Abstract
Background
By adulthood, low birth weight infants have an increased risk for chronic kidney disease (CKD). The extent to which objective CKD risk factors are present at earlier ages is unclear.
Methods
We analyzed 5352 participants aged 12–15 years in the National Health and Nutrition Examination Survey, 1999–2012. Participants were classified as low birth weight (LBW; < 2500 g), very low birth weight (VLBW; < 1500 g), or normal (2500–4000 g) by parental/proxy recall. Albuminuria (albumin/creatinine 30 – <300 mg/g), decreased estimated glomerular filtration rate (eGFR; < 90 ml/min/1.73 m2; Counahan–Barratt), and elevated systolic blood pressure (BP; ≥ 95th percentile for age, height, and sex) were considered CKD risk factors.
Results
While albuminuria did not vary by birth weight, elevated blood pressure (BP) and decreased eGFR occurred more frequently in LBW/VLBW adolescents (elevated BP: LBW 6.0 %, VLBW 11.2 %, normal 2.4 %; decreased eGFR: LBW 23.2 %, VLBW 32.5 %, normal 16.1 %). After multivariable adjustment, LBW/VLBW adolescents had greater odds for both elevated BP (LBW: OR 2.90, 95 % CI 1.48–5.71; VLBW: 5.23; 1.11–24.74) and decreased eGFR (LBW: 1.49, 95 % CI 1.06–2.10; VLBW 2.49, 95 % CI 1.20–5.18).
Conclusions
In the U.S. population, both decreased eGFR and elevated systolic BP occur frequently among adolescents with history of LBW/VLBW.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global public health burden of chronic kidney disease (CKD) is substantial and growing [1, 2]. In the United States alone, 11.5 % of adults have CKD [3], and caring for patients with end-stage renal disease (ESRD) consumes 6.7 % of the Medicare budget [4]. There is no cure for CKD [5]. Attenuating the effects of the CKD epidemic therefore requires improved detection, surveillance, and prevention of late-stage CKD [6].
There is convincing epidemiologic evidence that persons with low birth weight (LBW; < 2500 g) have an increased risk for developing CKD or ESRD by adulthood [7]. The Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guideline for CKD recognizes LBW as a potential risk factor for CKD susceptibility and initiation, and further recommends that all individuals at increased risk of developing CKD undergo testing to estimate glomerular filtration rate (eGFR) and assess markers of kidney damage [8]. When screening should occur for a static, lifelong CKD risk factor such as LBW is not clear. These knowledge gaps make it difficult to conduct decision analyses, formulate policy, or guide clinical care.
We therefore sought to determine the prevalence and population impact of CKD risk factors (including albuminuria, elevated systolic blood pressure, and abnormal eGFR) among adolescents aged 12–15 years with a history of LBW in a nationally representative cross-sectional survey.
Methods
Study population
We pooled data for participants 12–15 years of age from the National Health and Nutrition Examination Survey (NHANES) cycles from 1999–2012. NHANES is a complex, cross-sectional probability sample of the non-institutionalized United States population, conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention.
All participants aged 12–15 years old were initially included. Participants were excluded from all analyses if they were missing data for birth weight; pregnant at the time of the exam; or missing all data for all of the CKD risk factors of interest (blood pressure, eGFR, and albuminuria). To facilitate a comparison between adolescents with low birth weight and normal birth weight, participants with birth weight > 4000 g were also excluded from all analyses. Participants who were missing data for a particular factor of interest were excluded from those analyses only, as summarized in Fig. 1.
Birth weight
Birth weight was ascertained by parental or proxy recall using a survey instrument. Participants were classified as normal (2500–4000 g), LBW (<2500 g), and very low birth weight (VLBW; < 1500 g), as appropriate. Because all VLBW infants are also LBW infants, participants with birth weight < 1500 g were included in both VLBW and LBW analyses.
Blood pressure
Three systolic blood pressure (BP) readings were obtained for each NHANES participant. If one or more of these readings were disrupted, a fourth reading was obtained. Mean systolic BP was calculated from the available readings for each participant. Elevated systolic BP was defined as mean systolic BP ≥ 95th percentile for the participant’s age, sex, and height according to The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents [9].
Serum creatinine and eGFR
Serum creatinine was determined using a kinetic alkaline picrate (Jaffe) method. Because the analyzer for serum creatinine changed throughout the study period, we applied the recommended corrections [10, 11] to standardize serum creatinine measurements across survey years as below:
eGFR was calculated using the Counahan–Barratt equation:
[12]. Decreased eGFR was evaluated at three thresholds: < 60 ml/min/1.73 m2, < 75 ml/min/1.73 m2, and < 90 ml/min/1.73 m2. Hyperfiltration was defined as eGFR > 150 ml/min/1.73 m2.
