Abstract
The aim of this randomized controlled single-blind study is to explore whether addition of mud-pack and hot pool treatments to patient education make a significant difference in short and mild term outcomes of the patients with fibromyalgia. Seventy women with fibromyalgia syndrome were randomly assigned to either balneotherapy with mud-pack and hot pool treatments (35) or control (35) groups. After randomization, five patients from balneotherapy group and five patients from control group were dropped out from the study with different excuses. All patients had 6-h patient education programme about fibromyalgia syndrome and were given a home exercise programme. The patients in balneotherapy group had heated pool treatment at 38 °C for 20 min a day, and mud-pack treatment afterwards on back region at 45 °C. Balneotherapy was applied on weekdays for 2 weeks. All patients continued to take their medical treatment. An investigator who was blinded to the intervention assessed all the patients before and after the treatment, at the first and the third months of follow-up. Outcome measures were FIQ, BDI and both patient’s and physician’s global assessments. Balneotherapy group was significantly better than control group at after the treatment and at the end of the first month follow-up assessments in terms of patient’s and physician’s global assessment, total FIQ score, and pain intensity, fatigue, non-refreshed awaking, stiffness, anxiety and depression subscales of FIQ. No significant difference was found between the groups in terms of BDI scores. It is concluded that patient education combined with 2 weeks balneotherapy application has more beneficial effects in patients with fibromyalgia syndrome as compared to patient education alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and aim of the study
Fibromyalgia syndrome is a chronic pain syndrome. The most prominent symptoms include widespread musculoskeletal pain, fatigue, stiffness, anxiety, depression, difficulties in the daily living activities and sleep disturbances. Its prevalence in the overall population is 2 %; it is more common in women with a prevalence rate of 3.4 % where it is only 0.5 % in men (Wolfe et al. 1995).
Several medications and non-pharmacological approaches are used to relieve the symptoms of fibromyalgia syndrome; however, its radical treatment is not known to date. Pharmacological treatment alternatives include analgesics, non-steroidal anti-inflammatory drugs, antidepressants and anti-epileptics. Patient education, exercise, hot and cold applications and balneotherapy are commonly used non-pharmacological, complementary treatments (Oral et al. 2013; Carville et al. 2008). Patient education (Eich et al. 2012) and exercise (Busch et al. 2007) are highly recommended non-pharmacological modalities in fibromyalgia. The results of recently published studies indicate that balneotherapeutic applications, such as immersions and mud-pack applications, are effective on the symptoms of fibromyalgia syndrome (Buskila et al. 2001; Evcik et al. 2002; Donmez et al. 2005; Ozkurt et al. 2012; Kesiktas et al. 2011; Fioravanti et al. 2007).
The aim of this study is to find out whether addition of mud-pack and hot pool treatments to patient education would be more beneficial for fibromyalgia patients in short and mild term.
Patients and methods
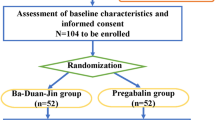
The study was designed as a single blind, randomized controlled study. The study was conducted at İstanbul University, İstanbul Medical Faculty, Department of Medical Ecology and Hydroclimatology. Two hundred and fifty-two fibromyalgia patients, who were registered at the outpatient clinic, were constituted the universe of the study. All registered patients were informed about the study and invited to participate in the study through telephone call. Three of the authors (AD, RE and NE) evaluated the volunteered patients regarding the study criteria and enrolled seventy female fibromyalgia patients conforming the inclusion criteria and gave their informed consent.
Inclusion criteria
The female patients should meet the American College of Rheumatology criteria for fibromyalgia and between 20 and 65 years of age (Wolfe et al. 2010). They should have had their usual treatment for at least2 months, without any modification. Participants have received sufficient explanation on the objectives, method and meaning of this study and grant their voluntary consent in writing.
Exclusion criteria
The patients should not have any medical condition that may prevent them from having balneotherapy and have had balneotherapy within past 1 year. The study project was approved by the local ethical committee of İstanbul Medical Faculty on 9th of February 2011.
All patients underwent physical examination. A series of laboratory tests including complete blood count, ESR, hepatic and renal function tests, thyroid hormone levels and urine analysis were ordered to reveal an additional pathology that may require to exclude the patients from the study.
