questions that aimed to identify date of onset, localization, intensity, and evolution. Average severity of pain (in the past 8 days) was assessed using a 10-cm visual analog scale (VAS). Pain severity was classified into mild (VAS 0–3), moderate (VAS 3–6), and severe pain (VAS 6–10) as previous research conducted in cancer and noncancer populations have demonstrated the validity of these categories [33]. We investigated the intake of pain medication and the level of pain relief reached (10–cm VAS, 0 indicating an absence of relief and 10 total relief). The patients were also asked about what caused their pain. Nine answers (nonexclusive) were proposed: chemotherapy, radiotherapy, surgery, weight gain, aging, articular pathology, AI, another treatment, or another cause.
Representations concerning the AI were addressed through two questions, one of which asked why that treatment had been prescribed by the oncologist (five choices: treatment of cancer, treatment of menopausal symptoms, prevention of cancer recurrence, do not know, other reason), while the other asked if the patients had been informed by the oncologist of the side effects of AI (if yes, the patients had to indicate on a list the side effects they received information about).
Statistics
Patients were classified into two groups depending on whether they reported arthralgia or not. Demographic and clinical characteristics were compared between the groups using the Mann–Whitney U test for continuous variables and the chi-squared and the Fisher exact tests for categorical variables. Comparisons were then performed to assess group differences in the quality of life (SF-36), emotional state (BDI-SF, STAI), and fear of recurrence (FCRI) variables. Descriptive analyses were conducted on the pain data. Within the arthralgia group, we explored the relations between pain variables (severity, pain relief, pain medication—yes/no) and quality of life/emotional state variables by calculating the Spearman’s correlation coefficient or by using the Mann–Whitney U test, when appropriate. Similarly, we explored the relations between pain variables and fear of recurrence. We also used the Mann–Whitney U test to study how the representations of AI and their side effects (considered as dichotomous variables) could be related to FoR.
All analyses were conducted using the Statistical Package for the Social Sciences (SPSS, version 14). All nonparametric tests (selected in the light of the sample size) were two-sided, and the significance level was set at 5 %.
Results
Study population
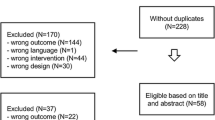
The final sample comprised 77 respondents, which represents a 77 % response rate (Fig. 1 summarizes the recruitment stages). Table 1 presents the demographic and medical characteristics of the study participants and distinguishes patients with or without arthralgia. There were no statistically significant differences of these variables between the two groups.
Prevalence and characteristics of arthralgia
In our study, 78 % of patients (n = 60) reported arthralgia. Pain was mainly described as mild (47 %, n = 27) to moderate (46 %, n = 26) and unstable (68 %, n = 41). The mean pain score was 3.8 out of 10.
Less than half of the patients with arthralgia (49 %, n = 27) were receiving pain medication: the most frequent were steps I (40 %, n = 12) and II (28 %, n = 8) according to the WHO ladder. In this treated group, the mean level of relief was estimated at 5.5 (SD = 2.72) out of 10.
About half of the patients (47 %, n = 27) used a nonpharmacological therapy such as physiotherapy (32 %, n = 19), relaxation therapy (5 %, n = 3), hypnosis (2 %, n = 1), acupuncture (17 %, n = 10).
In most cases, arthralgia was attributed to AI (80 %, n = 48). Musculoskeletal pathologies (57 %, n = 34), aging (44 %, n = 26), weight gain (26 %, n = 16), and chemotherapy (20 %, n = 12) were the other most frequently evocated causes (Fig. 2).
Quality of life and emotional state
Patients with arthralgia had a worse quality of life in all domains with the exception of General Health compared to patients without arthralgia (p < 0.05) ( Table 2). There was also a significant difference between groups on the PCS and on the MCS (lower score for patients with arthralgia) (p < 0.05).
A comparison of emotional outcomes showed a significant difference in state anxiety with higher scores being observed in the arthralgia group (p < 0.05). For trait anxiety, no difference was observed. However, there was no difference in depressive symptoms, with nonpathological mean levels being found in each group.
