Abstract
Background
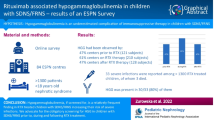
Rituximab (RTX) is efficient in steroid-dependent nephrotic syndrome (SDNS) in pediatric and adult patients. The aim of this study is to describe hypogammaglobulinemia as a side effect of RTX treatment.
Methods
All pediatric patients (< 18 years old) of four French pediatric nephrology centers who received RTX for SDNS between 2010 and 2015 have been included. Clinical and biological data have been analyzed retrospectively before, during, and after RTX treatment. Hypogammaglobulinemia was defined as an IgG level < − 2 standard deviations for patient age.
Results
A total of 107 pediatric patients have been included, 65.9% were boys, median age at nephrotic syndrome diagnosis was 3.1 interquartile range [IQ 2.24–5.45] years and age at RTX introduction was 11.7 [IQ 8.6–14.2] years. Twenty-one patients had hypogammaglobulinemia before the initiation of RTX. Of the patients, 25/86 had at least one hypogammaglobulinemia during B cell depletion or after B cell recovery while IgG levels at initiation were normal with a persisting hypogammaglobulinemia for 13 patients 1 year after B cell recovery. Patients who developed hypogammaglobulinemia were younger at RTX initiation with a median age of 8.2 years [IQ 6.3–12.4]. Among all the 46 patients with hypogammaglobulinemia during follow-up, 13 had a concomitant infection.
Conclusions
Hypogammaglobulinemia is a frequent complication of RTX treatment in younger children treated for SDNS. The use of RTX in children has to be carefully evaluated and their clinical and biological follow-up should be adapted to the age-dependent risk profile for hypogammaglobulinemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rituximab (RTX) is an anti-CD20 monoclonal antibody, which binds to the CD20 antigen and leads to immediate destruction of the CD20 expressing cell. B cell depletion after RTX injection is usually complete and lasts in most cases from 2 to 8 months [1]. In the treatment of steroid-dependent nephrotic syndrome (SDNS), a single RTX course has been proposed, but long-term remission rate after the first 6 months post RTX injection decreases considerably and is not satisfactory [2]. Disease relapse is presumably related to B cell recovery and particularly the recovery of switched memory B cells was also strongly predictive of relapse [3]. Therefore, either repeated RTX injections after a fixed time interval or RTX re-injection depending on B cell recovery have been successfully performed [4,5,6].
At treatment onset, immunoglobulin levels are generally not affected by RTX because CD20 is expressed on pre-B cells and mature B cells but not on stem cells or mature plasma cells. However, prolonged hypogammaglobulinemia after RTX therapy has recently been reported for adults with SDNS [7] and for the treatment of other autoimmune diseases without nephrotic-range proteinuria [8,9,10].
In SDNS children, we performed a previous monocentric study in 12 patients, in which RTX treatment seemed to aggravate pre-existing hypogammaglobulinemia, whereas immunoglobulin G (IgG) levels were normal in patients without pre-existing hypogammaglobulinemia [11]. In another monocentric retrospective study by Fujigana et al. in 60 children with SDNS [12], 16.7% had low IgG levels at 6 months after a single dose of RTX and the incidence of hypogammaglobulinemia in patients with pre-existing low IgG levels was significantly higher than that in patients with normal baseline IgG levels. However, the true frequency of hypogammaglobulinemia is unknown due to the lack of prospective studies in different patient cohorts and the clinical significance remains controversial. Indeed, some patients have recurrent infections while others are asymptomatic. Here, we report hypogammaglobulinemia, and concomitant infections before, during, and after RTX in children with “difficult-to-treat” SDNS and their relation to RTX dose, time of B cell depletion and patient age.