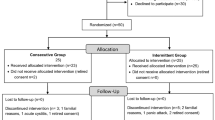
One of the authors (AD) randomized the patients, by using SPSS software generated randomization table, into two groups as balneotherapy group (35 patients) and controls (35 patients). Five patients in the balneotherapy group (3 of them because of time management problems, 1 of them because of her spouse’s illness, and 1 of them declared no reason) and 5 patients in the control group (4 of them declared that they wanted to go to the spa centre immediately, and 1 of them declared no reason) left the study after randomization.
A 6-h patient education programme on fibromyalgia syndrome was provided to all patients participating in the study. Patient education programme was delivered in 2 days, three interactive classes each day. First day’s programme included theoretical information on symptoms of fibromyalgia syndrome and prescription of individualized exercise programmes which includes stretching, relaxing, and posture exercises. At the second day, a psychologist thought the patients how stressing conditions may affect the disease and trained them how to coping with stress and on the use of relaxation techniques. Patient education programme was performed by two doctors, one physiotherapist and one psychologist.
Thirty-five patients in balneotherapy group had 10 heated pool baths and 10 mud-pack applications at the Department of Medical Ecology and Hydroclimatology. Temperature of the heated pool was 38 °C, and the duration of baths was 20 min. Immediately after the immersion, peloid packs at 45 °C were applied to backs of the patients for 20 min. The mud-pack used for application was a ready to use, single-use clay. Total mineralization of the mud was 3406 mg/L. The applications were performed for 2 weeks in weekdays.
Thirty-five patients at the control group were continued to have their treatment programme previously prescribed for their pain complaints due to fibromyalgia.
The same physician (RE), who was blinded to the treatment arms, evaluated all patients included in the study for four times: before the treatment, immediately after the treatment, and at the end of the 1st and the 3rd months after the treatment.
Evaluation parameters were Patient’s Global Assessment (PGASc) Investigator’s Global Assessment Score (IGASc), Fibromyalgia Impact Questionnaire (FIQ), pain, fatigue, non-refreshing sleep, stiffness, anxiety, depression and Beck Depression Index (BDI) (Burckhardt et al. 1991; Beck et al. 1961).
Statistical methods
Statistical evaluations were performed on intention-to-treat basis. Statistical calculations are performed using commercially available statistical software (SPSS ver.11.5, SPSS Inc., Chicago, USA). Assignment of the patients into the treatment arms is done by random assignment of patient admission numbers into two groups equally using the software’s grouping function. Demographic data are expressed as the mean and SD. Distribution of the data was evaluated using Shapiro-Wilk test. Normally distributed data were compared using Student’s t test. Friedman test and Mann Whitney U tests were used for multiple comparisons and two group comparisons, respectively, where the data distribution was non-parametric. Degree of freedom for alpha was set to 0.05 in all calculations. Calculated p values less than 0.05 were accepted as statistically significant.
Results
Seventy women with fibromyalgia who met the criteria according to the American College of Rheumatology were included in the study. Ten patients left the study after randomization (Fig. 1). The study was performed between February and December 2011. Balneotherapy and control groups were similar in terms of demographic features at the beginning of study (Table 1).
Significant improvements persisted up to the end of the 3rd month assessments in patient’s and investigator’s global assessment scores, total FIQ score, and pain intensity, fatigue, non-refreshed awaking, stiffness, anxiety and depression subscales of FIQ and BDI as compared to baseline values in balneotherapy group (Table 2).
Control group showed significant improvements in similar outcome measures except in patient’s global assessment scores and stiffness parameters (Table 3).
The differences from the baseline were calculated for each study variable in both groups. It was found that observed differences from the baseline are greater in balneotherapy group in pain, FIQ, tiredness, non-refreshing sleep, stiffness, anxiety, depression patient’s and investigator’s global assessment scores at the 15th day and at the end of the 1st month evaluation. No significant difference was found in BDI score (Table 4).
None of patients experienced thermal crisis that would require the cease of treatment. No side-effect was observed during treatment.
Discussion
The present study is a randomized controlled trial performed in an outpatient hospital setting using balneotherapy including mud packs, heated pool treatment and patient education in patients with fibromyalgia. In this study, balneotherapy group was found to be superior at the 15th day and at the end of the first month assessments regarding pain intensity, patient’s and investigator’s global assessment, fatigue, non-refreshing sleep, stiffness, anxiety, depression and FIQ scores. This superiority continued until the end of the third month assessment in non-refreshing sleep.
