Abstract
Deficiency of Complement Factor H Related (CFHR) plasma proteins and Autoantibody Positive Hemolytic Uremic Syndrome (DEAP-HUS) is a subtype of atypical hemolytic uremic syndrome, known to be associated with significant morbidity. Its pathogenesis is linked to the production of IgG autoantibodies against complement factor H, a regulator of the alternative complement pathway. The binding of the autoantibodies to the C terminal of complement factor H interferes with its regulatory function, leading to increased activation of the alternative complement pathway and consequent endothelial cellular damage. Early diagnosis and initiation of appropriate therapy is reported to lead to favorable outcomes. Institution of plasma exchange therapy within 24 h of diagnosis has been shown to rapidly lower antibody levels, leading to clinical improvement. Adjunctive immunosuppression therapy suppresses antibody production and helps in maintaining long-term clinical remission of the disease. Available data advocates a treatment regimen that combines plasma therapy (preferably plasma exchange) and immunosuppression to halt disease process and sustain long-term disease remission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
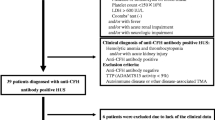
Hemolytic uremic syndrome (HUS) is a form of thrombotic microangiopathy (TMA) characterized by microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. The atypical form of the disease, aHUS, often refers to the non-Shiga toxin, non-streptococcal infection–associated HUS. Up to 60% of cases of aHUS have been linked to uncontrolled complement activation due to either genetic mutations in the alternative complement pathway or the presence of autoantibodies to complement factor H (CFH) [1, 2]. Autoantibodies to CFH are responsible for approximately 10% of cases [2], although prevalence greatly varies among countries, with up to 50% in India, 29% in the Korean population, and 5–25% in European cohorts [3, 4]. Gene mutations in the activators or regulators of the alternative complement pathway including CFH, membrane cofactor protein (CD46), factors I and B, C3 convertase components and C3, may occur [5,6,7,8]. Mutations in the thrombomodulin gene have been recently reported to also lead to aHUS [9]. The effect of these gene mutations on regulatory proteins leads to dysregulation of the alternative complement pathway, causing HUS.
A unique subtype of aHUS is the deficiency of CFHR plasma proteins and factor H autoantibody positive hemolytic uremic syndrome (DEAP–HUS), which is unique in that a deletion of genes encoding FH-related proteins is associated with the development of autoantibodies directed at CFH. These autoantibodies are found in 10–15% of aHUS patients and bind to the C-terminus of CFH, blocking CFH surface recognition and mimicking mutations found in the genetic form of CFH-mediated aHUS [10]. This binding effect results in defective CFH function and dysregulation of the alternative pathway, leading to endothelial cellular damage. DEAP-HUS tends to occur most frequently in teenagers but can also affect younger children and adults. It tends to present with a high frequency of gastrointestinal symptoms unlike other forms of aHUS. This makes it difficult to distinguish it from the typical Shiga toxin–related HUS at presentation. Extra-renal complications like seizures, pancreatitis, and hepatitis at presentation are also more frequent with DEAP-HUS. The disease tends to have a highly relapsing course with a high incidence of up to 50% of stage 5 chronic kidney disease reported in some cohorts. Higher anti-FH antibody titers at onset of disease, delay in the initiation of plasma exchange therapy, and low circulating free CFH levels are associated with poorer outcomes [11]. The mainstay of treatment of this disease involves prompt initiation of plasma exchange therapy and concurrent immunosuppression therapy to suppress antibody production. This review highlights the pathogenesis, treatment, and disease monitoring of patients with active DEAP-HUS.
Pathogenesis of DEAP-HUS
Complement factor H is the main regulator of the alternative complement pathway and exists in soluble form in the blood and on cell surfaces. The FH gene present on human chromosome 1 is part of the regulators of complement activation (RCA) gene cluster which encodes a single-chain serum glycoprotein. This factor H glycoprotein has a modular structure made up of an array of twenty short consensus repeat (SCR) domains [12,13,14]. These SCRs each have 20 homologous units of approximately 60 amino acid residues. The FH gene cluster consists of seven related genes that all encode soluble plasma proteins named CFH-related proteins 1 through 5 (CFHR1 to CFHR5) [14]. Emerging evidence suggests that these FH-related proteins have both activating and inhibiting regulatory properties [12]. CFHR1 is the most abundant protein and regulates the complement pathway by inhibiting the C3 and C5 convertases. In addition, CFHR1 blocks assembly and membrane insertion of the membrane attack complex (MAC). Full-length FH is a negative alternative pathway regulator that prevents amplification of the C3 and C5 convertases and acts as a cofactor for factor I (FI)–mediated conversion of C3b to inactive C3b (Fig. 1). Development of autoantibodies against complement FH occurs in about 6–10% of aHUS cases and leads to an acquired and transient deficiency of complement FH. These FH IgG autoantibodies frequently bind to the carboxy-terminal portion of full-length FH that contains the binding recognition site, thereby inhibiting cell surface protection from complement activity (Fig. 2). Recently, an association was found between the absence of CFHR1 and CFHR3 due to their gene deletion, and the presence of anti-FH autoantibodies [15,16,17,18,19,20]. The role of CFHR3 is so far unknown, but CFHR3 binds C3b and heparin, indicating a role in complement regulation [12].