Patients and methods
Study population
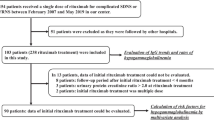
All pediatric patients (< 18 years old) who received a first course of RTX for SDNS between January 2010 and December 2015 in four pediatric nephrology departments were included. We did not include steroid-resistant patients which were defined as persistent nephrotic proteinuria despite 30 days of oral prednisone at 60 mg/m2 and 3 intravenous (IV) methylprednisolone pulses of 1 g/1.73 m2. RTX infusion was performed during remission phases with negative proteinuria. Initial RTX course was performed as one to two infusions of 375 mg/m2. CD19 depletion was confirmed by flow cytometry assay after RTX infusion. Where B cells reconstituted (CD19-positive cells > 10 mm3), a repeat RTX infusion was performed. From the medical records, we collected retrospectively clinical data, including date of birth, gender, date of idiopathic nephrotic syndrome (INS) diagnosis, date of first RTX injection, number of RTX injections, cumulative RTX dose, total B cell depletion duration, number of relapses prior to, during, and after RTX treatment, oral immunosuppressive treatments, intravenous immunoglobulin (IVIg) supplementation, date and characteristics of clinical infections concurrent with a low IgG level.
We collected biological data, including immunoglobulin (IgG, IgA, and IgM) levels before the first RTX injection for all patients, date and level of IgG during and after RTX treatment. IgG levels were collected during remission while serum albumin level was > 30 g/L. All patients had a follow-up of at least 6 months after the first RTX injection.
Methods
Our primary outcome was the first episode of hypogammaglobulinemia during follow-up, defined as IgG < -2 standard deviations (SD) for age. We used the following normal values depending on age [13, 14]: 0–2 years, IgG < 3.5 g/L; 2–6 years, IgG < 4.0 g/L; ≥ 6 years, IgG < 5.0 g/L. Infections were considered as concomitant with hypogammaglobulinemia when the diagnosis of infection was made in a patient with concomitant low IgG serum levels. Patients’ characteristics are presented as median and interquartile range (IQ) for continuous variables, and counts and percent for categorical variables. Results were compared by Wilcoxon-analysis and the χ2 test using SAS 9.4 and a p value less than 0.05 was considered statistically significant.
Results
Patients’ characteristics
Patients’ characteristics at the time of RTX treatment are presented in Table 1. The median follow-up was 4.02 years [IQ 2.7–5.8] after the first RTX infusion and only 6/107 patients had less than 18 months follow-up. One hundred seven patients, 37 (34.5%) girls, treated by RTX for SDNS were included. The median age of the study population at the time of INS diagnosis was 3.1 years [IQ 2.2–5.4]. Prior to RTX, all patients received other immunosuppressive drugs aside from oral steroids, including levamisole (19.6%), mycophenolate mofetil (MMF) (74.8%), cyclophosphamide (29%), and calcineurin inhibitors (86.9%). All patients had “difficult-to-treat” SDNS and were treated with the first RTX dose at a median age of 11.7 years [IQ 8.6–14.2]. The median time range on B cell depletion in our cohort was 16.9 months [IQ 6.0–24.0] with 1500 mg/m2 [IQ 1125–1875] median cumulative RTX dose and median CD19 depletion period was 19.8 months [IQ 13.2–26.4]. Ninety-six patients required repeat infusions of RTX, 11 patients only received a single infusion because of different RTX treatment protocols in the participating centers
Patients with hypogammaglobulinemia
During follow-up, including the time before and after RTX initiation, 46/107 (43%) patients had at least one episode of hypogammaglobulinemia detected (Fig. 1). Twenty-one patients had hypogammaglobulinemia before RTX, with a median IgG level of 4.6 g/L [IQ 3.6–4.8] (Table 1). Hypogammaglobulinemia persisted in 12/21 patients during RTX treatment and in 8 patients 1 year after B cell recovery. Among the 82 patients with a normal IgG level at RTX initiation, 25/82 developed hypogammaglobulinemia after RTX initiation, with a persisting hypogammaglobulinemia in 13/25 patients and a lower IgG level 1 year after B cell recovery compared to RTX initiation (median IgG level 4.4 g/L [IQ 3.8–5.8] vs. 6.1 [5.5–6.7]). Their first episode of hypogammaglobulinemia occurred after a median of 15 months [IQ 7.5–36.2] post RTX initiation.
There is no difference between patients with hypogammaglobulinemia before RTX or during RTX related to relapse number or immunosuppressive treatment prior RTX, gender, and age at diagnosis (Table 1). Patients with hypogammaglobulinemia after RTX initiation were younger at first RTX infusion than those with normal IgG levels during follow-up: 8.2 years [IQ 6.3–12.4] and 13.3 years [IQ 9.9–14.9] respectively (p < 0.001) (Table 1). The percentage of patients with low IgG levels after RTX onset decreased significantly in those who had a RTX onset after the age of 7 years (Fig. 2).