Within the arthralgia group, pain severity was significantly associated with the PCS (r = 0.375, p < 0.01) and the MCS (r = −0.442, p < 0, 01), the anxiety state (r = 0.322, p < 0.05) and the depression score (r = 0.474, p < 0.01): the more severe the pain was, the greater were the physical and mental difficulties, anxiety, and depressive symptoms experienced by the patients. No difference was observed according to the degree of pain relief and pain medication intake.
Factors associated with fear of recurrence
As hypothesized, the mean score for the arthralgia group (14.8) exceeded the pathological threshold (>13) and was higher in the arthralgia than in the nonarthralgia group (14.8 vs. 10.7, p < 0.01). Pain intensity was significantly and positively associated with the severity of FoR (r = 0.274, p < 0.05).
FoR score was not associated with the fact of receiving pain medication. However, in the group of arthralgia patients treated for pain, the greater was the level of pain relief, the lower was their FoR (r = −0.409, p < 0.05).
FoR did not appear to be associated with representations of the AI and its side effects (Table 3). There was no significant difference depending on whether the patients:
-
Knew or not that their treatment was aimed to decrease the risk of cancer recurrence (84 % of the total sample said they were aware of this)
-
Had or had not been informed about AI side effects including arthralgia (80 % of the total sample said they had been informed about side effects and 84 % about the risk of developing arthralgia)
-
Knew or not what caused their pain
-
Ascribed or not their pain to their treatment
Discussion
The first aim of our study was to describe the prevalence of arthralgia in a population of women in remission after breast cancer and treated with AI and the impact of arthralgia on quality of life and emotional state of these patients. Our analyses confirmed that arthralgia is indeed an important side effect of AI: 78 % of patients in our study reported arthralgia, i.e., a higher rate than generally expected [4, 14–19].
Arthralgia was associated with lower quality of life in seven of the eight assessed subscales, including the physical and the mental component summaries. Our results confirm findings reported by Olufade et al. [15]. Howver, the peculiarity of our study was to include specific anxiety and depression scales that allowed us to better assess the patient’s emotional state. As far as depressive symptomatology is concerned, we found nonpathological scores in both groups and there was no significant difference between groups. These results are consistent with the conclusions drawn by the teams led by Schilder [34] and Takei [9] which did not reveal any depressive symptoms in a population of patients receiving AI treatment (although these studies did not, however, distinguish between patients with and without arthralgia).
More specifically with reference to anxiety, the scale we used had the advantage of measuring both state anxiety (anxiety assessment at the present moment) and trait anxiety (characterization of an individual’s habitual tendency to exhibit anxiety). In our study, women with arthralgia had significantly higher anxiety scores than those without arthralgia. Moreover, the higher was the pain intensity, the higher was the anxiety score. Despite this, trait anxiety was nonpathological and identical in the two groups. This is a main outcome of this study as a high level of trait anxiety could have influenced the occurrence of pain as it has recently been suggested by Laroche et al. [14]. This was not the case in our study: the higher level of pain in one of the groups has no relationship with preexisting levels of anxiety.
The second aim of our study was to determine the relation between arthralgia and FoR. On the one hand, our analyses revealed that FoR was pathological and significantly higher in women who reported arthralgia than in those who did not, with a significant correlation between pain intensity and FoR level. As mentioned above, the absence of any difference between the two groups in terms of trait anxiety, which might have influenced the occurrence and intensity of FoR [25], is remarkable. Given to our cross-sectional design, those results suggest that pain impact FoR and not vice versa.
The existence of a significant association between pain relief due to pain medication and FoR intensity also supports this interpretation of results: as patient assessment of pain relief increases, FoR decreases. It is therefore unfortunate that only 49 % of patients received pharmacological treatment, most frequently as WHO step I or II pain medication, which could only partially relieve their pain. Other pharmacological classes of pain medication (WHO ladder step III, antiepileptics and antidepressants) were rarely reported. Furthermore, only half of the patients used nonpharmacological therapies which are known to be relevant for the treatment of chronic joint and muscle pain [35] and are starting to be successfully tested among patients receiving AI [36, 37].