Controlling the alternative-pathway amplification loop. The amplification (C3b feedback) loop is a positive-feedback cycle that consumes complement C3 to generate more enzyme and activation products; if unregulated, it cycles until all available C3 is consumed. Tight regulation is provided in the plasma by enzymes and cofactors that remove the C3 fragment C3b from the feedback cycle for breakdown into smaller fragments. As a consequence, the C3b feedback cycle normally operates at a very low rate (tick over). The balance between activation and regulation is disturbed in disease; a healthy balance can be restored by providing extra control (for example, increasing regulation, such as that provided by the complement regulatory protein factor H (FH), thereby increasing “feed out” from the amplification loop) or by preventing the formation of C3b in the feedback cycle (for example, by blocking convertase enzyme, thereby decreasing “feed in” to the amplification loop). Agents that target amplification of complement can have major therapeutic effects. Ba, non-catalytic fragment of FB; C3b–FH, complex between C3b and FH; CR1, complement receptor type 1; iC3b–FH, complex between inactive C3b and FH. B.Paul Morgan and Claire L Harris (2015) Complement, a target for therapy in inflammatory and degenerative diseases. Volume 14. Reprinted with permission
Anti-FH antibodies in atypical HUS. a Complement factor H (FH) regulates the alternative pathway of complement activation to prevent damage to self. It binds to glycosaminoglycans (GAGs) on cell surfaces through its central part (short consensus repeats SCRs 6–8) and its carboxyl terminus (SCRs 19–20). The amino-terminal part competes with factor B (FB) for binding to C3b and acts as a cofactor for factor I (FI) to inactivate C3b to iC3b, whereas the C terminus binds to C3b and its cleavage fragment C3d. FH also enhances the dissociation of the C3bBb complex. b In anti-FH-associated hemolytic uremic syndrome (HUS), anti-FH antibodies form immune complexes with FH and bind to multiple domains, thereby perturbing the interaction of FH with C3b, C3d and with GAG, ultimately reducing the ability of FH to confer protection against complement. c In C3 glomerulopathies, anti-FH antibodies bind to the amino terminus of FH, thereby perturbing the interaction of FH with C3b in the fluid phase. This perturbation reduces the ability of FH to function as a cofactor for factor I (FI)–mediated inactivation of C3b to iC3b. However, the binding of FH to C3d and GAG is preserved in C3 glomerulopathies. Reprinted with permission
Greater than 90% of the patients with DEAP-HUS have a homozygous chromosomal deletion of the CFHR1 and CFHR3 genes. Although homozygous deletions of the CFHR1/CFHR3 encoding segment are associated with DEAP-HUS in the majority of cases, heterozygous deletions have also been reported [20]. The frequency of homozygous CFHR1/CFHR3 deficiency is ~ 11–15% in aHUS and almost 100% in DEAP-HUS patients [20]. Homozygous CFHR1/CFHR3 deficiency has also been observed in the normal healthy Caucasian population at a frequency of about 2 to 5%. Family studies have demonstrated that only those deficient persons that have also generated autoantibodies to FH develop DEAP-HUS. Healthy family members who are homozygous deficient for CFHR1 and CFHR3 but who do not have autoantibodies to FH do not necessarily develop DEAP-HUS. The causative factor(s) and mechanisms that result in autoantibody production and development of DEAP-HUS are still unknown, but one possibility is that one (or both) of these molecules normally impairs the antibody production by B lymphocytes [21]. Therefore, in the absence of CFHR-1 and/or CFHR-3 proteins, autoantibody production by B lymphocytes may be dysregulated and inadequately controlled [21,22,23].
Treatment strategies and rationale
The treatment goal in DEAP-HUS is induction of clinical remission as fast as possible and maintenance of long-term remission without disease recurrence. Although plasma therapy and immunosuppression use remain the treatment approaches of choice, currently, no consensus exists on the optimal treatment regimen or the most effective immunosuppressive agents for the management of DEAP-HUS. Various treatment strategies instituted by clinicians have resulted in variable outcomes, and in some cases, similar treatment regimens have led to similar and sometimes different results, highlighting the possible contribution of other factors in shaping disease phenotype (Table 1). Moreover, every patient presents a unique clinical picture, as disease manifestation may be associated with specific genetic, biologic, and environmental predispositions [20]. Perhaps a better understanding of the pathophysiology of the disease and rationale for use of various therapies will inform the development of an ideal treatment regimen that produces consistent results. Treatment options and rationale for their use in DEAP-HUS management are hereby reviewed.