Urine albumin and creatinine
Urine albumin and creatinine were measured in a random urine sample. Before 2007, urine creatinine was measured by Jaffe reaction; after 2007, an enzymatic creatinase reaction was used. We used the recommended corrections [13] to account for this change as follows:
-
Urine creatinine < 75 mg/dl: Corrected creatinine = (1.02*sqrt(Creatinine) – 0.36)2
-
Urine creatinine 75 to < 250 mg/dl: Corrected creatinine = (1.05*sqrt(Creatinine) – 0.74)2
-
Urine creatinine ≥ 250 mg/dl: Corrected creatinine = (1.01*sqrt (Creatinine) – 0.10)2
Albuminuria was defined as an albumin-to-creatinine ratio (ACR) of ≥ 30 and < 300 mg/g.
Statistical analyses
All statistical analyses were performed using IBM SPSS® version 23 (Armonk, NY, USA) or SAS version 9.3 (Cary, NC, USA) using a calculated 14-year exam sample weight to account for NHANES complex sample design. Data from the 2000 United States Census were used to extrapolate weighted proportions to population estimates, with population estimates corresponding to the population of 12 to 15-year-old adolescents at the midpoint of the merged survey periods (approximately January 1, 2006).
Continuous variables were compared using the Student’s t test and categorical variables were compared by χ 2 test. Linear and logistic regression models were used to evaluate the association of LBW or VLBW with continuous and binary variables, respectively. Multivariable models were created to adjust for differences in age, sex, race category, body mass index (BMI), z score, and poverty–income ratio. Candidate variables for multivariable regression models were determined by biological plausibility or p < 0.20 in univariable analysis. A two-sided significance level of 0.05 was set for all tests.
Three measures of exposure impact were calculated. First, the number needed to be exposed (NNE) with adjustment for confounders was estimated from adjusted odds ratios (OR) obtained in multivariable logistic regression models according to the method of Bender and Blettner [14]. In this context, the NNE estimates the number of adolescents who would need to be born with LBW/VLBW for there to be one additional adolescent with a CKD risk factor who would not otherwise have had that CKD risk factor.
Second, we calculated the population attributable risk (PAR), representing the reduction in the incidence of CKD risk factors that would be observed if the entire population was unexposed to LBW/VLBW. To account for potential confounders, the PAR was calculated from adjusted ORs [15] as follows:
Third, we calculated the attributable population, representing the absolute number of adolescents in the general U.S. population whose CKD risk factors were attributable to LBW/VLBW exposure. The attributable population was calculated as the product of the PAR and the total population of cases for each CKD risk factor.
Results
Study population
A total of 5352 participants were analyzed, representing a total population of 13,941,330. Among these, 9.0 % reported a history of LBW, and 1.3 % reported a history of VLBW. Demographic and clinical features of the study population are shown in Table 1.
Urine albumin/creatinine
Albuminuria (ACR 30 – <300) was present in 13.7 % of the population, while overt proteinuria (ACR ≥ 300 mg/g) was present in 1.8 %. Neither the frequency of albuminuria nor the frequency of overt proteinuria varied by birth weight category. There was no association between LBW or VLBW status and albuminuria in either univariable or multivariable logistic regression models (Table 2).
eGFR
Across the entire population, the mean eGFR was 107.9 (95 % CI 106.8–109.1) ml/min/1.73 m2. Among adolescents with normal birth weight, the mean eGFR was 108.2 (95 % CI 107.0–109.4) ml/min/1.73 m2, compared to 105.6 (95 % CI 102.6–108.5) ml/min/1.73 m2 for LBW adolescents and 101.5 (95 % CI 95.5–107.4) ml/min/1.73 m2 for VLBW adolescents. In a multivariable general linear model, every 1 kg increase in birth weight up to 4 kg increased eGFR by 2.4 ml/min/1.73 m2 (95 % CI 1.0–3.8, p = 0.001; model R2 0.16). In this model, the marginal mean difference in eGFR between VLBW adolescents and those with normal birth weight was –6.1 ml/min/1.73 m2 (p = 0.03).
eGFR < 60 ml/min/1.73 m2 was present in only four participants (0.06 %). None of these participants had albuminuria. There was no association between birth weight and eGFR < 60 ml/min/1.73 m2.
eGFR < 90 ml/min/1.73 m2 with albuminuria was present in 2.2 % of the population. The frequency did not vary by birth weight: 2.1 % (95 % CI 0.9–4.9 %) of adolescents with history of LBW had eGFR < 90 ml/min/1.73 m2 with albuminuria, versus 2.2 % (95 % CI 1.6–2.9 %) of those with normal birth weight.