We also hypothesized that FoR might be linked to erroneous representations of arthralgia or to a lack of information concerning the treatment and its side effects. However, our results showed that patients tended to be well informed about aims of treatment (i.e., to prevent recurrence) and their side effects. Furthermore, most of painful patients ascribed their arthralgia to their AI treatment and, to a lesser extent, to aging or to chemotherapy, but not to the cancer itself. In our study, being informed of the aims of the treatment and being aware of the causes of the arthralgia did not coincide with a reduced FoR. Based on Corter et al.’s ideas [28] on the role of the interpretation of residual symptoms in perpetuating FoR, it is possible that persistence of pain might act as a trigger that reminds sufferers of their illness and then allow them to interpret, more or less consciously, pain as a sign of recurrence, and this even though they are in possession of knowledge concerning the treatment and the origins of their pain that contradicts this belief.
Our study has certain limitations. The small sample size did not allow us to test the linear regression model and explains why we performed nonparametric analyses. The cross-sectional approach cannot allow us to establish with certainty any causal links in the observed association between arthralgia, anxiety, and FoR.
Nevertheless, as we have seen above, the difference in the results between trait anxiety and state anxiety supports the hypothesis that pain plays a crucial role. A prospective study involving a qualitative dimension may help define coping abilities mobilized by these patients, and explore in greater detail the cognitive process involved in the erroneous interpretation of pain.
Earlier studies of FoR have shown that it is characterized by intrusive thoughts similar to concerns observed in generalized anxiety disorder, and indeed to obsessions that are more closely associated with obsessive-compulsive disorder [38]. We know that the cognitive models of anxious disorder emphasize the importance of the subject’s basic cognitive schemas in the erroneous evaluation of intrusive thoughts [39]. An evaluation of these schemas might allow us to gain a better understanding of the processes involved in the incorrect processing of the information and thus contribute to the development of suitable care models for the behavioral and cognitive therapies that are already effectively employed to manage emotional distress, including FoR, among patients in remission of their cancer [40, 41] or in a situation of chronic pain [42, 43]. Another treatment approach could be pharmacological, based on antidepressants’ use: in fact, some of them (serotonin norepinephrine reuptake inhibitors (SNRIs)) are known to be effective in the treatment not only of depression and anxiety but also of chronic pain [44]. Recently, Henry et al. [45] studied a small group of patients receiving AI and found a reduction in joint and muscle pain following 8 weeks of duloxetine (SNRI). However, these interesting results will have to be confirmed in a randomized study involving a larger number of patients and a control group.
Conclusion
Our study has confirmed the existence of a correlation between arthralgia and an impaired quality of life, at physical but also mental levels. It has also revealed a close relationship between pain intensity and FoR, in particular by showing that effective pain medication is accompanied by a reduced FoR. Another important finding was that information regarding aims of AI treatment and its side effects, in particular with regard to arthralgia, although essential, was inadequate to overcome the patients’ intense concerns with regard to pain. We therefore consider as a main issue to raise awareness among oncologists in systematic screening of arthralgia and implementing state of the art pain management. This strategy may be promoted by diffusion of current guidelines about pain treatment, development of new pharmacological strategies if needed, and offer a better access to nonpharmacological treatments.