Plasmapheresis
Plasmapheresis refers to the extracorporeal separation of blood components into cells and plasma, and subsequent removal of the plasma component, which is replaced with donor fresh frozen plasma (FFP) or albumin (in patients allergic to FFP). The rationale for plasma exchange (PE) in DEAP-HUS treatment is its ability to rapidly remove the circulating CFH autoantibodies, leading to normalization or improvement in the regulatory function of CFH and stabilization of the alternative complement pathway. In their retrospective analysis, Khandelwal et al. showed a greater than 80% reduction of CFH autoantibody titer following 3–7 PE treatments [24]. The American Society for Apheresis (ASFA) strongly recommends the use of PE as first-line therapy in the treatment of CFH autoantibody–associated aHUS [23]. In the absence of PE therapy with FFP, plasma infusion (PI) may be utilized, in the hope that infusing enough CFH can override the blocking effect of the CFH autoantibodies. Clinical observations, however, suggest the superiority of PE therapy over PI. In a case series, 2 out of the 3 patients with DEAP-HUS who received PE as initial therapy experienced prompt recovery of kidney function [25]. The third patient who initiated treatment with PI required dialysis but subsequently recovered kidney function when PI was discontinued and replaced with PE. These patients also received immunosuppressive therapy, intended to suppress antibody production and help sustain disease remission. In another case series, all 3 patients with DEAP-HUS whose diagnosis was delayed due to a diarrheal prodrome and who initiated PE long past the 24-h window still recovered kidney function. In 2 of the patients, remission was induced and sustained without use of immunosuppression [26]. Other reports, however, showed adverse kidney outcomes with delayed PE therapy [22]. In their cohort of 138 children with CFH autoantibody–associated HUS, most of whom had CHHR1 homozygous gene deletion, independent risk factors for adverse kidney outcome included delay in initiation of PE and high autoantibody levels [4]. Moreover, multiple reports have shown disease relapse with withdrawal of PE therapy and rise of autoantibody levels [20, 25]. Although clear guidelines on the schedule and duration of PE therapy are currently lacking, a reasonable strategy would be to initiate daily treatments at diagnosis until antibody titers are significantly lowered, with concomitant initiation of immunosuppressive therapy and a subsequent weaning of plasma therapy.
Immunosuppression
The hallmark of disease activity in DEAP-HUS is the uncontrolled production of IgG autoantibodies which bind to the C-terminal recognition site of CFH, impairing its ability to bind C3b, thus leading to uncontrolled activation of the alternative complement pathway [27]. Removal of circulating antibodies and suppression of their production is key to clinical improvement and long-term disease remission [4, 28]. While PE acutely lowers antibody levels, ongoing antibody production is unopposed and disease recurrence is inevitable with discontinuation of plasma therapy and rebound of antibody titers. The inhibitory effect of immunosuppressant medications on antibody production is well established. Immunosuppressive medications act through a variety of mechanisms to suppress antibody production by their effect on B lymphocyte subsets [29]. Prednisone, cyclophosphamide (CYC), methotrexate (MTX), mycophenolate mofetil (MMF), and azathioprine (AZA) are shown to decrease B-1a lymphocytes by 60%, while cyclosporine (CsA) has little effect on B cell populations [29]. By the nature of its effect on B cell subpopulations, rituximab is effective in lowering CFH autoantibody titers, but these may rebound in some patients and predispose to disease relapse. Cyclophosphamide, however, has been shown to cause stable decrease in CFH autoantibodies and maintenance of disease remission in patients with CFH autoantibody–associated HUS [25, 30, 31]. Intravenous immunoglobulin (IVIG) has not been shown to be of benefit in DEAP-HUS management [20]. Immunosuppressive therapy allows for discontinuation of plasma therapy with low risk for disease relapse by maintaining suppressed autoantibody titers. In the largest cohort published so far, Sinha and colleagues demonstrated better kidney survival and long-term outcomes in patients who received combined therapies with plasma exchange and immunosuppression, underscoring the role of immunosuppression in maintaining low autoantibody titers long term [4]. In their review of therapy outcomes, Dragon Durey et al. showed a 35–43% risk of developing CKD stages 4–5 and death in patients whose treatment regimens comprised PE predominantly or supportive care, as compared with 10% risk in patients who received a combination of PE and immunosuppression (p < 0.0001) [32]. As regards immunosuppression regimens, various treatment protocols have produced heterogonous results (Table 1). While a first-line treatment regimen combining PEs, steroids, and 2–5 pulses of cyclophosphamide has demonstrated efficacy in inducing disease remission without need for long-term maintenance immunosuppression, regimens combining rituximab, mycophenolate mofetil, or azathioprine might require long-term immunosuppression to prevent disease relapse [10, 20, 25, 28, 33]. An international consensus statement has recommended treatment withdrawal after 1–2 years for maintenance immunosuppression protocols using mycophenolate mofetil, azathioprine, and steroids [34]. Prospective studies are needed to help determine the appropriate and optimal duration of immunosuppressive therapy and when it is safe to withdraw immunosuppression in patients with DEAP-HUS.