Percentage and number of patients with hypogammaglobulinemia in relation to patients’ age among those with normal IgG levels at rituximab onset (N = 86). RTX, rituximab. Light gray bar = patients with normal IgG levels. Dark gray bar = patients with hypogammaglobulinemia after rituximab initiation and relative percentage
The percentage of patients with concomitant oral immunosuppressive treatment during B cell depletion was not different in patients with (32.6%) or without hypogammaglobulinemia (29.5%), neither was the type of oral immunosuppression, with 64.3% and 55.5% of patients on calcineurin inhibitors, respectively.
Among 63 patients without relapse during the RTX treatment, 13 (20.6%) developed hypogammaglobulinemia after RTX initiation vs. 4/29 patients (13.8%) with 1 or 2 relapses and 8/16 (50%) with 3 or more relapses during RTX treatment.
Clinical and biological data during RTX treatment
There was no difference in cumulative RTX dose (1500 mg/m2 [IQ 1125–2250] vs 1500 mg/m2 [IQ 750–1875]) or in CD19 depletion period (20.2 months [IQ 16.3–36.0] vs.17.9 months [IQ 9.1–24.1]) in patients with vs. without hypogammaglobulinemia during RTX treatment (Table 1).
When we divided the patients into three age groups at RTX initiation (Fig. 3) (17 patients in the group “0–6 years,” 49 in the group “7–12 years,” and 41 in the group “≥ 13 years”), there was a further decline of IgG levels in the “0–6 years group” compared to the two other groups. At the end of follow-up, the median IgG serum levels were lower in the “0–6 years group” 4.76 g/l [IQ 4.1–8.2] vs. 6.16 g/l [4.3–8.9] and 6.37 g/l [IQ 5.3–9.4]) for two other groups respectively. Moreover, 8/17 (47%) patients who were under 7 years old at RTX onset still had hypogammaglobulinemia 1 year after RTX discontinuation and B cell recovery. Among the older patients, the number of persistent hypogammaglobulinemia was 13/49 (30.4%) for “7–12 years” and 3/41 (7.3%) for “≥ 13 years.” The cumulative RTX doses were similar in the “0–6 years” group compared to the two other age groups (1875 mg/m2 [IQ 1500–2625] vs. 1500 [IQ 1125–1875] vs. 1500 [IQ 750–1875]) and so was the respective B cell depletion periods (22.1 months [IQ 11.3–25.2] vs. 19.6 [IQ 14.9–26.4] vs. 18.7 [IQ 11.2–28.7]).
Changes of IgG plasma levels at rituximab initiation and over time. Median IgG levels in g/l and interquartile range are given at the time of rituximab perfusion and during the B cell depletion period (M0 to M18) and 1 year after B cell recovery (M12 post RTX) according to age at rituximab initiation (0–6 years ; 7–12 years and ≥ 13 years). RTX, rituximab
Concomitant infections during rituximab treatment
In patients with hypogammaglobulinemia, 13/46 (28%) concomitant infections during one episode of hypogammaglobulinemia were reported (Fig. 1). Among these 13 patients, 7 required hospitalizations and were treated by intravenous antibiotics. Infections were 5 pneumonias, 1 fulminant viral myocarditis (already described elsewhere [15]), 1 viral meningitis, 4 ENT infections (recurrent otitis in 2 patients), 1 varicella, and 1 EBV infection. All these patients received IVIg supplementation as part of treatment during their acute infectious episode. Among 46 patients who had hypogammaglobulinemia, those with concomitant infections were younger at RTX initiation with a median age of 6.5 years [5.2–14.6] vs. 10.3 [7.2–12.4] in those without infections. Whereas there was no difference in cumulative RTX dose (1875 mg/m2 [IQ 1500–2250] and 1875 mg/m2 [QI 1500–2625]) respectively or B cell depletion period (24.0 months [IQ 17.3–35.8] and 24.0 months [IQ 13.5–27.8]) (Table 2).