References
Aydiner A (2013) Meta-analysis of breast cancer outcome and toxicity in adjuvant trials of aromatase inhibitors in postmenopausal women. Breast 22:121–129
Amir E, Seruga B, Niraula S, Carlsson L, Ocaña A (2011) Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst 103:1299–1309
Niravath P (2013) Aromatase inhibitor-induced arthralgia: a review. Ann Oncol 24:1443–1449
Gaillard S, Stearns V (2011) Aromatase inhibitor-associated bone and musculoskeletal effects: new evidence defining etiology and strategies for management. Breast Cancer Res 13:205
Buzdar A, Howell A, Cuzick J et al (2006) Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol 7:633–643
Coates AS, Keshaviah A, Thürlimann B et al (2007) Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1–98. J Clin Oncol 25:486–492
Coombes RC, Kilburn LS, Snowdon CF et al (2007) Survival and safety of exemestane versus tamoxifen after 2–3 years' tamoxifen treatment (Intergroup Exemestane Study): a randomised controlled trial. Lancet 369:559–570
Goss PE, Ingle JN, Martino S et al (2005) Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst 97:1262–1271
Takei H, Ohsumi S, Shimozuma K, Takehara M, Suemasu K, Ohashi Y, Hozumi Y (2012) Health-related quality of life, psychological distress, and adverse events in postmenopausal women with breast cancer who receive tamoxifen, exemestane, or anastrozole as adjuvant endocrine therapy: National Surgical Adjuvant Study of Breast Cancer 04 (N-SAS BC 04). Breast Cancer Res Treat 133:227–236
Fallowfield LJ, Kilburn LS, Langridge C, Snowdon CF, Bliss JM, Coombes RC (2012) Long-term assessment of quality of life in the Intergroup Exemestane Study: 5 years post-randomisation. Br J Cancer 106:1062–1067
Cella D, Fallowfield L, Barker P, Cuzick J, Locker G, Howell A (2006) Quality of life of postmenopausal women in the ATAC ("Arimidex", tamoxifen, alone or in combination) trial after completion of 5 years' adjuvant treatment for early breast cancer. Breast Cancer Res Treat 100:273–284
van Nes JG, Fontein DB, Hille ET, Voskuil DW, van Leeuwen FE, de Haes JC, Putter H, Seynaeve C, Nortier JW, van de Velde CJ (2012) Quality of life in relation to tamoxifen or exemestane treatment in postmenopausal breast cancer patients: a Tamoxifen Exemestane Adjuvant Multinational (TEAM) Trial side study. Breast Cancer Res Treat 134:267–276
Whelan TJ, Goss PE, Ingle JN et al (2005) Assessment of quality of life in MA.17: a randomized, placebo-controlled trial of letrozole after 5 years of tamoxifen in postmenopausal women. J Clin Oncol 23:6931–6940
Laroche F, Coste J, Medkour T et al (2014) Classification of and risk factors for estrogen deprivation pain syndromes related to aromatase inhibitor treatments in women with breast cancer: a prospective multicenter cohort study. J Pain 15:293–303
Olufade T, Gallicchio L, MacDonald R, Helzlsouer KJ (2015) Musculoskeletal pain and health-related quality of life among breast cancer patients treated with aromatase inhibitors. Support Care Cancer 23:447–455
Mao JJ, Stricker C, Bruner D, Xie S, Bowman MA, Farrar JT, Greene BT, DeMichele A (2009) Patterns and risk factors associated with aromatase inhibitor-related arthralgia among breast cancer survivors. Cancer 115:3631–3639
Henry NL, Giles JT, Ang D et al (2008) Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat 111:365–372
Crew KD, Greenlee H, Capodice J, Raptis G, Brafman L, Fuentes D, Sierra A, Hershman DL (2007) Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol 25:3877–3883
Presant CA, Bosserman L, Young T, Vakil M, Horns R, Upadhyaya G, Ebrahimi B, Yeon C, Howard F (2007) Aromatase inhibitor-associated arthralgia and/ or bone pain: frequency and characterization in non-clinical trial patients. Clin Breast Cancer 7:775–778
Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J (2008) Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 30:112–126
Reich M, Lesur A, Perdrizet-Chevallier C (2008) Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat 110:9–17
Crist JV, Grunfeld EA (2013) Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology 22:978–986
