Abstract
Adipocytokines, including adiponectin, resistin, and visfatin may play an important role in the pathophysiology of osteoarthritis (OA). Spa therapy is one of the most commonly used non-pharmacological approaches for OA, but its mechanisms of action are not completely known. The aim of the present study was to assess whether a cycle of mud-bath therapy (MBT) influences the serum levels of adiponectin, resistin, and visfatin in patients with knee OA. As part of a prospective randomized, single blind-controlled trial evaluating the efficacy of MBT in knee OA, we included in this study 95 outpatients. One group (n = 49) received a cycle of MBT at the spa center of Chianciano Terme (Italy) in addition to the usual treatment, and one group (control group; n = 46) continued their regular care routine alone. Patients were assessed at basal time and at the end of the study (15 days) for clinical and biochemical parameters. Clinical assessments included spontaneous pain on a visual analog scale (VAS) score and the Western Ontario and McMaster Universities index (WOMAC) subscores for knee OA evaluated as total pain score (W-TPS), total stiffness score (W-TSS), and total physical function score (W-TPFS). Adiponectin, resistin and visfatin serum levels were assessed by enzyme immunoassay methods. At the end of the mud-bath therapy, serum adiponectin levels showed a significant decrease (p < 0.001), while no significant modifications were found in the control group at day 15. Serum resistin showed a significant decrease (p < 0.0001) in the MBT group at the end of the study and a significant increase in the control patients (p < 0.001). No significant modifications of visfatin were found in MBT. Furthermore, we tested the relationships between demographic and clinical parameters and adipocytokine concentrations measured in the MBT group at basal and at the end of the study. In conclusion, the present study shows that a cycle of MBT can modify serum levels of adiponectin and resistin but not the circulating levels of visfatin. In view of the recent evidences about the involvement of adiponectin and resistin in the pathogenesis and progression of OA, the decrease of these adipokines after mud-bath therapy may play a protective role in the course of the disease. However, it remains to be clarified which of the mechanisms of action of MBT may have determined the changes in serum levels of adiponectin and resistin that we observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common form of joint disease and the major contributor of disability in older people (Woolf and Pfleger 2003). Current treatment of OA includes pharmacological and non-pharmacological modalities. Spa therapy can represent a useful backup to pharmacological treatment or a valid alternative for patients who do not tolerate pharmacological treatments, but its mechanisms of action are not completely known (Hochberg et al. 2012).
Obesity constitutes major risk factors for OA presumably due to excessive joint loading (Oliveria et al. 1999). However, several studies demonstrated that obesity is also a risk factor for nonweight-bearing joints (Yusuf et al. 2010). Obesity is nowadays considered as a chronic low-grade inflammatory status, which is closely related to the release, by white adipose tissue, of many factors, most of them of pro-inflammatory nature, including classical cytokines such as interleukin (IL)-6, IL-1β, and tumor necrosis factor (TNF)-α, as well as adipokines, such as adiponectin, leptin, resistin, and visfatin (Fantuzzi 2005; Tilg and Moschen 2006).
Adiponectin has been found to improve insulin sensitivity and to have anti-atherogenic properties (Kadowaki et al. 2006; Ouchi et al. 2006). Interestingly, adiponectin has also been identified as a regulatory factor in inflammation and arthritis (Gomez et al. 2011). Adiponectin is detected in both synovial fluid and in plasma of OA patients (Presle et al. 2006) and has been reported to increase the production of metalloproteinases (MMPs), cytokines, and prostaglandin E2 (PGE2) by chondrocytes and synovial fibroblasts (Koskinen et al. 2011; Francin et al. 2014).
Resistin, a novel adipocyte-secreted hormone, has received attention for its involvement in insulin resistance in obesity and diabetes mellitus (Steppan et al. 2001). Recent research shows that human resistin is expressed in immune cells and possesses many characteristics of a pro-inflammatory cytokine (Senolt et al. 2007; Koskinen et al. 2014). Although the study regarding the role of resistin in OA is sparse, some studies showed its direct effect on cartilage matrix and cytokine production.