Complement C5 blockade
Cleavage of complement factor 5 into the potent anaphylatoxin and pro-inflammatory 5a and the membrane attack complex-forming 5b is responsible for the complement-mediated events in atypical HUS. In addition to its pro-inflammatory properties [35], the membrane attack complex C5b-9 disrupts cell membranes, leading to cell lysis. Eculizumab, a humanized chimeric monoclonal antibody, binds the terminal complement C5, inhibiting its cleavage by C5 convertase into C5a and C5b, thus terminating complement-mediated cellular injury [36, 37]. On September 23, 2011, eculizumab was approved by the FDA for the treatment of all patients with aHUS and its use has favorably transformed the clinical outcomes of patients with atypical HUS. Short- and long-term safety profiles have been established in the pediatric population [38, 39], although life-threatening meningococcal infections remain a serious risk associated with its use and guidelines for vaccination and antibiotic prophylaxis are currently in place [40, 41]. Limited data on the use of eculizumab as a sole agent in the management of DEAP-HUS and other CFH autoantibody–associated HUS is available. In their cohort of 17 pediatric patients with CFH autoantibody–associated HUS, Brocklebank et al. demonstrated the ability of eculizumab to induce and maintain long-term disease remission in 4 patients, in whom the drug was used as a sole agent without immunosuppression or plasma exchange [3]. In another report, a plasma-therapy-dependent patient with DEAP-HUS was initiated on eculizumab 4 years after initial presentation. After 2.5 years, plasma therapy was successfully discontinued but CFH autoantibody levels remained positive at low levels, suggesting complement activation but without disease relapse [42]. The risk of on-going alternative complement pathway activation due to persistence of CFH autoantibodies and the excessive cost associated with long-term eculizumab use should be considered when choosing it as a sole therapeutic agent in patients with DEAP-HUS. Treatment regimens combining other immunosuppressive medications are likely to be more cost effective while at the same time maintaining disease remission [28, 43, 44]. Giving its molecular weight of 148,000 Da, eculizumab is minimally removed on dialysis but can be removed by PE, and so timing should be carefully planned during intense PE therapy. Ravulizumab (Ultomiris), approved by the FDA 10/18/19 for the treatment of aHUS, is a long-acting complement C5 inhibitor that can be administered every 8 weeks and a convenient option for patients in whom this treatment is considered.
Novel therapies
A synthetic fusion protein, MFHR1, has recently been described as a potential therapeutic option for complement dysregulation disorders. Structurally, the MFHR1 is composed of the regulatory (inhibitory) components of CFH and CFHR1. The two N-terminal C5/C5b6 binding domains of CFHR1 are linked to the regulatory and surface recognition domains of CFH [45]. The resultant synthetic protein has been shown to produce a multitarget inhibition of the alternative complement pathway cascade. First, it accelerates the decay of the C3 convertase thereby inhibiting further alternative complement pathway activation. Secondly, it binds C5 convertase, preventing C5 cleavage and the generation of the proinflammatory C5a and the membrane attack complex C5b-9 [46]. When available for clinical use, MFHR1 will be a welcome and an important addition to the therapeutic options for DEAP-HUS. However, it remains unclear what the binding effect of CFH autoantibodies on MFHR1 is and whether this would hinder its effectiveness in the clinical context.
Monitoring complement pathway activity during therapy
Laboratory techniques are currently available for measuring activity of the complement system. Measurement of the total activity of the complement pathways as well as individual components of the complement system allows for disease characterization, assessment of disease severity, and response to complement targeted therapy. In DEAP-HUS patients undergoing therapy, routine monitoring of kidney function, lactate dehydrogenase (a marker of hemolysis and tissue breakdown), hemoglobin, reticulocyte, and platelet count is helpful in monitoring disease evolution and treatment effect. The treatment goal is to downregulate complement activation, preventing or limiting further tissue injury. The alternative and terminal pathways are the pathways of interest in DEAP-HUS, and their activity can be measured using functional assays, including hemolytic assays, immunoassays, or ELISA (Table 2) [47,48,49]. The 50% hemolytic complement (CH50) assay is the most commonly used method for measuring functional activity of the classical complement pathway, while the 50% hemolytic complement (AH50) assay measures activity of the alternative complement pathway. These hemolytic assays are an expression of the volume or dilution of the sample needed to produce 50% cell lysis [47, 50]. Low levels of CH50 or AH50 suggest deficiency or absence of components of the respective pathways [51,52,53] and require further evaluation, including measurement of the individual components of the complement system (Table 2). When both CH50 and AH50 are low, a deficiency of one or more of the components of the terminal pathway is suggested [53]. In DEAP-HUS therapy, AH50 levels should normalize with disease remission. Measurement of CFH autoantibody is helpful in assessing the effectiveness of PE and/or immunosuppressive therapy. Autoantibody levels are generally high during the acute phase of the disease and should decrease with appropriate therapy. In most cases, autoantibody levels remain positive but at lower titers during disease remission [25, 54]. The positive threshold for CFH autoantibody titers using ELISA is set at 100 AU/mL. In the largest cohort so far, mean autoantibody titers were 5411 ± 1388.1 AU/mL at disease onset and 844.3 ± 215.4 AU/mL at disease remission. At disease relapse, autoantibody titers rose back up to a mean of 3313.3 ± 817.5 AU/mL [4]. Similar autoantibody titer trends have been reported by other investigators [10, 25, 33]. There does not seem to be a consistent autoantibody titer at which sustained disease remission is guaranteed, and so at this time the authors are unable to recommend a specific titer at which withdrawal of immunosuppression would be considered safe. Moreover, autoantibody titers are known to fluctuate during disease remission [10]. Since eculizumab blocks complement C5, preventing the formation of the terminal complement complex, sC5b-9, quantification of the membrane attack complex should demonstrate a reduction in its titers with eculizumab use and other treatments [50].