van den Beuken-van Everdingen MH, Peters ML, de Rijke JM, Schouten HC, van Kleef M, Patijn J (2008) Concerns of former breast cancer patients about disease recurrence: a validation and prevalence study. Psychooncology 17:1137–1145
Janz NK, Hawley ST, Mujahid MS, Griggs JJ, Alderman A, Hamilton AS, Graff JJ, Jagsi R, Katz SJ (2011) Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer 117:1827–1836
Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, Ozakinci G (2013) Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv 7:300–322
Leventhal H, Diefenbach M, Leventhal EA (1992) Illness cognition: using common sense to understand treatment adherence and affect cognition interactions. Cognit Ther Res 16:143–163
Lee-Jones C, Humphris G, Dixon R, Hatcher MB (1997) Fear of cancer recurrence–a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology 6:95–105
Corter AL, Findlay M, Broom R, Porter D, Petrie KJ (2013) Beliefs about medicine and illness are associated with fear of cancer recurrence in women taking adjuvant endocrine therapy for breast cancer. Br J Health Psychol 18:168–181
Leplège A, Ecosse E, Verdier A, Perneger TV (1998) The French SF-36 Health Survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol 51:1013–1023
Furlanetto LM, Mendlowicz MV, Romildo Bueno J (2005) The validity of the Beck Depression Inventory-Short Form as a screening and diagnostic instrument for moderate and severe depression in medical inpatients. J Affect Disord 86:87–91
Bruchon-Schweitzer M, Paulhan I (1993) Manuel de l'inventaire d'anxiété état-trait forme Y (STAI-Y) de Spielberger. Editions du Centre de Psychologie Appliquée, Paris
Simard S, Savard J (2009) Fear of Cancer Recurrence Inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer 17:241–251
Paul SM, Zelman DC, Smith M, Miaskowski C (2005) Categorizing the severity of cancer pain: further exploration of the establishment of cutpoints. Pain 113:37–44
Schilder CM, Eggens PC, Seynaeve C, Linn SC, Boogerd W, Gundy CM, Beex LV, Van Dam FS, Schagen SB (2009) Neuropsychological functioning in postmenopausal breast cancer patients treated with tamoxifen or exemestane after AC-chemotherapy: cross-sectional findings from the neuropsychological TEAM-side study. Acta Oncol 48:76–85
Cunningham NR, Kashikar-Zuck S (2013) Nonpharmacological treatment of pain in rheumatic diseases and other musculoskeletal pain conditions. Curr Rheumatol Rep 15:306
Mao JJ, Xie SX, Farrar JT, Stricker CT, Bowman MA, Bruner D, DeMichele A (2014) A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer 50:267–276
Bao T, Cai L, Giles JT et al (2013) A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 138:167–174
Simard S, Savard J, Ivers H (2010) Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. J Cancer Surviv 4:361–371
Alford BA, Beck AT (1997) The integrative power of cognitive therapy. The Guilford Press, New York
Osborn RL, Demoncada AC, Feuerstein M (2006) Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med 36:13–34
Herschbach P, Book K, Dinkel A, Berg P, Waadt S, Duran G, Engst-Hastreiter U, Henrich G (2010) Evaluation of two group therapies to reduce fear of progression in cancer patients. Support Care Cancer 18:471–479
Ehde DM, Dillworth TM, Turner JA (2014) Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol 69:153–166
Sturgeon JA (2014) Psychological therapies for the management of chronic pain. Psychol Res Behav Manag 7:115–124
Watson CP, Gilron I, Sawynok J, Lynch ME (2011) Nontricyclic antidepressant analgesics and pain: are serotonin norepinephrine reuptake inhibitors (SNRIs) any better? Pain 152:2206–2210
Henry NL, Banerjee M, Wicha M, Van Poznak C, Smerage JB, Schott AF, Griggs JJ, Hayes DF (2011) Pilot study of duloxetine for treatment of aromatase inhibitor-associated musculoskeletal symptoms. Cancer 117:5469–5475
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lopez, C., Charles, C., Rouby, P. et al. Relations between arthralgia and fear of recurrence: results of a cross-sectional study of breast cancer patients treated with adjuvant aromatase inhibitors therapy. Support Care Cancer 23, 3581–3588 (2015). https://doi.org/10.1007/s00520-015-2722-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2722-9