Visfatin also called pre-B cell colony-enhancing factor (PBEF) and nicotinamide phosphoribosyltransferase (Nampt) was originally identified as an adipokine exhibiting insulin-mimetic effects via binding to and activating the insulin receptor (Fukuhara et al. 2005). Visfatin has pro-inflammatory and immunomodulating functions (Sun et al. 2013) and manifested a pro-degradative effect in cartilage by increasing the synthesis of MMP-3, MMP-13, thrombospondin motifs (ADAMTS)-4, and ADAMTS-5 (Gosset et al. 2008; Hu et al. 2011; Laiguillon et al. 2014).
In a previous study, we showed that a cycle of mud-bath therapy (MBT) can modify serum levels of adiponectin in patients with knee OA (Fioravanti et al. 2011a, b). Partial contradictory data were observed in a recent pilot study conducted in healthy, young male by Shimodozono et al. (2012).
The objectives of this study were to assess whether a cycle of MBT influences the response of serum levels of adiponectin, resistin, and visfatin in patients with knee OA.
Materials and methods
Trial design
This is a part of a prospective randomized, single blind-controlled trial on the efficacy of MBT in patients with knee OA (Fioravanti et al. 2014a, b). The study protocol followed the Principles of the Declaration of Helsinki 1964 and later amendments and was approved by the Ethics Committee of Siena University Hospital (decision no. 340, 12th August 2010) and was registered on http://www.clinicaltrials.gov (NCT01538043).
Patients
As a part of a recently published randomized single blind-controlled clinical trial (Fioravanti et al. 2014a, b) on the efficacy of spa therapy in knee OA, we included 95 outpatients with primary bilateral knee OA fulfilling the American College of Rheumatology (ACR) criteria (Altman et al. 1986). Patients were recruited by the general practitioners between 1 December 2010 and 1 December 2011. Radiological staging was carried out using the Kellgren method (Kellgren and Lawrence 1957). Patients with a radiological score of I–III were included in the study. Exclusion criteria were severe comorbidity of the heart, lung, liver, cerebrum or kidney, acute illness, type 1 diabetes, varices, systemic blood disease, neoplasm, a body mass index (BMI) of >30 kg/m2 pregnancy, or nursing. In addition, for the purposes of this study, we excluded patients with history of type 2 diabetes mellitus, a history of instable weight, uncontrolled arterial hypertension, endocrine diseases affecting body weight, and/or use of medication affecting body weight within the prior 3 months and heavy smokers.
At the screening visit, blood samples were taken for erythrocyte sedimentation rate (ESR), electrolyte, creatinine, aspartate and alanine aminotransferases, and complete blood count analysis; urinalysis was also performed to verify the absence of exclusion criteria.
Written informed consent was obtained for all patients.
Treatment
Patients fulfilling the inclusion criteria were randomized to receive a cycle of mud-bath therapy in addition to the usual treatment (MBT group) or to continue their care routine alone (control group). The MBT group (n = 49) was treated with a combination of daily local mud-packs prepared with water from the Sillene Spring (Chianciano Terme, Italy) and baths in the same water. The sillene water is characterized by high sulfate, bicarbonate, calcium, and magnesium contents. Mud-packs were applied on both knees for 20 min at an initial temperature of 42 °C and with sillene water at 37 °C for 15 min in a bathtub for a total of 12 applications carried out over a period of 2 weeks. The control group (n = 46) continued their regular care routine alone (exercise, acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), symptomatic slow-acting drugs for OA (SYSADOA), and intra-articular hyaluronic acid).
Patients in both groups were advised to continue their established pharmacological and non-pharmacological treatments.
Outcome
Patients were assessed at basal time and at the end of the study (15 days) for clinical and biochemical parameters. Clinical assessments at each examination included spontaneous pain on a 0–100-mm visual analog scale (VAS) with 0 for the absence of pain (Jensen et al. 1986) and the Western Ontario and McMaster Universities index (WOMAC) subscores for knee OA evaluated as total pain score (W-TPS), total stiffness score (W-TSS), and total physical function score (W-TPFS) (Bellamy et al. 1998; Salaffi et al. 2003).