Conclusion and future directions
DEAP-HUS is a rare subtype of aHUS associated with significant morbidity. Rapidly lowering plasma autoantibody levels at disease onset can halt excessive complement activation and induce disease remission. Combined therapies with PE and immunosuppression have been shown to be associated with favorable renal outcomes. Currently, no consensus exists on the optimal therapeutic approaches that yield consistent results. In line with available clinical guidelines on the management of aHUS, the authors recommend initiation of eculizumab (or PE where eculizumab is unavailable) within 24 h of presentation, to block activity of the terminal complement pathway. This is particularly important as results of investigations may take a few days to return (in our experience, laboratory turnaround time for anti-CFH autoantibody is as long as 7 days). As soon as the presence of anti-CFH autoantibodies is confirmed (and DEAP-HUS subsequently diagnosed), intense (daily) PE therapy should be commenced. Although current guidelines recommend at least 5 daily PEs at the initiation of treatment, fewer treatments, in association with immunosuppressive therapy, may be enough to induce prolonged remission with sustainably low antibody titers [23, 32]. Indeed, some investigators have stayed away from use of PE as first-line therapy and have used eculizumab with or without other immunosuppressants, with recovery of kidney function [3, 28]. Moreover, PE requires the placement of a central line, which carries the increased risk of infection and thrombosis. High-dose intravenous steroids or oral prednisolone should be initiated as part of initial therapy; readers may refer to Dragon-Durey et al. for dosing recommendations [32]. The authors feel eculizumab may be discontinued when PE is initiated along with other immunosuppression, but for clinicians who choose to continue eculizumab, concomitant PE and eculizumab dosing guidelines have been provided by Alexion [55]. The cost effectiveness of concomitant PE and eculizumab therapy should be weighed against clinical benefit. For patients who present with kidney failure, the authors propose the administration of intravenous cyclophosphamide after 5–7 PEs and repeat every 3–4 weeks for a total of 2–5 doses, as recommended by Dragon-Durey and colleagues [32]. Patients with less severe presentations and who do not require dialysis may be treated with eculizumab along with mycophenolate mofetil or azathioprine (thereby avoiding central placement), although this regimen may require prolonged therapy as previously mentioned. The authors favor the use of cyclophosphamide in both severe and less severe cases, as this regimen has the advantage of allowing a rapid withdrawal of immunosuppression therapy while maintaining long-term remission. However, the cytotoxic properties of cyclophosphamide, including gonadal toxicity, bone marrow suppression, infections, and risk of malignancy, must be born in mind. Different therapeutic approaches have been recommended by an international group of experts for various clinical scenarios [34]. Plasma autoantibody levels should be monitored at intervals during therapy, and since high autoantibody levels have been shown to correlate with disease activity, the aim should be to keep autoantibodies at a level that maintains disease remission for the individual patient. Obviously, this level would vary from patient to patient. Prospective studies can focus on identifying disease and patient-specific characteristics that determine treatment response and regimens that yield consistent results. A disease registry would allow for a study of treatment patterns and outcomes in patients with DEAP-HUS.
References
Noris M, Remuzzi G (2009) Thrombotic microangiopathy: what not to learn from a meta-analysis. Nat Rev Nephrol 5:186–188. https://doi.org/10.1038/nrneph.2009.28
Noris M, Remuzzi G (2009) Atypical hemolytic-uremic syndrome. N Engl J Med 361:1676–1687. https://doi.org/10.1056/NEJMra0902814
Brocklebank V, Johnson S, Sheerin TP, Marks SD, Gilbert RD, Tyerman K, Kinoshita M, Awan A, Kaur A, Webb N, Hegde S, Finlay E, Fitzpatrick M, Walsh PR, Wong EKS, Booth C, Kerecuk L, Salama AD, Almond M, Inward C, Goodship TH, Sheerin NS, Marchbank KJ, Kavanagh D (2017) Factor H autoantibody is associated with atypical hemolytic uremic syndrome in children in the United Kingdom and Ireland. Kidney Int 92(5):1261–1271. https://doi.org/10.1016/j.kint.2017.04.028
