Abstract
The layout of this study, designed as a randomized crossover clinical trial, is to evaluate the efficacy of an intervention with mineral-medicinal water from As Burgas (Ourense) in patients suffering from fibromyalgia. This sample was randomly divided into two groups: group A and group B. In phase 1, group A had 14 baths in thermal water for a month and standard pharmacological treatment; group B, standard pharmacological treatment. Washout period is 3 months. In phase 2, group A had standard treatment and group B had 14 baths in thermal water for a month plus standard treatment. The Fibromyalgia Impact Questionnaire (FIQ) was used; this grades the impact of the illness from 1 (minimum) to 10 (maximum), which was measured in both phases. Twenty-five patients were included in each group and the study was concluded with 20 patients in group A and 20 in group B. The intervention group obtained, once the baths finished, a mean score of 60.3 (± 11.8) and the control group of 70.8 (± 13.0) (p < 0.001). Three months later, the intervention group presented a mean score of 64.4 (± 10.6) and the control group of 5.0 (± 11.3) (p < 0.001). We can therefore conclude that the simple baths with mineral-medicinal water from As Burgas can make an improvement on the impact caused by fibromyalgia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia is, still nowadays, a syndrome with little known etiology, characterized by generalized skeletal muscle pain accompanied by other diverse symptoms, such as fatigue, sleep disturbances, and anxiety and depression issues, among others (Wolfe et al. 2013). Its treatment is usually complex (Macfarlane et al. 2017) and, in many occasions, unsatisfactory, placing the fibromyalgia (FM) as a public health problem due to the significant health expenditure generated, which is mainly translated in a high rate of medical consultations and a high consumption of drugs (Arnold et al. 2018).
Taking into account the chronicity and idiopathic origin of this syndrome, the primary aim of treatment should be focused on improving the quality of life of patients, and evidence makes clear the need to combine pharmacological treatments with non-pharmacological ones (Häuser et al. 2012). Among these last ones, balneotherapy has been proved an effective strategy in the treatment of chronic pain (Morer et al. 2017; Karagülle et al. 2017). It is a safe therapeutic option, with little adverse effects (Langhorst et al. 2009) and usually well tolerated by patients, providing analgesia, sedation, and muscular rejuvenation (Naumann et al. Sadaghiani Naumann and Sadaghiani 2014), which has great importance in this pathology.
The main aim of this study is to assess the efficacy of an intervention with mineral-medicinal water in patients with fibromyalgia, which could lead to a clinically relevant reduction in parameters of affectation at the end of the intervention and after 1 month, measured with the Fibromyalgia Impact Questionnaire (FIQ). As secondary objectives, positive changes in hemodynamic variables (systolic, diastolic, and pulse pressure), drug consumption, and allodynia will be evaluated.
Materials and methods
Study design and patient selection
A randomized crossover clinical trial (RCT) was proposed, being developed between January 2016 and January 2017. The study was approved by the Autonomous Committee of Research Ethics of Galicia (Registration Code 2016/362).
Patients were invited by the doctors and nurses from a health center in the city of Ourense to participate. In case of acceptance, an appointment to a consultation with two nurses that were members of the research team would be set. Afterwards, they would be provided with the information sheet and the informed consent form that needed to be signed. At that point, the measurements would be taken. Furthermore, they were provided with health education guidelines, emphasizing the benefits of the abandonment of certain harmful behaviors, especially sedentary lifestyle.
Participants: inclusion and exclusion criteria
Male and female patients aged between 18 and 65 and diagnosed with FM according to the criteria of the American College of Rheumatology of 2010 were included (Wolfe et al. 2010), excluding those who had absolute or relative contraindications for taking baths of mineral-medicinal (MM) water such as the following: acute phase illnesses, tumors, cardiac, respiratory or renal terminal insufficiencies, severe metabolic disorders, severe or decompensated arterial hypertension, and recent cerebrovascular accidents, also post-traumatic and postoperative processes, hypotension, vascular pathologies, history of fractures due to osteoporosis, or uncontrolled thyroid diseases (Bazzichi et al. 2013; Fazaa et al. 2014; Bağdatlı et al. 2015; Branco et al. 2016; Fioravanti et al. 2018). We also excluded patients who had taken baths with MM water during the last year, those who suffered from psychiatric or cognitive disorders, had a disability that limited their participation, pregnant women, those who had taken part in other clinical trials, and patients who did not consent to participate.