Randomized controlled trials and recent systematic review and meta-analysis reports indicate that balneotherapy has positive effects in fibromyalgia syndrome patients in terms of pain intensity, FIQ scores, patients’ and investigator’s global assessment (Falagas et al. 2009; Mc Veigh et al. 2008; Langhorst et al. 2009; Fraioli et al. 2013). However, authors of these studies are anonymously agreed that there is a need for more randomized controlled trials focused on this subject.
Patient education, heated pool treatment, balneotherapy and therapeutic exercises are advised in the section of non-pharmacologic treatment of FMS in the Guidelines for Fibromyalgia Treatment (Carville et al. 2008; Buckhardt et al. 2005; Arnold et al. 2012; Häuser et al. 2010). Therefore, these therapeutic approaches are included in the present study.
Our study results are in agreement with the findings stated in systematic reviews. As distinct from the other balneological studies on fibromyalgia, the present study is carried out at outpatient basis at the tertiary hospital environment rather than a spa centre. Therefore, the patients didn’t have to change their daily living routines. Both patient groups included in the study had similar patient education and home exercise programmes. We believe that observed improvements in control group are related to patient education and exercise programme. Additionally, the patients in balneotherapy group had heated pool treatment and mud pack applications.
Multidisciplinary treatment programmes including different types of non-pharmacological therapies are accepted more effective for fibromyalgia. Combination of spa therapy and patient education improves symptoms and quality of life patients with fibromyalgia (Zijlstra et al. 2005).
The effects of mud packs and heated pool help to relieve muscle spasm with thermal stimuli. Application of mud pack and heated pool decrease the muscle tone and increase the pain threshold at the nerve endings accordingly. Gate-control theory may explain pain-relieving effect of balneotherapy. Body surface of the patient is stimulated during immersion by temperature and hydrostatic pressure of hot water and sensation of pain decrease because of these stimuli, according to the theory. In addition to these effects, hot mineral water baths and mud-pack therapy increases plasma endorphin and cortisol levels, activation of the diencephalic-pituitary-adrenal axis, and decreases in plasma levels of several inflammatory mediators (IL-1, IL-6, PGE2, LTB4, TNF-α) (Fraioli et al. 2013; Cozzi et al. 1995; Ardiç et al. 2007; Fioravanti et al. 2011)
Considering both groups continued to live in their usual environment, observed superiority of the balneotherapy group in pain intensity, FIQ scores, patients’ and physicians’ global assessment may not be attributed to rest and environmental changes. It is better to argue that observed superiority may be due to heated pool and peloid pack applications. In the literature, it was frequently discussed whether environmental changes contribute to the positive effects of balneotherapy. Fibromyalgia patients may felt relaxed simply because they are away from their usual environment. Tubergen suggested that certain nonspecific variables of the spa environment such as environmental change, pleasant scenery, being in a non-competitive atmosphere with fellow patients, and the absence of work duties may be beneficial for patients with fibromyalgia (van Tubergen and Hidding 2002).
The present study has few limitations. The main limitation is the small number of patients included in the study, and one may criticize the short duration of follow-up period. Our budget hindered us from including more patients and to limit the follow-up period with 3 months.
In conclusion, balneotherapy with mud-pack and hot pool treatments is found to be effective in treating patients with fibromyalgia. Beneficial effects are observed both in short and mid-terms. Further randomized controlled studies should be designed to verify these results and to identify whether balneotherapy is cost-effective in fibromyalgia treatment.