The WOMAC index consists of 24 questions (5 related to the amount of pain, 2 to stiffness, and 17 to physical function), and takes less than 5 min to complete (Bellamy 2009). For WOMAC, we used a 5-point Likert scale; the Likert scale may be more favorable over the VAS version (McConnell et al. 2001). The Likert version of the WOMAC rates each question on an ordinal scale of 0 to 4, with lower scores indicating lower levels of symptoms or physical disability (McConnell et al. 2001).
Blood samples (6 mL) were drawn from an antecubital vein with the patient in the supine position in the morning after an overnight fast. The blood was immediately centrifuged and serum was stored at −80 °C until analyzed.
Biochemical parameters including serum total cholesterol (mg/dL), triglycerides (mg/dL), high-density lipoprotein cholesterol (HDL-C; mg/dL), low-density lipoprotein cholesterol (LDL-C) (mg/dL) (Friedewald formula), glycemia (mg/dL), and high-sensitivity C-reactive protein (hs-CRP). Serum hs-CRP concentrations were measured using a highly sensitive immunonephelometric method (DADE Behring, Milan, Italy) on a BN II analyzer. The lower limit of detection was 0.175 mg/L (analytical sensitivity, 0.04 mg/L) (Punzi et al. 2012).
Serum adiponectin levels were determined with the enzyme-linked immunosorbent assay method using adiponectin (human) ELISA kit (AdipoGen Inc., South Korea). Sensitivity of samples was 100 pg/mL. Inter- and Intra-assay coefficients of variation were 2.8–5.5 and 2.9–3.8 %, respectively (Fioravanti et al. 2011a, b). Serum resistin levels were detected with the enzyme-linked immunosorbent assay method using resistin (human) Elisa kit (AdipoGen Inc., South Korea). Sensitivity of samples was 100 pg/mL. Inter- and Intra-assay coefficients of variation were 4.2–7.2 and 2.8–5.2 %, respectively (Cantarini et al. 2013).
Serum visfatin levels were detected with the enzyme-linked immunosorbent assay method using Nampt (isfatin/PBEF; human) ELISA kit (AdipoGen Inc. Korea). Sensitivity of samples was 30 pg/mL. Inter-assay and Intra-assay coefficients of variation were 4.7–7.2 and 2.3–9 %, respectively (Fioravanti et al. 2014a, b).
Statistical analysis
Values are given as mean ± standard deviation (SD). For all tests, a p value less than 0.05 was considered as statistically significant. Student’s or χ 2 tests were used to demonstrate the homogeneity of the two group variables in basal condition. The independent-samples t test was used to assess differences between groups whereas the paired-samples t test was used to assess the effect of treatment for clinical and biochemical parameters. Correlation analysis was performed using Pearson’s correlation coefficient or Spearman’s rank correlation coefficient.
For all analyses, SAS System v. 9.0 statistical software (Carry, USA Inc.) was used.
Results
Figure 1 provides the patient disposition throughout the study. Baseline demographic and clinical characteristics of the patients included in the study are given in Table 1. Comparison of the two groups showed no statistically significant differences in demographic and clinical characteristics except for sex and W-TPS. No significant differences between groups were found in serum total cholesterol, triglycerides, HDL-C, LDL-C, glycemia, and hs-CRP.
At the end of the treatment (2 weeks), a statistically significant reduction (p < 0.001) in spontaneous pain and in all WOMAC subscores was observed in the MBT group. In the control group, there were no significant differences after 2 weeks. The differences between the two groups were significant at day 15 (p < 0.001) (Table 2).
No significant modifications of serum total cholesterol, triglycerides, HDL-C, LDL-C, glycemia, and hs-CRP were found in both analyzed groups in the final observation (Table 3).