Intervention
The sample was randomly divided into two groups: group A and group B. The study was, likewise, divided into two phases.
Phase 1
The patients of group A took 14 baths, 30-min long for a month, in bicarbonated sodium water of medium mineralization, alkaline, lithic, fluorinated, silicated, with a temperature of 38 °C in the thermal and public pool of As Burgas (Ourense), while they carried on taking the treatment prescribed by their doctor. On the other hand, patients in group B only followed the usual pharmacological treatment prescribed by their doctor that they were already taking before the study commenced.
The two groups were subjected to four measurements: baseline, a measurement when group A finished the baths, another one a month later, and the last one, 3 months after receiving the baths. Subsequently, the entire sample maintained a 3-month washout period. This washout period was planned so that there were no residual therapeutic effects of the baths in group A before starting the second phase of the trial, and it was made based on other study results (Bağdatlı et al. 2015; Koçyiğit et al. 2016); all of them were RCTs of parallel groups, since no studies with a cross design that could be used as a model were found.
Phase 2
Once the washout period was completed, the baseline measurements were again collected from the two groups of participants. Subsequently, the groups were crossed. Thus, only group A carried on with its usual pharmacological treatment and patients from group B received the same intervention in As Burgas thermal pool as group A in the first phase, in addition to continuing with the treatment prescribed by the doctor. The two groups were once again measured at the end of group B baths, 1 month after and 3 months later.
From the beginning of the study and throughout it, and with the aim of not masking the pain, clear instructions were given to the patients to not take symptomatic drugs 1 day before the different checkups. Likewise, they were told to not start any non-pharmacological therapy that could alter the results of the study.
Studied variables
Sociodemographic and epidemiological data, such as sex, age, marital status, studies, occupation, smoking habits, or body mass index, were collected. As a primary outcome, the clinically relevant reduction in the affectation parameters was suggested, being this measured with the FIQ. As secondary outcomes, we considered the positive changes in the hemodynamic variables (systolic and diastolic blood pressure and heart rate measured with the Omrom M-2 tensiometer), the intake of drugs for FM (grouping them in analgesics, antidepressants, anticonvulsants, and muscle relaxants), and allodynia, measured with the Omrom M-2 blood pressure cuff, which measures the intensity of the stimulus needed to produce pain and, the lowest this is, the highest is the allodynia index (Chandran et al. 2012; Cassisi et al. 2014). To measure the primary outcome of the fibromyalgia impact, the FIQ was used. This questionnaire is a validated instrument that assesses the impact of fibromyalgia over physical capacity, such as subjective signs closely related to this syndrome (Salgueiro et al. 2013). The scoring ranges from 1 to 100, with 1 being the highest functional capacity and quality of life (minimum impact of fibromyalgia) and 100 the maximum impact.
Sample size and randomization
The sample size was calculated based on the study by Bağdatlı et al. (2015), in which an average FIQ score of 51.2 points was observed in the experimental group before the intervention and a reduction of the score close to 12 points after the intervention. According to this, we estimated an average post-intervention FIQ score of 39.0 points and a standard deviation of the difference of 18.0 points. Under these assumptions, to achieve a power of the 80% to detect differences in contrast of the hypothesis by a comparison test of means for two related samples, taking into account a level of significance of 5%, 20 pairs of subjects were needed in the study. Assuming a percentage of losses and/or dropouts of 20%, it was necessary to recruit 25 pairs of subjects. The recruitment period was carried out during the months of January and February 2016. The first 50 patients who met the inclusion criteria and who agreed to participate were included in the study.
For the allocation of patients to one of the two groups, a randomization list generated automatically by an outside collaborator was used, keeping the sequence hidden for the research team until the intervention was assigned. The study was open, so there was no blinding of the participants or the researchers regarding the assigned group, nor in the evaluation of the results. However, monitoring was carried out by internal and external auditors to guarantee the quality of the data.