References
Ardiç F, Ozgen M, Aybek H et al (2007) Effect of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446
Arnold B, Häuser W, Arnold M, Bernateck M, Bernardy K, Brückle W, Friedel E, Hesselschwerdt HJ, Jäckel W, Köllner V, Kühn E, Petzke F, Settan M, Weigl M, Winter (2012) Multicomponent therapy of fibromyalgia syndrome. Systematic review, meta-analysis and guideline. Schmerz 26(3):287–290
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Buckhardt CS, Goldenberg D, Crofford L et al (2005) Guideline for the management of fibromyalgia syndrome pain in adults and children. APS Clinical Practice Guideline Series. American Pain Society, Glenview
Burckhardt CS, Clark SR, Bennet RM (1991) The fibromyalgia impact questionnaire: development and validition. J Rheumatol 18:728–733
Busch AJ, Barber KA, Overend TJ, Peloso PMJ, Schachter CL (2007) Exercise for treating fibromyalgia syndrome. Cochrane Database of Syst Rev. Issue 4. Art. No.: CD003786. doi: 10.1002/14651858.CD003786.pub2
Buskila D, Shakra MA, Neumann L, Odes L, Shneider E, Flusser D, Sukenik S (2001) Balneotherapy for fibromyalgia at Dead Sea. Rheumatol Int 20:105–108
Carville SF, Arendt-Nielsen S, Bliddal H et al (2008) EULAR evidence based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis 67:536–541
Cozzi F, Lazzarin I, Todesco S, Cima L (1995) Hypotalamic pituary-adrenal axis dysregulation in healthy subjects undergoing mud-bath-applications. Arthritis Rheum 38:724–725
Donmez A, Karagulle MZ, Tercan N, Dinler M, Işsever H, Karagülle M, Turan M (2005) Spa therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26:168–172
Eich W, Häuser W, Arnold B, Bernardy K, Brückle W, Eidmann U, Klimczyk K, Köllner V, Kühn-Becker H, Offenbächer M, Settan M, von Wachter M, Petzke F (2012) Fibromyalgia syndrome. General principles and coordination of clinical care and patient education. Schmerz 26:268–275
Evcik D, Kızılay B, Gökcen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59
Falagas ME, Zarkadoulia E, Rafailidis PI (2009) The therapeutic effect of balneotherapy: evaluation of the evidence from randomised controlled trials. Int J Clin Pract 63:1068–1084
Fioravanti A, Perpignano G, Tirri G et al (2007) Effects of mud-bath treatment on fibromyalgia patients: a randomized clinical trial. Rheumatol Int 27:1157–1161
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8
Fraioli A, Grassi M, Mennuni G, Geraci A, Petraccia L, Fontana M, Conte S, Serio A (2013) Clinical researches on the efficacy of spa therapy in fibromyalgia. A systematic review. Ann Ist Super Sanita 49(2):219–229
Häuser W, Thieme K, Turk DC (2010) Guidelines on the management of fibromyalgia syndrome—a systematic review. Eur J Pain 14:5–10
Kesiktas N, Karagülle Z, Erdogan N, Yazıcıoglu K, Yılmaz H, Paker N (2011) The efficacy of balneotherapy and physical modalities on the pulmonary system of patients with fibromyalgia. J Back Musculoskelet Rehabil 24(1):57–65
Langhorst J, Musial F, Klose P, Hauser W (2009) Efficacy of hydrotherapy in fibromyalgia syndrome—a meta-analysis of randomized controlled clinical trials. Rheumatology 48:1155–1159
Mc Veigh JG, Mc Gaughey H, Hall M, Kane P (2008) The effectiveness of hydrotherapy in the management of fibromyalgia syndrome: a systematic review. Rheumatol Int 29:119–130
Oral A, Ilieva EM, Küçükdeveci AA, Varela E, Valero R, Berteanu M, Christodoulou N (2013) Generalised and regional soft tissue pain syndromes. The role of physical and rehabilitation medicine physicians. The European perspective based on the best evidence. A paper by the UEMS-PRM Section Professional Practice Committee. Eur J Phys Rehabil Med 49(4):535–549
Ozkurt S, Dönmez A, Zeki Karagülle M, Uzunoğlu E, Turan M, Erdoğan N (2012) Balneotherapy in fibromyalgia: a single blind randomized controlled clinical study. Rheumatol Int 32:1949–1954
van Tubergen A, Hidding A (2002) Spa and exercise treatment in ankylosing spondylitis: fact or fancy? Best Pract Res Clin Rheumatol 16(4):653–666
Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L (1995) The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38:19–28
Wolfe F, Clauw DJ, Fitzcharles M-A et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600–610
Zijlstra TR, van de Laar MAFJ, Bernelot Moens HJ, Taal E, Zakraoui L, Rasker JJ (2005) Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology 44:539–546
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bağdatlı, A.O., Donmez, A., Eröksüz, R. et al. Does addition of ‘mud-pack and hot pool treatment’ to patient education make a difference in fibromyalgia patients? A randomized controlled single blind study. Int J Biometeorol 59, 1905–1911 (2015). https://doi.org/10.1007/s00484-015-0997-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-015-0997-7