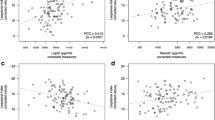
At the end of the mud-bath therapy, serum adiponectin levels showed a significant decrease (p < 0.001), whereas no significant modifications were found in the control group at day 15 (Fig. 2a). No significant differences were found between groups at basal time and at the end of the follow-up. Serum resistin showed a significant decrease (p < 0.0001) in MBT group at the end of the study and a significant increase in the control patients (p < 0.001) with a significant difference (p < 0.0001) between groups (Fig. 2b). Finally, serum visfatin was significantly (p < 0.05) higher in the control group than in MBT group at basal time and at the end of the follow-up. No significant modifications of visfatin were found after mud-bath therapy (Fig. 2c). The differences between the two groups were significant (p < 0.05) at basal time and after 2 weeks.
Furthermore, we tested the relationships between demographic and clinical parameters and adipocytokine and hs-CRP concentration measured in the MBT group at basal and at final time of the study (Table 4). Serum adiponectin levels were significantly and negative correlated with BMI and showed significant positive correlation with W-TSS at basal time, however, no significant correlation was found after mud-bath therapy. A significant negative correlation was observed between serum resistin and W-TPS and serum visfatin and W-TPFS at the end of the study (Table 4). Moreover, hs-CRP showed a significant positive correlation with W-TPFS after mud-bath therapy.
Finally, no changes whatsoever were made in terms of diet or physical activity levels, and no modifications in body weight were observed.
Discussion
Considerably strong and growing evidence supports the important role of various adipokines in OA (Hu et al. 2011; Conde et al. 2011). Adipokines were also viewed as a potential metabolic factor which link obesity to OA (Gabay and Berenbaum 2009).
Spa therapy is one of the most commonly used non-pharmacological approaches for OA in many European and Middle Eastern countries. It comprises a broad spectrum of therapeutic modalities including hydrotherapy, balneotherapy, mud-pack therapy, physiotherapy, and exercise (Verhagen et al. 2007). The mechanism by which mud-packs and/or balneotherapy improves the symptoms of rheumatic diseases is still not fully understood (Sukenik et al. 1999; Fioravanti et al. 2011a, b). In this study, we evaluated whether a cycle of mud-bath therapy has an effect on serum adiponectin, resistin and visfatin in patients with knee OA.
In agreement with our previous results (Fioravanti et al. 2011a, b), we showed a significant decrease of serum levels of adiponectin in patients treated with mud-bath therapy. Contradictory data were observed in a recent pilot study conducted by Shimodozono et al. (2012). The authors reported in seven healthy men, a slight, but not significant, increase immediately and 30 min after a single 10-min warm-water bath (WWB) at 41 °C with tap water or with WWB with inorganic salts and carbon dioxide (ISCO2). These differences might be due to the subjects studied (relatively healthy, young, lean, and male in this last study) and in modalities of bathing (duration of thermal stimulation and the substances used in the mineral water).
There is some evidence that adiponectin in skeletal joints may have pro-inflammatory effects and may be involved in cartilage degradation (Koskinen et al. 2011; Francin et al. 2014). Lago et al. (2008) recently demonstrated that adiponectin induced the expression of type-2 nitric oxide synthase (NOS) and stimulated IL-6, MMP-3, MMP-9, and monocyte chemo-attractant protein-1 (MCP-1) release. Then, the decrease of this adipokine can partially explain the beneficial effects of mud-bath therapy in OA patients. However, adiponectin presents metabolic properties as it increases insulin sensitivity, improves glucose metabolism and decreases plasma triglycerides, and has anti-atherogenetic actions. Furthermore, plasma levels of adiponectin are low in obese individuals and in those with cardiovascular disease (Matsuzawa 2005; Ouchi et al. 2006; Gonzalez-Gay et al. 2008); obesity and cardiometabolic syndrome are frequently associated with OA (Puenpatom and Victor 2009). Thus, it is important to study the effects of spa therapy on certain cardiovascular risk factors.