Statistical analysis
Descriptive analyses (expressing the continuous variables in mean and standard deviation (SD) and qualitative variables in absolute numbers and percentages) and comparison tests (Student’s t test for independent and paired samples and McNemar test), as well as normality tests of continuous variables (Shapiro-Wilks test), were performed. If the last ones did not present a normal distribution, the non-parametric tests of Mann-Whitney and Wilcoxon were used. Intention-to-treat analyses were conducted to keep the advantages of randomization regarding known or unknown variables that could influence the results, and analysis by protocol. The study losses were analyzed separately. The analyses were performed with the software SPSS version 19.
Results
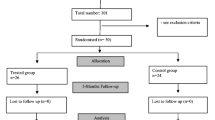
Of the 191 men and women from the health center diagnosed with FM, 106 (75.2%) did not meet the inclusion criteria, 20 (14.2%) could not be contacted, and 15 (10.6%) did not accept to participate. Fifty were the individuals that started the study, finalizing 41 of them, with a total percentage of losses of the 18% (4 subjects in group A and 5 subjects in group B), not observing significant differences between the lost sample and the one that carried on with the study. Among the lost cases, 6 of them left due to work causes, 2 due to illness, and 1 due to pregnancy. Figure 1 shows the flow of participants in each stage of the trial according to the CONSORT diagram.
The subjects were mostly women (48, 96%), with an average age of 52.9 ± 9.9, were married or lived as a couple (35, 70%), and had secondary school education (29, 58%), and 25 (50%) were active. Their mean BMI was 28.1 ± 4.6; 13 of the subjects smoked (26%) and had an average evolution of the disease of 14.2 years since the diagnosis (± 4.0).
Initially, the homogeneity of the sample was checked after the random assignment of the subjects in the two groups, not observing statistically significant differences between them, except the systolic blood pressure (p = 0.026), the intake of muscle relaxant drugs (p = 0.042), and the intake of anticonvulsant drugs (p = 0.047) (Table 1).
Intra-group comparison
FIQ results
By analyzing group A results in the two phases of the study, we can observe that in both, first and second phases, the FIQ score means after the 3-month washout period have remained statistically significantly lower than the baseline mean in the first phase; except the last measurement 11 months after receiving the baths. In the first phase of the study, group A baseline mean was 79.4 ± 10.2, being 61.9 ± 13.0 (p < 0.001) at the end of the baths; 66.3 ± 12.9 (p < 0.001) 1 month after; and 64.2 ± 11.0 (p < 0.001) 3 months later. During the second phase, when group A was the control, the score was 64.4 ± 8.7 (p < 0.001) after the baseline measurement (performed 6 months after receiving the baths). The following measurement in this group, 7 months after receiving the baths, was 64.6 ± 11.5 (p < 0.001); the next one, 8 months later, was 68.2 ± 12.3 (p = 0.002); and the last measurement, 11 months after receiving the baths, was 74.0 ± 10.0 (p = 0.070).
On the other hand, group B FIQ score means, being this group not subjected to any intervention during the first phase of the study, did not show significant changes, with a baseline measurement of 74.2 ± 11.3 at the beginning of the study, 77.4 ± 11.3 (p = 304) when group A finished the baths, 73.8 ± 17.5 (p = 0.936) 1 month after, and 76.2 ± 12.8 (p = 0.551) 3 months later. During the second phase of the study, the baseline measurement after the washout period was 77.3 ± 6.7 (p = 0.145). It was during this phase when both groups were crossed, being group B the intervention target with mineromedicinal water baths. Thus, just at the end of the baths, the average score was 58.7 ± 10.5 (p < 0.001); 63.7 ± 9.8 (p = 0.002) 1 month after, and 64.7 ± 10.6 (p = 0.020) 3 months later.
Allodynia results
On top of this, the allodynia results in group A also showed significant changes like the FIQ ones, as it can be observed in Fig. 3.
A carry-over effect was observed in the design of the study, since group A, the one that started the intervention with baths in phase 1, maintained, after the bleaching period in the second phase of the study, in the which it acted as control group, improvements in both aspects, since the differences in the FIQ and allodynia means were significant, compared with the first baseline measurement in the first phase, as it can be observed in Figs. 2 and 3.