Discussion
Among all RTX-treated SDNS patients in our study, 43% had at least one episode of hypogammaglobulinemia, and more than half of them developed hypogammaglobulinemia after RTX initiation. To our knowledge, this is the first study on hypogammaglobulinemia in a large cohort of RTX-treated pediatric patients with SDNS and to report a higher risk for hypogammaglobulinemia if RTX was started in younger patients. This confirms a very recent report by Fujigana et al. in which 4 out of 6 children developed hypogammaglobulinemia with a median age of 4.2 years at RTX initiation [16].
Our data suggest that younger age is a risk factor for hypogammaglobulinemia during RTX treatment, even if baseline IgG levels were in the normal range at treatment onset. Further, patients with concomitant infections during hypogammaglobulinemia had a median age of six years at RTX initiation, whereas those without concomitant infection had a median age of 10 years. On the other hand, in our cohort, RTX seems to be a safe treatment for older SDNS pediatric patients, without an increased risk for hypogammaglobulinemia and infection compared to adults.
Patients with hypogammaglobulinemia
The incidence of hypogammaglobulinemia in our cohort was in line with data reported in previous studies on RTX treated SDNS patients: Those with low baseline IgG levels had a higher risk for persistence or aggravation of hypogammaglobulinemia during the RTX treatment [11, 12]. Similarly, in patients with multi-system autoimmune diseases, IgG levels at the time of the first RTX infusion were correlated with IgG concentration after the RTX treatment period [8, 9, 17]. Moreover, in adults, data from the French Autoimmunity and RTX registry (AIR registry) found that hypogammaglobulinemia (< 6 g/L) at baseline has clinical consequences and was an important risk factor for severe infections during a 12-month follow-up post RTX with an odds ratio of 4.9 [18].
The origin of hypogammaglobulinemia in patients before RTX treatment is difficult to determine and may have several explanations: (i) An underlying immune dysfunction may be present at baseline. (ii) The immune dysfunction may be a long-lasting effect of orally administered immunosuppression before RTX initiation. (iii) Hypogammaglobulinemia secondary to IgG urinary loss during relapses before RTX initiation. The time interval between the last relapse and RTX initiation may impact initial post RTX IgG level.
Patients with initial hypogammaglobulinemia and infections after RTX may have subclinical immune deficiency or dysfunction, which might be unmasked or exacerbated by RTX as our results may suggest in younger children with low IgG at baseline and a rapid decrease following RTX treatment. Thus, evaluating immunoglobulin level changes after obtaining a remission and after a longer relapse free period may help to identify patients with underlying immune deficiency and/or humoral dysfunction.
Clinical and biological data during RTX treatment
In our study, 23.4% of patients developed hypogammaglobulinemia during RTX treatment.
A recent adult cohort study conducted in 8633 patients who received RTX for autoimmune/rheumatologic diseases and malignancies showed that 19.3% of patients with normal IgG levels at baseline developed mild to severe hypogammaglobulinemia after RTX [8].
In our study, patients with more relapses during RTX treatment had more episodes of hypogammaglobulinemia even if all IgG levels were collected during remission with serum albumin > 30 g/L. In these patients, there is probably an overlap of two mechanisms, i.e., IgG urinary loss and RTX induced low IgG. Prospective follow-up cohort studies are needed in order to improve the comprehension of differential mechanisms leading to IgG deficiency in RTX-treated SDNS patients.
Further, we have shown that patients with hypogammaglobulinemia and those without did not differ in terms of global cumulative RTX doses and duration of B cell depletion. It has been reported previously that the cumulative RTX dose did not impact hypogammaglobulinemia development [10]. Moreover, different RTX treatment protocols are currently used in “difficult-to-treat” SDNS and some studies have assessed the effect of different RTX regimens [19] on B cell recovery and relapse rate, but the impact of these different RTX regimen on plasma IgG levels has never been investigated.
Concomitant infections during rituximab treatment
Our findings, although limited, seem to indicate that patients who developed hypogammaglobulinemia have a higher inherent risk of developing infections mostly ENT and pulmonary. Infections represent one of the most common adverse events of B cell depletion. A retrospective cohort study identified 2875 pediatric patients with 4639 RTX admissions across the USA and showed that infections after RTX exposure vary depending on the underlying condition. In this study, the frequency of sepsis ranged from 2.4% in patients with autoimmune diseases to 12.2% in those with primary immune deficiencies [20]. However, the hypogammaglobulinemia rate in these patients and the age at RTX initiation were not analyzed.