There was an inverse relationship between birth weight and eGFR at both the < 75 ml/min/1.73 m2 and < 90 ml/min/1.73 m2 thresholds (Fig. 2). In univariable and multivariable logistic regression models, both LBW and VLBW adolescents had greater odds for eGFR < 90 ml/min/1.73 m2. However, only VLBW adolescents had greater odds for eGFR < 75 ml/min/1.73 m2. Hyperfiltration was present in 2.4 % (1.7–3.0 %) of adolescents, and did not vary by birth weight category (Table 2).
Systolic blood pressure
Overall, 2.7 % (2.0–3.4 %) of participants had elevated systolic BP. Adolescents with history of LBW or VLBW had greater odds for elevated systolic BP, even after adjustment in multivariable logistic regression models (Table 2). In multivariable logistic regression, every 1 kg increase in birth weight up to 4 kg decreased the odds for having elevated systolic blood pressure by half (OR 0.50; 95 % CI 0.31–0.81; p = 0.005). In a multivariable general linear model, each 1 kg increase in birth weight up to 4 kg was associated with a change in systolic blood pressure of 1.1 mm Hg (95 % CI –1.8 to –0.3; p = 0.005; R 2 = 0.16).
Population impact measures
Measures of exposure impact were calculated for elevated systolic BP and decreased eGFR (Table 3). Exposure impact as determined by NNE was greater for VLBW than for LBW adolescents for all measures calculated. However, because of the increased prevalence of LBW compared to VLBW, the attributable population was larger for LBW than for VLBW.
Discussion
In a large, nationally representative cross-sectional sample of adolescents, lower birth weight was associated with decreased eGFR and higher systolic BP (but not albuminuria) by age 12–15 years. These associations persisted even after adjustment for confounding factors. This is the first population-based assessment of CKD and CKD risk factors for adolescents with a history of LBW or VLBW.
These findings support the growing body of literature demonstrating increased risk for impaired renal function among persons born with LBW, and additionally provide an estimate of the magnitude of that effect on a population basis. For every 12.7 adolescents with a history of LBW or every 5.1 adolescents with a history of VLBW in the United States, there was one additional person with eGFR < 90 ml/min/1.73 m2 and/or elevated systolic blood pressure at age 12–15. Overall, approximately 120,000 adolescents in the United States had decreased eGFR and/or elevated systolic BP attributable to their history of LBW (Table 3).
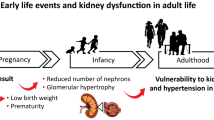
The reasons for this may be multifactorial. Both premature and LBW infants often begin life with decreased nephron number due to impaired nephrogenesis [16, 17] and altered developmental programming [18]. Reduced nephron number may lead to glomerular hypertrophy, hyperfiltration, and ultimately secondary glomerulosclerosis [19]. Even after birth, threats to nephron survival persist. Acute kidney injury occurs in 18–40 % [20, 21] of VLBW infants, and may be a particular risk factor for later CKD [22–24]. Nephrotoxic medication exposure is also common, with 87 % of VLBW infants receiving at least one nephrotoxic medication before discharge (or one per every six hospital days) [25]. Infants with LBW or in utero growth restriction may undergo accelerated or excessive “catch up” growth, which is associated with elevated BP [26, 27] and potentially CKD [28].
Yet in spite of the recognition of LBW as a risk factor for CKD, there is little specific guidance for clinicians caring for these patients. While the American Academy of Pediatrics provides clinical guidelines for the general care [29] and neurodevelopmental follow up [30] of premature infants early in life, there are no guidelines for when or whether these patients should be screened for CKD. Similarly, while the K/DOQI clinical practice guideline for CKD recommends laboratory screening for patients at risk for CKD, it is silent on when such testing should occur for patients with LBW [8]. Risk-based screening for albuminuria or decreased eGFR in early adolescence has been proposed for LBW/VLBW patients [31], but there is no evidence to support either the efficacy or cost-effectiveness of this approach. The data provided here may inform such an analysis, since the results are representative of the U.S. adolescent population.
A few observations about our findings may be useful in designing or assessing the value of a screening program. First, albuminuria was common, and did not vary by birth weight category. However, in NHANES, albuminuria was determined on the basis of a single random, non-supine void, which may lack the specificity to distinguish patients with true kidney disease in the pediatric population. Orthostatic [32], exercise-induced [33], and other benign or transient proteinurias are common in pediatric patients, and most adolescents who have albuminuria do not have any other risk factors for cardiovascular disease [34]. In this context, albuminuria—or at least albuminuria assessed on a single random urine sample—is not likely to be an effective screening strategy for identifying CKD among adolescents with a history of LBW. Alternative strategies should be explored.