Inter-group comparison
FIQ results
The main objective of the study, the impact of fibromyalgia measured with the FIQ in the three measurements carried out (just after the baths, 1 month, and 3 months later) to the two groups (control and intervention with baths) during both phases (first and second), shows that the impact on the group that was taking the baths was always lower (Table 2; Fig. 4). The average score in the control group at the end of the baths was 70.9 ± 13.0 and 60.4 ± 11.8 in the group taking the baths (p < 0.001). The mean score was 71.3 ± 15.1 in the control group a month later and 65 in the group taking the baths (± 11.4, p < 0.001). Three months after the baths were finished, the control group showed an average score of 75.0 ± 11.4 and the group that took the baths, of 64.4 ± 10.7 (p < 0.001).
Comparison of the average FIQ scores in the intervention groups (group A in the first phase and group B in the second phase) and in the control groups (group B in the first phase and group A in the second phase), at the end of the baths, 1 month, and 3 months later. FIQ: Fibromyalgia Impact Questionnaire; p: calculated with Student’s t test for related samples tiff
Allodynia results
In regard to one of the secondary objectives, the improvement or increase of the mean in the allodynia data, we were able to observe that just at the end of the baths and 1 month later, both groups did not show statistically significant differences. However, 3 months after the intervention, the group subjected to the baths presented a significant improvement against the other group, as it can be observed in Table 2 and Fig. 5.
Comparison of the average allodynia scores in the intervention groups (group A in the first phase and group B in the second phase) and in the control groups (group B in the first phase and group A in the second phase), at the end of the baths, 1 month, and 3 months later. p: calculated with Student’s t test for related samples tiff
Regarding the other variables, such as hemodynamic values and drug intake, no significant differences were observed in the different measurements carried out throughout the study.
Discussion
In the present study, after the administration of a protocol of baths with MM water to patients diagnosed with FM, a significant improvement in the impact caused by the disease was found. This was measured with the FIQ several months after the intervention. Our study is the first one to use a crossover RCT design to measure the therapeutic use of MM baths in patients with fibromyalgia. The choice of this type of design was to give scientific value to a type of coadjuvant therapy that, in our environment and until now, has not been taken into sufficient consideration by health professionals.
A consensus on the therapeutic management of fibromyalgia has been reached (Macfarlane et al. 2017), highlighting the importance of the multidisciplinary approach and giving special emphasis to non-pharmacological treatments; and even more recently, an evidence-based diagnostic system for this illness has been established, based on the ACTTION-APS taxonomy (Arnold et al. 2018). This taxonomy includes mechanisms, common characteristics, comorbidities, and diagnostic criteria that could improve the recognition of FM in clinical practice.
FM has been suggested to be a clinical manifestation of the central nervous system hypersensitivity (Yunus 2008), being this hypersensitivity the main mechanism involved in the development and maintenance of chronic pain (Woodman 2013). There is evidence of altered central pain pathways, suggesting that stress peptides that trigger the release of inflammatory and neurosensitizing mediators take part in neuroinflammation (Theoharides et al. 2015). The immersion in mineral-medicinal water has been proved to cause physiological effects both locally and generally, exerted by physical, chemical, and biological mechanisms (Fioravanti et al. 2011; Galvez et al. 2018). Perhaps for this reason, the temperature rise and the effect of hydrostatic pressure generated by thermal baths can produce analgesia by increasing the pain threshold (Ardıç et al. 2007). These findings have been confirmed by other investigators by pointing out that in patients with fibromyalgia, a protocol of baths with water MM can reduce certain mediators of inflammation and pain, and that this may be due to the chemical components of the water (Guidelli et al. 2012). If we add to these properties its possible antioxidant action, we would have the answer to the therapeutic benefit observed (Prandelli et al. 2013).