A significant reduction of serum resistin was shown in our knee patients after mud-bath therapy; on the contrary, in the control patients, we demonstrated a significant increase of this adipokine at the end of the follow-up. Resistin is a dimeric protein produced by adipocytes and macrophages and induces insulin resistance in mice (Steppan and Lazar 2002). Expression of resistin mRNA in human peripheral blood mononuclear cells (PBMCs) is increased by the pro-inflammatory cytokines IL-1, IL-6, and TNF (Kaser et al. 2003). Resistin can be detected locally in the synovium of inflamed joints in both rheumatoid arthritis (RA) and OA (Senolt et al. 2007; Koskinen et al. 2014). Furthermore, resistin increased expression of MMP-1, MMP-13, and ADAMTS-4 in human articular chondrocytes and stimulates proteoglycan degradation, as well as inhibited the production of proteoglycan and type II collagen in mouse and human cartilage explants (Lee et al. 2009; Poonpet and Honsawek 2014). In addition, resistin can stimulate inflammatory cytokines, such as IL-6 and TNF-α, as well as PGE2 synthesis. For these reasons, a decrease of resistin might play some role in the pathogenesis and in the progression of OA.
Surprisingly, after mud-bath therapy, we did not show any modification of serum visfatin; nevertheless, our study or other currently available data were unable to identify the reason of this different result in comparison with adiponectin and resistin.
Finally, no significant correlation was found between serum adipokines and the other considered clinical parameters except for adiponectin and W-TSS at basal time, resistin and W-TPS, hs-CRP, and W-TPFS at the end of the study.
In conclusion, the present study shows that a cycle of mud-bath therapy can modify serum levels of adiponectin and resistin, but not the circulating levels of visfatin. In view of the recent evidences about the involvement of adiponectin and resistin in the pathogenesis and progression of OA, the decrease of these adipokines after mud-bath therapy may play a protective role in the course of the disease.
However, it remains to be clarified which of the mechanisms of action of mud-bath therapy may have determined the changes in serum levels of adiponectin and resistin that we observed. The mechanisms of action of mud-bath therapy are not fully understood. The net benefit is probably the result of a combination of factors, among which the mechanical, thermal, and chemical effects are most prominent (Sukenik et al. 1999; Fioravanti et al. 2011a, b).
The effects of thermal baths are partially related to temperature (Srámek et al. 2000). Furthermore, mud-bath therapy induces a neuroendocrine reaction, which causes an increase in serum levels of corticosteroids and catecholamines (Laatikainen et al. 1988; Cima et al. 1992) and a reduction in circulation levels of TNF-α and IL-1β (Bellometti et al. 1997, 2002). These effects of mud-bath therapy can explain the modifications of serum levels of adiponectin and resistin demonstrated by our study. In fact, the circulating levels of adiponectin and resistin are influenced by temperature (Puerta et al. 2002; Imbeault et al. 2009; Iwen et al. 2011; Jankovic et al. 2013), catecholamines (Goossens et al. 2008; Iwen et al. 2011), TNF-α, and IL-1β (Delaigle et al. 2004; Kaser et al. 2003).
Furthermore, the local application of heat, by causing an increase in the internal temperature of the knee, may determine a change in serum adipocytokine levels, probably due to localized production thereof (Presle et al. 2006). Nevertheless, our study and other currently available data do not identify any specific mechanism of action.
The present study has several limitations which warrant mention. First, we did not include a control group of healthy subjects. Second, we did not evaluate the possible long-term effects of mud-bath therapy. Finally, we measured total adiponectin levels, which included both low molecular weight (LMW) and high molecular weight (HMW) isoforms; however, only LMW has an anti-inflammatory effect (Fantuzzi 2005).
Further longitudinal studies are needed to clarify the potential effects of mud-bath therapy on adipokine levels.