As expected from an epidemiological point of view, our data show that younger children developed more infections than older ones. Indeed, in the general population, preschool-aged children also have a higher incidence of viral infections and pneumonia than older children [21].
Furthermore, Barmettler et al. reported that 4.5% of RTX-treated adult patients received IVIg and that among these patients, a higher cumulative IVIg supplementation dose was associated with a reduced risk of serious infectious complications [8]. Although the role of IVIg therapy is not clearly established, it suggests that supplementation may be considered in those patients with low IgG levels and/or recurrent infections. Therapy may be of prolonged duration since hypogammaglobulinemia may persist for years despite cessation of RTX and B cell recovery [22].
In addition to monitoring IgG levels and infections, vaccine responses may help to identify high-risk patients who may benefit from IVIg. However, in our study, we reported only 13 concomitant infections in patients with hypogammaglobulinemia, and in the future, these data should be compared to a control group without hypogammaglobulinemia or SDNS in a prospective study.
Despite the relatively large patient number, there are several limitations, including the retrospective design, with possibly a selection, misclassification, and sampling bias with patients’ IgG levels checked more frequently as a result of a more severe clinical presentation.
Limitations should also be considered when interpreting the findings, in particular the absence of a control group and unavailable data on infection in patients without hypogammaglobulinemia, on cumulative corticosteroid or agranulocytosis which can differently affect the risk of infection in patients treated with RTX. Moreover, some patients did not have IgG levels tested during the RTX treatment period especially if IgG levels were normal at the RTX initiation. Therefore, we were unable to assess the true prevalence of hypogammaglobulinemia. Identically, the true prevalence of concomitant infection with a low IgG level is probably underestimated because some infections are treated as ambulatory and may not be listed in the medical file.
In conclusion, our findings suggest that B cell depletion is a risk factor for hypogammaglobulinemia, particularly in young children. Concomitant infections occur in a considerable number of patients with hypogammaglobulinemia. Therefore, the use of RTX, especially in younger children, should remain prudent and the benefit-risk ratio should be compared to alternative treatment modalities. IgG levels should be monitored systematically in RTX-treated patients, in order to identify those patients who may benefit from IVIg supplementation.
References
Sellier-Leclerc A-L, Baudouin V, Kwon T, Macher M-A, Guérin V, Lapillonne H, Deschênes G, Ulinski T (2012) Rituximab in steroid-dependent idiopathic nephrotic syndrome in childhood--follow-up after CD19 recovery. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 27:1083–1089
Fujinaga S, Hirano D, Nishizaki N, Kamei K, Ito S, Ohtomo Y, Shimizu T, Kaneko K (2010) Single infusion of rituximab for persistent steroid-dependent minimal-change nephrotic syndrome after long-term cyclosporine. Pediatr Nephrol Berl Ger 25:539–544
Colucci M, Carsetti R, Cascioli S, Casiraghi F, Perna A, Ravà L, Ruggiero B, Emma F, Vivarelli M (2016) B Cell Reconstitution after Rituximab Treatment in Idiopathic Nephrotic Syndrome. J Am Soc Nephrol JASN 27:1811–1822
Guigonis V, Dallocchio A, Baudouin V, Dehennault M, Hachon-Le Camus C, Afanetti M, Groothoff J, Llanas B, Niaudet P, Nivet H, Raynaud N, Taque S, Ronco P, Bouissou F (2008) Rituximab treatment for severe steroid- or cyclosporine-dependent nephrotic syndrome: a multicentric series of 22 cases. Pediatr Nephrol Berl Ger 23:1269–1279