Sinha A, Gulati A, Saini S, Blanc C, Gupta A, Gurjar BS, Saini H, Kotresh ST, Ali U, Bhatia D, Ohri A, Kumar M, Agarwal I, Gulati S, Anand K, Vijayakumar M, Sinha R, Sethi S, Salmona M, George A, Bal V, Singh G, Dinda AK, Hari P, Rath S, Dragon-Durey MA, Bagga A, Indian HUS Registry (2014) Prompt plasma exchanges and immunosuppressive treatment improves the outcomes of anti-factor H autoantibody-associated hemolytic uremic syndrome in children. Kidney Int 85:1151–1160. https://doi.org/10.1038/ki.2013.373
Caprioli J, Noris M, Brioschi S, Pianetti G, Castelletti F, Bettinaglio P, Mele C, Bresin E, Cassis L, Gamba S, Porrati F, Bucchioni S, Monteferrante G, Fang CJ, Liszewski MK, Kavanagh D, Atkinson JP, Remuzzi G, International Registry of Recurrent and Familial HUS/TTP (2006) Genetics of HUS: the impact of MCP, CFH, and IF mutations on clinical presentation, response to treatment, and outcome. Blood 108:1267–1279. https://doi.org/10.1182/blood-2005-10-007252
Frémeaux-Bacchi V, Miller EC, Liszewski MK, Strain L, Blouin J, Brown AL, Moghal N, Kaplan BS, Weiss RA, Lhotta K, Kapur G, Mattoo T, Nivet H, Wong W, Gie S, Hurault de Ligny B, Fischbach M, Gupta R, Hauhart R, Meunier V, Loirat C, Dragon-Durey MA, Fridman WH, Janssen BJ, Goodship TH, Atkinson JP (2008) Mutations in complement C3 predispose to development of atypical hemolytic uremic syndrome. Blood 112:4948–4952. https://doi.org/10.1182/blood-2008-01-133702
Loirat C, Noris M, Fremeaux-Bacchi V (2008) Complement and the atypical hemolytic uremic syndrome in children. Pediatr Nephrol 23:1957–1972. https://doi.org/10.1007/s00467-008-0872-4
Geerdink LM, Westra D, van Wijk JA, Dorresteijn EM, Lilien MR, Davin JC, Kömhoff M, Van Hoeck K, van der Vlugt A, van den Heuvel LP, van de Kar NC (2012) Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol 27:1283–1291. https://doi.org/10.1007/s00467-012-2131-y
Delvaeye M, Noris M, De Vriese A, Esmon CT, Esmon NL, Ferrell G, Del-Favero J, Plaisance S, Claes B, Lambrechts D, Zoja C, Remuzzi G, Conway EM (2009) Thrombomodulin mutations in atypical hemolytic-uremic syndrome. N Engl J Med 361:345–357. https://doi.org/10.1056/NEJMoa0810739
Strobel S, Hoyer PF, Mache CJ, Sulyok E, Liu WS, Richter H, Oppermann M, Zipfel PF, Józsi M (2010) Functional analyses indicate a pathogenic role of factor H autoantibodies in atypical haemolytic uraemic syndrome. Nephrol Dial Transplant 25:136–144. https://doi.org/10.1093/ndt/gfp388
Puraswani M, Khandelwal P, Saini H, Saini S, Gurjar BS, Sinha A, Shende RP, Maiti TK, Singh AK, Kanga U, Ali U, Agarwal I, Anand K, Prasad N, Rajendran P, Sinha R, Vasudevan A, Saxena A, Agarwal S, Hari P, Sahu A, Rath S, Bagga A (2019) Clinical and immunological profile of anti-factor H antibody associated atypical hemolytic uremic syndrome: a nationwide database. Front Immunol 10:1282. https://doi.org/10.3389/fimmu.2019.01282
Cserhalmi M, Papp A, Brandus B, Uzonyi B, Józsi M (2019) Regulation of regulators: role of the complement factor H-related proteins. Semin Immunol 45:101341. https://doi.org/10.1016/j.smim.2019.101341
Zipfel PF (2009) Complement and immune defense: from innate immunity to human diseases. Immunol Lett 126:1–7. https://doi.org/10.1016/j.imlet.2009.07.005
Skerka C, Chen Q, Fremeaux-Bacchi V, Roumenina LT (2013) Complement factor H related proteins (CFHRs). Mol Immunol 56:170–180. https://doi.org/10.1016/j.molimm.2013.06.001
Skerka C, Hellwage J, Weber W, Tilkorn A, Buck F, Marti T, Kampen E, Beisiegel U, Zipfel PF (1997) The human factor H-related protein 4 (FHR-4). A novel short consensus repeat-containing protein is associated with human triglyceride-rich lipoproteins. J Biol Chem 272:5627–5634. https://doi.org/10.1074/jbc.272.9.5627
Skerka C, Horstmann RD, Zipfel PF (1991) Molecular cloning of a human serum protein structurally related to complement factor H. J Biol Chem 266:12015–12020
Skerka C, Kühn S, Günther K, Lingelbach K, Zipfel PF (1993) A novel short consensus repeat-containing molecule is related to human complement factor H. J Biol Chem 268:2904–2908
Skerka C, Zipfel PF (2008) Complement factor H related proteins in immune diseases. Vaccine 26(Suppl 8):I9–I14. https://doi.org/10.1016/j.vaccine.2008.11.021
Abarrategui-Garrido C, Martínez-Barricarte R, López-Trascasa M, de Córdoba SR, Sánchez-Corral P (2009) Characterization of complement factor H-related (CFHR) proteins in plasma reveals novel genetic variations of CFHR1 associated with atypical hemolytic uremic syndrome. Blood 114:4261–4271. https://doi.org/10.1182/blood-2009-05-223834
Dragon-Durey MA, Blanc C, Garnier A, Hofer J, Sethi SK, Zimmerhackl LB (2010) Anti-factor H autoantibody-associated hemolytic uremic syndrome: review of literature of the autoimmune form of HUS. Semin Thromb Hemost 36:633–640. https://doi.org/10.1055/s-0030-1262885