Abbreviations
- OA:
-
Osteoarthritis
- IL-1β:
-
Interleukin-1β
- TNF-α:
-
Tumor necrosis factor-α
- MMPS :
-
Metalloproteinases
- PGE2:
-
Prostaglandin E2
- ADAMTS:
-
Thrombospondin motifs
- PBEF:
-
Pre-B cell colony-enhancing factor
- Nampt:
-
Nicotinalide phosphoribosyltransferase
- MBT:
-
Mud-bath therapy
- hs-CRP:
-
High-sensitivity C-reactive protein
- ACR:
-
American College of Rheumatology
- BMI:
-
Body mass index
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- SYSADOA:
-
Symptomatic slow-acting drugs for OA
- VAS:
-
Visual analog scale
- WOMAC:
-
Western Ontario and McMaster Universities index
- W-TPS:
-
Total pain score
- W-TSS:
-
Total stiffness score
- W-TPFS:
-
Total physical function score
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
References
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Bellamy N (2009) WOMAC osteoarthritis index: user guide IX. WOMAC, Queensland
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1998) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Bellometti S, Cecchettin M, Galzigna L (1997) Mud pack therapy in osteoarthrosis. Changes in serum levels of chondrocyte markers. Clin Chim Acta 268:101–106
Bellometti S, Galzigna L, Richelmi P, Gregotti C, Bertè F (2002) Both serum receptors of tumor necrosis factor are influenced by mud pack treatment in osteoarthrotic patients. Int J Tissue React 24:57–64
Cantarini L, Brucato A, Simonini G et al (2013) Leptin, adiponectin, resistin, visfatin serum levels and idiopathic recurrent pericarditis: biomarkers of disease activity? A preliminary report. Clin Exp Rheumatol 31:207–212
Cima L, Cozzi F, Giusti P, Guidetti G, Todesco S (1992) Neuroendocrin effects of a cycle of fangotherapy. Pharmacol Rhes 26(suppl 1):302
Conde J, Scotece M, Gómez R, Lopez V, Gómez-Reino JJ, Gualillo O (2011) Adipokines and osteoarthritis: novel molecules involved in the pathogenesis and progression of disease. Arthritis 2011:203901. doi:10.1155/2011/203901
Delaigle AM, Jonas JC, Bauche IB, Cornu O, Brichard SM (2004) Induction of adiponectin in skeletal muscle by inflammatory cytokines: in vivo and in vitro studies. Endocrinology 145:5589–5597
Fantuzzi G (2005) Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol 115:911–919
Fioravanti A, Cantarini L, Guidelli GM, Galeazzi M (2011a) Mechanisms of action of spa therapies in rheumatic diseases: what scientific evidence is there? Rheumatol Int 31:1–8. doi:10.1007/s00296-010-1628-6
Fioravanti A, Cantarini L, Bacarelli MR, de Lalla A, Ceccatelli L, Blardi P (2011b) Effects of spa therapy on serum leptin and adiponectin levels in patients with knee osteoarthritis. Rheumatol Int 31:879–882. doi:10.1007/s00296-010-1401-x
Fioravanti A, Adamczyk P, Pascarelli NA, Giannitti C, Urso R, Tołodziecki M, Ponikowska I (2014) Clinical and biochemical effects of a 3-week program of diet combined with spa therapy in obese and diabetic patients: a pilot open study. Int J Biometeorol
Fioravanti A, Bacaro G, Giannitti C, Tenti S, Cheleschi S, Guidelli GM, Pascarelli NA, Galeazzi M (2014) One year follow-up of mud-bath therapy in patients with bilateral knee osteoarthritis: a randomized, single-blind controlled trial. Int J Biometeorol [Accepted]
Francin PJ, Abot A, Guillaume C et al (2014) Association between adiponectin and cartilage degradation in human osteoarthritis. Osteoarthr Cartil 22:519–526. doi:10.1016/j.joca.2014.01.002
Fukuhara A, Matsuda M, Nishizawa M et al (2005) Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science 307:426–430
Gabay O, Berenbaum F (2009) Adipokines in arthritis: new kids on the block. Curr Rheumatol Rev 5:226–232