Sellier-Leclerc A-L, Macher M-A, Loirat C, Guérin V, Watier H, Peuchmaur M, Baudouin V, Deschênes G (2010) Rituximab efficiency in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol Berl Ger 25:1109–1115
Kimata T, Hasui M, Kino J, Kitao T, Yamanouchi S, Tsuji S, Kaneko K (2013) Novel use of rituximab for steroid-dependent nephrotic syndrome in children. Am J Nephrol 38:483–488
Trujillo JE, Bosque M, Asensio Ò, Ranera A, Rojo JC, Vilella M, Guijarro E, Domingo X, Valdesoiro L, Larramona H (2014) PD42 - Is rituximab a trigger for persistent hypogammaglobulinemia in idiopathic nephrotic syndrome? Clin Transl Allergy 4:P42
Barmettler S, Ong M-S, Farmer JR, Choi H, Walter J (2018) Association of Immunoglobulin Levels, Infectious Risk, and Mortality With Rituximab and Hypogammaglobulinemia. JAMA Netw Open 1:e184169
Roberts DM, Jones RB, Smith RM, Alberici F, Kumaratne DS, Burns S, Jayne DRW (2015) Rituximab-associated hypogammaglobulinemia: incidence, predictors and outcomes in patients with multi-system autoimmune disease. J Autoimmun 57:60–65
Besada E, Koldingsnes W, Nossent JC (2014) Serum immunoglobulin levels and risk factors for hypogammaglobulinaemia during long-term maintenance therapy with rituximab in patients with granulomatosis with polyangiitis. Rheumatol Oxf Engl 53:1818–1824
Delbe-Bertin L, Aoun B, Tudorache E, Lapillone H, Ulinski T (2013) Does rituximab induce hypogammaglobulinemia in patients with pediatric idiopathic nephrotic syndrome? Pediatr Nephrol Berl Ger 28:447–451
Fujinaga S, Ozawa K, Sakuraya K, Yamada A, Shimizu T (2016) Late-onset adverse events after a single dose of rituximab in children with complicated steroid-dependent nephrotic syndrome. Clin Nephrol 85:340–345
Jolliff CR, Cost KM, Stivrins PC, Grossman PP, Nolte CR, Franco SM, Fijan KJ, Fletcher LL, Shriner HC (1982) Reference intervals for serum IgG, IgA, IgM, C3, and C4 as determined by rate nephelometry. Clin Chem 28:126–128
Agarwal S, Cunningham-Rundles C (2007) Assessment and clinical interpretation of reduced IgG values. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol 99:281–283
Sellier-Leclerc A-L, Belli E, Guérin V, Dorfmüller P, Deschênes G (2013) Fulminant viral myocarditis after rituximab therapy in pediatric nephrotic syndrome. Pediatr Nephrol Berl Ger 28:1875–1879
Fujinaga S, Nishino T, Umeda C, Tomii Y, Watanabe Y, Sakuraya K (2019) Long-term outcomes after early treatment with rituximab for Japanese children with cyclosporine- and steroid-resistant nephrotic syndrome. Pediatr Nephrol Berl Ger 34:353–357
Christou EAA, Giardino G, Worth A, Ladomenou F (2017) Risk factors predisposing to the development of hypogammaglobulinemia and infections post-Rituximab. Int Rev Immunol 36:352–359
Mariette X, Gottenberg J-E, Ravaud P, Combe B (2011) Registries in rheumatoid arthritis and autoimmune diseases: data from the French registries. Rheumatol Oxf Engl 50:222–229
Hogan J, Dossier C, Kwon T, Macher M-A, Maisin A, Couderc A, Niel O, Baudouin V, Deschênes G (2019) Effect of different rituximab regimens on B cell depletion and time to relapse in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol Berl Ger 34:253–259
Kavcic M, Fisher BT, Seif AE, Li Y, Huang Y-S, Walker D, Aplenc R (2013) Leveraging administrative data to monitor rituximab use in 2875 patients at 42 freestanding children’s hospitals across the United States. J Pediatr 162:1252–1258 1258.e1
Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy LB, Ziegler T, Kauppila J, Leinonen M, McCracken GH (2004) Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics 113:701–707
Barmettler S, Price C (2015) Continuing IgG replacement therapy for hypogammaglobulinemia after rituximab--for how long? J Allergy Clin Immunol 136:1407–1409
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parmentier, C., Delbet, JD., Decramer, S. et al. Immunoglobulin serum levels in rituximab-treated patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol 35, 455–462 (2020). https://doi.org/10.1007/s00467-019-04398-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04398-1