Balneotherapy deserves to be currently considered as another therapy in the treatment of fibromyalgia (Forestier et al. 2017) and along this line are the studies developed by different authors. Koçyiğit et al. (2016)) carried out an RCT in a spa with 61 participants; all of which were provided with health education guidelines. The members of the intervention group were given a series of 21 mineromedicinal water baths of 20 min of duration 5 days a week. The control group carried on with the usual treatment. Pre-intervention measurements were carried out, and also after15 days, a month, and 3 and 6 months later, finding a significant improvement in the impact caused by the disease on the group having the baths against the control group up to 3 months after the intervention. One hundred patients took part in the study by Fioravanti et al. (2018); it was also carried out in a spa and measurements were taken in the same time intervals as those by Kocyigit; however, there were no more similarities between the two studies. This has been the first double-blind study on FM balneotherapy that has been done so far. The intervention group received 12 baths with MM water for 2 weeks. The baths had a duration of 15 min followed by a 15-min rest. On the other hand, the control group also received 12 baths of 15 min duration and 15-min rest, but the baths were, in this case, in hot potable water that was applied with a dye to simulate the color of the mineral-medicinal water. In the results, they found significant differences between both groups up to 6 months after the experiment.
Our results were also along line with other literatures. Over three follow-up months, the group that received the baths showed significant improvement compared with the control group. However, in our study, as an unforeseen finding and due to circumstances related to the design, improvement was also found after the intervention with significant results up to 8 months after it. In crossed RCTs, the tested effect must occur quickly and has a short duration, in addition to remaining stable during the two periods of the study. When choosing the design and adjusting the measurement periods and washout, other works were analyzed; all of them were RCTs of parallel groups, since, as we have mentioned previously, we could not find studies with a crossover design that could serve us as a model. The consulted works carried out measurements 3 months after the intervention (Neumann et al. 2001; Buskila et al. 2001; Altan et al. 2004; Nugraha et al. 2011; Özkurt et al. 2012; Bağdatlı et al. 2015), 4 months (Fioravanti et al. 2007), and 6 months (Evcik et al. 2002; Koçyiğit et al. 2016; Fioravanti et al. 2018), and only in one study, the measurements were repeated 9 months later (Dönmez et al. 2005). In all these studies, it was possible to maintain a 3-month therapeutic effect mainly, reaching a maximum of 6 months in those mentioned above. For this reason, we proposed a 3-month washout period in the design of this study, in order to avoid residual therapeutic effects of the baths in group A before starting the second phase of the trial. Therefore, patients in this group spent 6 months from the time they received the baths in the first phase of the study until the end of the washout period, which, according to the scientific findings made up to that moment, seemed initially enough time. However, this was not the case, given that this beneficial effect was maintained significantly up to 8 months after finishing baths with MM waters, reaching up to 11 months later (difference not statistically significant but clinically relevant). This finding revealed the inadequate design of the study. However, on the other hand, we found that simple baths in a public pool with MM water maintained good therapeutic results for a longer period of time than in the previously mentioned studies, which leads us to affirm that MM water improved the FM symptoms in a group of patients and that this improvement could last up to 8 months.
This is the first international study that has been designed as a RCT in patients suffering from fibromyalgia, where the effect of the baths and the control are assessed in the same individual, obtaining this way a lower variability than if the comparison of the effect was performed in different subjects, as it is the case of parallel RCTs. However, until the present work, no parallel studies had been carried out in Spain either.
On the other hand, both the controls and the experimental group in a large number of the published studies were accommodated and received the different types of interventions in spas. It has been shown that patients who abandon their daily routine and are in a different environment, such as a spa, interacting and socializing with other patients can feel an improvement in the pathological processes they suffer (Baysal et al. 2018). However, in our study, the participating subjects received the baths in a public thermal pool, accessible to any citizen and to which they came only for this therapeutic activity. This last aspect of accessibility, despite being characteristic of the city where the study was carried out, is relevant from a healthcare point of view, since it outlines the possibility for health professionals of using these thermal baths as a contributing therapeutic resource for certain pathologies.