Buhlmann D, Eberhardt HU, Medyukhina A, Prodinger WM, Figge MT, Zipfel PF, Skerka C (2016) FHR3 blocks C3d-mediated coactivation of human B cells. J Immunol 197:620–629. https://doi.org/10.4049/jimmunol.1600053
Skerka C, Zipfel PF, Müller D, Micklisch S, Riedl M, Zimmerhackl LB, Hofer J (2010) The autoimmune disease DEAP-hemolytic uremic syndrome. Semin Thromb Hemost 36:625–632. https://doi.org/10.1055/s-0030-1262884
Schwartz J, Winters JL, Padmanabhan A, Balogun RA, Delaney M, Linenberger ML, Szczepiorkowski ZM, Williams ME, Wu Y, Shaz BH (2013) Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the Writing Committee of the American Society for Apheresis: the sixth special issue. J Clin Apher 28:145–284. https://doi.org/10.1002/jca.21276
Khandelwal P, Gupta A, Sinha A, Saini S, Hari P, Dragon Durey MA, Bagga A (2015) Effect of plasma exchange and immunosuppressive medications on antibody titers and outcome in anti-complement factor H antibody-associated hemolytic uremic syndrome. Pediatr Nephrol 30:451–457. https://doi.org/10.1007/s00467-014-2948-7
Boyer O, Balzamo E, Charbit M, Biebuyck-Gougé N, Salomon R, Dragon-Durey MA, Frémeaux-Bacchi V, Niaudet P (2010) Pulse cyclophosphamide therapy and clinical remission in atypical hemolytic uremic syndrome with anti-complement factor H autoantibodies. Am J Kidney Dis 55:923–927. https://doi.org/10.1053/j.ajkd.2009.12.026
Kim JJ, McCulloch M, Marks SD, Waters A, Noone D (2015) The clinical spectrum of hemolytic uremic syndrome secondary to complement factor H autoantibodies. Clin Nephrol 83:49–56. https://doi.org/10.5414/CN107777
Nozal P, Bernabéu-Herrero ME, Uzonyi B, Szilágyi Á, Hyvärinen S, Prohászka Z, Jokiranta TS, Sánchez-Corral P, López-Trascasa M, Józsi M (2016) Heterogeneity but individual constancy of epitopes, isotypes and avidity of factor H autoantibodies in atypical hemolytic uremic syndrome. Mol Immunol 70:47–55. https://doi.org/10.1016/j.molimm.2015.12.005
Hackl A, Ehren R, Kirschfink M, Zipfel PF, Beck BB, Weber LT, Habbig S (2017) Successful discontinuation of eculizumab under immunosuppressive therapy in DEAP-HUS. Pediatr Nephrol 32:1081–1087. https://doi.org/10.1007/s00467-017-3612-9
Salinas-Carmona MC, Perez LI, Galan K, Vazquez AV (2009) Immunosuppressive drugs have different effect on B lymphocyte subsets and IgM antibody production in immunized BALB/c mice. Autoimmunity 42:537–544. https://doi.org/10.1080/08916930903019119
Moore I, Strain L, Pappworth I, Kavanagh D, Barlow PN, Herbert AP, Schmidt CQ, Staniforth SJ, Holmes LV, Ward R, Morgan L, Goodship TH, Marchbank KJ (2010) Association of factor H autoantibodies with deletions of CFHR1, CFHR3, CFHR4, and with mutations in CFH, CFI, CD46, and C3 in patients with atypical hemolytic uremic syndrome. Blood 115:379–387. https://doi.org/10.1182/blood-2009-05-221549
Kwon T, Dragon-Durey MA, Macher MA, Baudouin V, Maisin A, Peuchmaur M, Fremeaux-Bacchi V, Loirat C (2008) Successful pre-transplant management of a patient with anti-factor H autoantibodies-associated haemolytic uraemic syndrome. Nephrol Dial Transplant 23:2088–2090. https://doi.org/10.1093/ndt/gfn063
Durey MA, Sinha A, Togarsimalemath SK, Bagga A (2016) Anti-complement-factor H-associated glomerulopathies. Nat Rev Nephrol 12:563–578. https://doi.org/10.1038/nrneph.2016.99
Sana G, Dragon-Durey MA, Charbit M, Bouchireb K, Rousset-Rouvière C, Bérard E, Salomon R, Frémeaux-Bacchi V, Niaudet P, Boyer O (2014) Long-term remission of atypical HUS with anti-factor H antibodies after cyclophosphamide pulses. Pediatr Nephrol 29:75–83. https://doi.org/10.1007/s00467-013-2558-9
Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, Coppo R, Emma F, Johnson S, Karpman D, Landau D, Langman CB, Lapeyraque AL, Licht C, Nester C, Pecoraro C, Riedl M, van de Kar NC, Van de Walle J, Vivarelli M, Frémeaux-Bacchi V, HUS International (2016) An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol 31:15–39. https://doi.org/10.1007/s00467-015-3076-8
Morgan BP (2016) The membrane attack complex as an inflammatory trigger. Immunobiology 221:747–751. https://doi.org/10.1016/j.imbio.2015.04.006
Brachet G, Bourquard T, Gallay N, Reiter E, Gouilleux-Gruart V, Poupon A, Watier H (2016) Eculizumab epitope on complement C5: progress towards a better understanding of the mechanism of action. Mol Immunol 77:126–131. https://doi.org/10.1016/j.molimm.2016.07.016
Wijnsma KL, Ter Heine R, Moes DJAR, Langemeijer S, Schols SEM, Volokhina EB, van den Heuvel LP, Wetzels JFM, van de Kar NCAJ, Brüggemann RJ (2019) Pharmacology, pharmacokinetics and pharmacodynamics of eculizumab, and possibilities for an individualized approach to eculizumab. Clin Pharmacokinet 58:859–874. https://doi.org/10.1007/s40262-019-00742-8