Gomez R, Conde J, Scotece M, Gomez-Reino JJ, Lago F, Gualillo O (2011) What’s new in our understanding of the role of adipokines in rheumatic diseases? Nat Rev Rheumatol 7:528–536
Gonzalez-Gay MA, Llorca J, Garcia-Unzueta MT et al (2008) High-grade inflammation, circulating adiponectin oncentrations and cardiovascular risk factors in severe rheumatoid arthritis. Clin Exp Rheumatol 26:596–603
Goossens GH, Jocken JW, van Baak MA, Jansen EH, Saris WH, Blaak EE (2008) Short-term beta-adrenergic regulation of leptin, adiponectin and interleukin-6 secretion in vivo in lean and obese subjects. Diabetes Obes Metab 10:1029–1038. doi:10.1111/j.1463-1326.2008.00856.x
Gosset M, Berenbaum F, Salvat C, Sautet A, Pigenet A, Tahiri K, Jacques C (2008) Crucial role of visfatin/pre-B cell colony enhancing factor in matrix degradation and prostaglandin E2 synthesis in chondrocytes: possible influence on osteoarthritis. Arthritis Rheum 58:1399–1409. doi:10.1002/art.23431
Hochberg MC, Altman RD, April KT, American College of Rheumatology et al (2012) Recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 64:465–474
Hu PF, Bao JP, Wu LD (2011) The emerging role of adipokines in osteoarthritis: a narrative review. Mol Biol Rep 38:873–878. doi:10.1007/s11033-010-0179-y
Imbeault P, Dépault I, Haman F (2009) Cold exposure increases adiponectin levels in men. Metabolism 58:552–559. doi:10.1016/j.metabol.2008.11.017
Iwen KA, Wenzel ET, Ott V et al (2011) Cold-induced alteration of adipokine profile in humans. Metabolism 60:430–437. doi:10.1016/j.metabol.2010.03.011
Jankovic A, Korac A, Buzadzic B et al (2013) Endocrine and metabolic signaling in retroperitoneal white adipose tissue remodeling during cold acclimation. J Obes 2013:937572. doi:10.1155/2013/937572
Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27:117–126
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 116:1784–1792
Kaser S, Kaser A, Sandhofer A, Ebenbichler CF, Tilg H, Patsch JR (2003) Resistin messenger-RNA expression is increased by proinflammatory cytokines in vitro. Biochem Biophys Res Commun 309:286–290
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502
Koskinen A, Juslin S, Nieminen R, Moilanen T, Vuolteenaho K, Moilanen E (2011) Adiponectin associates with markers of cartilage degradation in osteoarthritis and induces production of proinflammatory and catabolic factors through mitogen activated protein kinase pathways. Arthritis Res Ther 13:R184. doi:10.1186/ar3512
Koskinen A, Vuolteenaho K, Moilanen T, Moilanen E (2014) Resistin as a factor in osteoarthritis: synovial fluid resistin concentrations correlate positively with interleukin 6 and matrix metalloproteinases MMP-1 and MMP-3. Scand J Rheumatol 43:249–253. doi:10.3109/03009742.2013.853096
Laatikainen T, Salminen K, Kohvakka A, Pettersson J (1988) Response of plasma endorphins, prolactin and catecholamines in women to intense heat in a sauna. Eur J Appl Physiol Occup Physiol 57:98–102
Lago R, Gomez R, Otero M et al (2008) A new player in cartilage homeostasis: adiponectin induces nitric oxide synthase type II and pro-inflammatory cytokines in chondrocytes. Osteoarthr Cartil 16:1101–1109. doi:10.1016/j.joca.2007.12.008
Laiguillon MC, Houard X, Bougault C et al (2014) Expression and function of visfatin (Nampt), an adipokine-enzyme involved in inflammatory pathways of osteoarthritis. Arthritis Res Ther 16:R38. doi:10.1186/ar4467
Lee JH, Ort T, Ma K et al (2009) Resistin is elevated following traumatic joint injury and causes matrix degradation and release of inflammatory cytokines from articular cartilage in vitro. Osteoarthr Cartil 17:613–620. doi:10.1016/j.joca.2008.08.007
Matsuzawa Y (2005) Adiponectin: identification, physiology and clinical relevance in metabolic and vascular disease. Atheroscler Suppl 6:7–14