Among the limitations of the study, we find the lack of blinding of the patients due to it not being allowed by the intervention, since the city where it was developed has no other spaces like the free mineral-medicinal water springs, which just have hot potable water. Another aspect is that the sample studied was not very large, but it was still possible to detect significant differences, since the proposed design allows the same sample to work with greater statistical power. On the other hand, the washout time was proven not to be sufficient, situation that caused a carry-over effect. Nevertheless, this methodological failure facilitated the verification of the long duration of the therapeutic effect provided by the MM waters. It could be interesting to carry out a follow-up of the sample to deepen in the therapeutic effect that MM water has over this pathology.
In conclusion, the impact caused by FM has been improved in this study by an intervention of 14 half-hour baths with MM water in patients diagnosed with the illness, and the improvement has lasted significantly for 8 months.
References
Altan L, Bingöl U, Aykac M et al (2004) Investigation of the effects of pool-based exercise on fibromyalgia syndrome. Rheumatol Int 24:272–277
Ardıç F, Özgen M, Aybek H, Rota S, Çubukçu D, Gökgöz A (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446
Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, Fitzcharles MA, Paiva ES, Staud R, Sarzi-Puttini P, Buskila D, Macfarlane GJ (2018) AAPT diagnostic criteria for fibromyalgia. J Pain. https://doi.org/10.1016/j.jpain.2018.10.008
Bağdatlı AO, Donmez A, Eröksüz R, Bahadır G, Turan M, Erdoğan N (2015) Does addition of ‘mud-pack and hot pool treatment’ to patient education make a difference in fibromyalgia patients? A randomized controlled single blind study. Int J Biometeorol 59:1905–1911
Baysal E, Leblebicioğlu H, Khorshid L, Sarı D (2018) Why individuals choose balneotherapy and benefit from this kind of treatment. Complement Ther Clin Pract 32:157–162
Bazzichi L, Da Valle Y, Rossi A, et al (2013) A multidisciplinary approach to study the effects of balneotherapy and mud-bath therapy treatments on fibromyalgia. Clin Exp Rheumatol 31:111–20
Branco M, Rego NN, Silva PH et al (2016) Bath thermal waters in the treatment of knee osteoarthritis: a randomized controlled clinical trial. Eur J Phys Rehabil Med 52:422–430
Buskila D, Abu-Shakra M, Neumann L, Odes L, Shneider E, Flusser D, Sukenik S (2001) Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int 20:105–108
Cassisi G, Sarzi-Puttini P, Casale R, Cazzola M, Boccassini L, Atzeni F, Stisi S (2014) Pain in fibromyalgia and related conditions. Reumatismo 66:72–86
Chandran AB, Coon CD, Martin SA, McLeod LD, Coles TM, Arnold LM (2012) Sphygmomanometry-evoked allodynia in chronic pain patients with and without fibromyalgia. Nurs Res 61:363–368. doi. https://doi.org/10.1097/NNR.0b013e318259b6cc
Dönmez A, Karagülle MZ, Tercan N, Dinler M, İşsever H, Karagülle M, Turan M (2005) SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26:168–172
Evcik D, Kızılay B, Gökçen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59
Fazaa A, Souabni L, Abdelghani KB, et al (2014) Comparison of the clinical effectiveness of thermal cure and rehabilitation in knee osteoarthritis. A randomized therapeutic trial. Ann Phys Rehabil Med 57:561–69
Fioravanti A, Perpignano G, Tirri G, Cardinale G, Gianniti C, Lanza CE, Loi A, Tirri E, Sfriso P, Cozzi F (2007) Effects of mud-bath treatment on fibromyalgia patients: a randomized clinical trial. Rheumatol Int 27:1157–1161
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8
Fioravanti A, Manica P, Bortolotti R, Cevenini G, Tenti S, Paolazzi G (2018) Is balneotherapy effective for fibromyalgia? Results from a 6-month double-blind randomized clinical trial. Clin Rheumatol 37:2203–2212
Forestier R, Erol-Forestier FB, Francon A (2017) Current role for spa therapy in rheumatology. Joint, Bone, Spine 84:9