Licht C, Greenbaum LA, Muus P, Babu S, Bedrosian CL, Cohen DJ, Delmas Y, Douglas K, Furman RR, Gaber OA, Goodship T, Herthelius M, Hourmant M, Legendre CM, Remuzzi G, Sheerin N, Trivelli A, Loirat C (2015) Efficacy and safety of eculizumab in atypical hemolytic uremic syndrome from 2-year extensions of phase 2 studies. Kidney Int 87:1061–1073. https://doi.org/10.1038/ki.2014.423
Rondeau E, Cataland SR, Al-Dakkak I, Miller B, Webb NJA, Landau D (2019) Eculizumab safety: five-year experience from the Global Atypical Hemolytic Uremic Syndrome Registry. Kidney Int Rep 4:1568–1576. https://doi.org/10.1016/j.ekir.2019.07.016
Crew PE, McNamara L, Waldron PE, McCulley L, Christopher Jones S, Bersoff-Matcha SJ (2020) Antibiotic prophylaxis in vaccinated eculizumab recipients who developed meningococcal disease. J Inf Secur 80:350–371. https://doi.org/10.1016/j.jinf.2019.11.015
McNamara LA, Topaz N, Wang X, Hariri S, Fox L, MacNeil JR (2017) High risk for invasive meningococcal disease among patients receiving eculizumab (Soliris) despite receipt of meningococcal vaccine. MMWR Morb Mortal Wkly Rep 66(27):734–737. https://doi.org/10.15585/mmwr.mm6627e1
Noone D, Waters A, Pluthero FG, Geary DF, Kirschfink M, Zipfel PF, Licht C (2014) Successful treatment of DEAP-HUS with eculizumab. Pediatr Nephrol 29:841–851. https://doi.org/10.1007/s00467-013-2654-x
Diamante Chiodini B, Davin JC, Corazza F, Khaldi K, Dahan K, Ismaili K, Adams B (2014) Eculizumab in anti-factor h antibodies associated with atypical hemolytic uremic syndrome. Pediatrics 133:e1764–e1768. https://doi.org/10.1542/peds.2013-1594
Dedhia P, Govil A, Mogilishetty G, Alloway RR, Woodle ES, Abu Jawdeh BG (2017) Eculizumab and belatacept for de novo atypical hemolytic uremic syndrome associated with CFHR3-CFHR1 deletion in a kidney transplant recipient: a case report. Transplant Proc 49:188–192. https://doi.org/10.1016/j.transproceed.2016.11.008
Top O, Parsons J, Bohlender LL, Michelfelder S, Kopp P, Busch-Steenberg C, Hoernstein SNW, Zipfel PF, Häffner K, Reski R, Decker EL (2019) Recombinant production of MFHR1, a novel synthetic multitarget complement inhibitor, in moss bioreactors. Front Plant Sci 10:260. https://doi.org/10.3389/fpls.2019.00260
Michelfelder S, Fischer F, Wäldin A, Hörle KV, Pohl M, Parsons J, Reski R, Decker EL, Zipfel PF, Skerka C, Häffner K (2018) The MFHR1 fusion protein is a novel synthetic multitarget complement inhibitor with therapeutic potential. J Am Soc Nephrol 29:1141–1153. https://doi.org/10.1681/ASN.2017070738
Prohászka Z, Nilsson B, Frazer-Abel A, Kirschfink M (2016) Complement analysis 2016: clinical indications, laboratory diagnostics and quality control. Immunobiology 221:1247–1258. https://doi.org/10.1016/j.imbio.2016.06.008
Kerboua KE, Djenouhat K (2020) Semi-solid phase assay for the alternative complement pathway activity assessment (AP100). J Immunoassay Immunochem 41:144–151. https://doi.org/10.1080/15321819.2019.1696819
Jaskowski TD, Martins TB, Litwin CM, Hill HR (1999) Comparison of three different methods for measuring classical pathway complement activity. Clin Diagn Lab Immunol 6:137–139
Puissant-Lubrano B, Puissochet S, Congy-Jolivet N, Chauveau D, Decramer S, Garnier A, Huart A, Kamar N, Ribes D, Blancher A (2017) Alternative complement pathway hemolytic assays reveal incomplete complement blockade in patients treated with eculizumab. Clin Immunol 183:1–7. https://doi.org/10.1016/j.clim.2017.06.007
Costabile M (2010) Measuring the 50% haemolytic complement (CH50) activity of serum. J Vis Exp 37:1923. https://doi.org/10.3791/1923
Kirschfink M, Mollnes TE (2003) Modern complement analysis. Clin Diagn Lab Immunol 10:982–989. https://doi.org/10.1128/cdli.10.6.982-989.2003
Shih AR, Murali MR (2015) Laboratory tests for disorders of complement and complement regulatory proteins. Am J Hematol 90:1180–1186. https://doi.org/10.1002/ajh.24209
Lee BH, Kwak SH, Shin JI, Lee SH, Choi HJ, Kang HG, Ha IS, Lee JS, Dragon-Durey MA, Choi Y, Cheong HI (2009) Atypical hemolytic uremic syndrome associated with complement factor H autoantibodies and CFHR1/CFHR3 deficiency. Pediatr Res 66:336–340. https://doi.org/10.1203/PDR.0b013e3181b1bd4a
Alexion. Highlights of prescribing information (2019) https://alexion.com/Documents/Soliris_USPI.pdf. Accessed 4/2/20
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iorember, F., Nayak, A. Deficiency of CFHR plasma proteins and autoantibody positive hemolytic uremic syndrome: treatment rationale, outcomes, and monitoring. Pediatr Nephrol 36, 1365–1375 (2021). https://doi.org/10.1007/s00467-020-04652-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04652-x