McConnell S, Kolopack P, Davis AM (2001) The Western Ontario and McMaster Universities Osteoarthritis index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 45:453–461
Oliveria SA, Felson DT, Cirillo PA, Reed JI, Walker AM (1999) Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology 10:161–166
Ouchi N, Shibata R, Walsh K (2006) Cardioprotection by adiponectin. Trends Cardiovasc Med 16:141–146
Poonpet T, Honsawek S (2014) Adipokines: biomarkers for osteoarthritis? World J Orthop 5:319–327. doi:10.5312/wjo.v5.i3.319
Presle N, Pottie P, Dumond H et al (2006) Differential distribution of adipokines between plasma and synovial fluid in patients with osteoarthritis. Contribution of joint tissues to their articular production. Osteoarthr Cartil 14:690–695
Puenpatom RA, Victor TW (2009) Increased prevalence of metabolic syndrome in individuals with osteoarthritis: an analysis of NHANES III data. Postgrad Med 121:9–20. doi:10.3810/pgm.2009.11.2073
Puerta M, Abelenda M, Rocha M, Trayhurn P (2002) Effect of acute cold exposure on the expression of the adiponectin, resistin and leptin genes in rat white and brown adipose tissues. Horm Metab Res 34:629–634
Punzi L, Ramonda R, Deberg M, Frallonardo P, Campana C, Musacchio E, Henrotin Y (2012) Coll2-1, Coll2-1NO2 and myeloperoxidase serum levels in erosive and non-erosive osteoarthritis of the hands. Osteoarthr Cartil 20:557–561. doi:10.1016/j.joca.2012.02.638
Salaffi F, Leardini G, Canesi B et al (2003) Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) osteoarthritis index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560
Senolt L, Housa D, Vernerova Z et al (2007) Resistin in rheumatoid arthritis synovial tissue, synovial fluid and serum. Ann Rheum Dis 66:458–463
Shimodozono M, Matsumoto S, Ninomiya K et al (2012) Acute effects of a single warm-water bath on serum adiponectin and leptin levels in healthy men: a pilot study. Int J Biometeorol 56:933–939. doi:10.1007/s00484-011-0502-x
Srámek P, Simecková M, Janský L, Savlíková J, Vybíral S (2000) Human physiological responses to immersion into water of different temperatures. Eur J Appl Physiol 81:436–442
Steppan CM, Lazar MA (2002) Resistin and obesity-associated insulin resistance. Trends Endocrinol Metab 13:18–23
Steppan CM, Bailey ST, Bhat S et al (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312
Sukenik S, Flusser D, Abu-Shakra M (1999) The role of spa therapy in various rheumatic diseases. Rheum Dis Clin N Am 25:883–897
Sun Z, Lei H, Zhang Z (2013) Pre-B cell colony enhancing factor (PBEF), a cytokine with multiple physiological functions. Cytokine Growth Factor Rev 24:433–442. doi:10.1016/j.cytogfr.2013.05.006
Tilg H, Moschen AR (2006) Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 6:772–783
Verhagen AP, Bierma-Zeinstra SM, Boers M et al (2007) Balneotherapy for osteoarthritis. Cochrane Database Syst Rev 17, CD006864
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
Yusuf E, Nelissen RG, Ioan-Facsinay A et al (2010) Association between weight or body mass index and hand osteoarthritis: a systematic review. Ann Rheum Dis 69:761–765
Competing interest statement
None.
Funding
This study was funded by Regione Toscana. This study sponsor did not participate in the study design, in the collection, analysis, or the interpretation of data.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Fioravanti, A., Giannitti, C., Cheleschi, S. et al. Circulating levels of adiponectin, resistin, and visfatin after mud-bath therapy in patients with bilateral knee osteoarthritis. Int J Biometeorol 59, 1691–1700 (2015). https://doi.org/10.1007/s00484-015-0977-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-015-0977-y