Galvez I, Torres-Piles S, Ortega-Rincón E (2018) Balneotherapy, immune system and stress response: a hormetic strategy? Int J Mol Sci 19:1687
Guidelli G, Tenti S, De Nobili E et al (2012) Fibromyalgia syndrome and spa therapy: myth or reality? Clin Med Insights: Arthritis and Musculoskel Disord 5:19–26
Häuser W, Jung E, Erbslöh-Möller B, Gesmann M, Kühn-Becker H, Petermann F, Langhorst J, Thoma R, Weiss T, Wolfe F, Winkelmann A (2012) The German fibromyalgia consumer reports–a cross-sectional survey. BMC Musculoskelet Disord 13:74
Karagülle M, Kardeş S, Karagülle MZ (2017) Real-life effectiveness of spa therapy in rheumatic and musculoskeletal diseases: a retrospective study of 819 patients. Int J Biometeorol 61:1945–1956
Koçyiğit BF, Gür A, Altındağ Ö et al (2016) Comparison of education and balneotherapy efficacy in patients with fibromyalgia syndrome: a randomized, controlled clinical study. Ağrı J Turkish Soc Algology 28:72–78
Langhorst J, Musial F, Klose P, Hauser W (2009) Efficacy of hydrotherapy in fibromyalgia syndrome--a meta-analysis of randomized controlled clinical trials. Rheumatology (Oxford) 48:1155–1159
Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, Choy E, Kosek E, Amris K, Branco J, Dincer F, Leino-Arjas P, Longley K, McCarthy GM, Makri S, Perrot S, Sarzi-Puttini P, Taylor A, Jones GT (2017) EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis 76:318–328
Morer C, Roques CF, Françon A, Forestier R, Maraver F (2017) The role of mineral elements and other chemical compounds used in balneology: data from double-blind randomized clinical trials. Int J Biometeorol 61:2159–2173
Naumann J, Sadaghiani C (2014) Therapeutic benefit of balneotherapy and hydrotherapy in the management of fibromyalgia syndrome: a qualitative systematic review and meta-analysis of randomized controlled trials. Arthritis Res Ther 16:R141
Neumann L, Sukenik S, Bolotin A, Abu-Shakra M, Amir M, Flusser D, Buskila D (2001) The effect of balneotherapy at the Dead Sea on the quality of life of patients with fibromyalgia syndrome. Clin Rheumatol 20:15–19
Nugraha B, Neues-Lahusen M, Candir F, et al (2011) Wirkungen serieller H2S-Mineralwasserbäder auf Schmerzen bei Patienten mit Fibromyalgiesyndrom–eine Pilotstudie. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin 21:284–89
Özkurt S, Dönmez A, Karagülle MZ et al (2012) Balneotherapy in fibromyalgia: a single blind randomized controlled clinical study. Rheumatol Int 32:1949–1954
Prandelli C, Parola C, Buizza L, Delbarba A, Marziano M, Salvi V, Zacchi V, Memo M, Sozzani S, Calza S, Uberti D, Bosisio D (2013) Sulphurous thermal water increases the release of the anti-inflammatory cytokine IL-10 and modulates antioxidant enzyme activity. Int J Immunopathol Pharmacol 26:633–646
Salgueiro M, García-Leiva JM, Ballesteros J, Hidalgo J, Molina R, Calandre EP (2013) Validation of a Spanish version of the revised fibromyalgia impact questionnaire (FIQR). Health Qual Life Outcomes 11:132
Theoharides TC, Tsilioni I, Arbetman L, Panagiotidou S, Stewart JM, Gleason RM, Russell IJ (2015) Fibromyalgia syndrome in need of effective treatments. J Pharmacol Exp Ther 355:255–263
Wolfe F, Clauw DJ, Fitzcharles M et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600–610
Wolfe F, Brähler E, Hinz A, Häuser W (2013) Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res 65:777–785
Woodman I (2013) Fibromyalgia: fibromyalgia—all in the brain? Nat Rev Rheumatol 9:565
Yunus MB (2008) Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum 37:339–352
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-Fernández, M.R., Calvo-Ayuso, N., Martínez-Reglero, C. et al. Efficacy of baths with mineral-medicinal water in patients with fibromyalgia: a randomized clinical trial. Int J Biometeorol 63, 1161–1170 (2019). https://doi.org/10.1007/s00484-019-01729-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-019-01729-7