Second, though blood pressure should be measured for all adolescent health visits [9], our data highlight the importance of this for patients with a history of LBW or VLBW. Hypertension is both a cause and a consequence of CKD [35] and there was an inverse linear association between birth weight and systolic blood pressure at age 12–15. Among all adolescents with elevated BP, approximately 13.1 % was attributable to LBW history.
Finally, while eGFR < 60 ml/min/1.73 m2 was rare, more modest decreases in eGFR were common in our population. Nearly one-quarter of LBW adolescents, one-third of VLBW adolescents, and almost half of adolescents with birth weight < 1000 g had eGFR < 90 ml/min/1.73 m2. Such mild decreases in eGFR are unlikely to be of any immediate clinical consequence. Previous analyses of NHANES have shown that adolescents with eGFR ≤ 10th percentile were no more likely than peers with higher eGFR to have anemia, metabolic acidosis, hyperphosphatemia, short stature, elevated BP, or albuminuria [36]. Yet, even mildly reduced GFR may have long-term consequences. CKD risk factors can be identified ≥ 30 years before CKD diagnosis in the general population [37], and among adults in the Framingham Heart Study, an eGFR < 90 ml/min/1.73 m2 was associated with a threefold increase in the odds of progression to CKD when compared to those with eGFR ≥ 120 ml/min/1.73 m2 over approximately 20 years of follow-up [38]. It should be considered that decreased GFR may confer a very different long-term prognosis for a young adolescent than a middle-aged adult, but whether earlier identification of patients with decreased eGFR would be beneficial or an example of overdiagnosis [39] requires longitudinal study.
Our study has several limitations. First, while nationally representative, NHANES data are cross-sectional. Therefore, elevated systolic BP was determined on the basis of a single physical examination, rather than the three or more required to diagnose hypertension [9]. However, elevated BP on even a single occasion increases the likelihood of being diagnosed with hypertension in later adolescence [40, 41] or adulthood [42]. Similarly, we could not determine the chronicity of decreased eGFR; it is possible that participants had decreased kidney function only transiently. However, it is unclear why this would occur unequally between birth weight groups.
Second, we estimated GFR using the Counahan–Barratt equation, which was developed for and validated in a population with CKD [12]. This could lead to a systematic underestimation of GFR in healthy adolescents [29]. However, the mathematical formula differs only slightly from the revised Schwartz equation [43] (k = 0.43 vs. k = 0.413), which has been validated in a predominantly non-CKD population [44]. Using the revised Schwartz formula in our study population resulted in slightly higher population estimates for adolescents with decreased eGFR but did not alter statistical inference or hypothesis testing. Because the revised Schwartz equation was derived using serum creatinine measurements made by enzymatic methods traceable to isotope dilution mass spectrometry [43], the Counahan–Barratt equation may be the more appropriate formula for estimating GFR using the creatinine methodology used in NHANES. Further, creatinine-based formulae for eGFR have not been validated in LBW and VLBW individuals, in whom catch-up growth is associated with a higher fat mass percentage [45].
Third, in NHANES, birth weight was obtained by parental recall, not validated independently. However, the frequency of elevated systolic BP and decreased eGFR among participants with non-recalled birth weight did not differ from those with normal birth weight. Additionally, parental recall of birth weight has been shown to be an accurate proxy for recorded birth weight, with 75 % of parents recalling a weight within 50 g of the child’s documented weight up to 16 years after delivery [46]. The identification of LBW adolescents by parental recall likely also better approximates clinical practice.
Fourth, although both prematurity and intrauterine growth restriction affect nephron endowment and influence long-term CKD risk [16, 17, 27], gestational age is not recorded in NHANES. Our analyses were therefore limited to birth weight alone.
Finally, while we believe that these data could be useful in assigning probabilities for decision analysis [47] or for informing screening policy, the data presented are frequencies only. It is unknown how many NHANES participants with CKD risk factors were previously aware of their condition. Indeed, patients with LBW are over-represented in the Chronic Kidney Disease in Children (CKiD) cohort [48].
In summary, in a nationally representative survey, CKD risk factors (including elevated systolic BP and decreased eGFR) were found more frequently among 12 to 15-year-old adolescents with a history of LBW or VLBW than among their peers with normal birth weight, even after adjusting for potentially confounding factors. This study is the first to provide population-based estimates of the prevalence of CKD risk factors for adolescents with history of LBW or VLBW in the general U.S. adolescent population, and highlight the need for long-term follow-up of these patients.
References
Meguid El Nahas A, Bello AK (2005) Chronic kidney disease: the global challenge. Lancet 365:331–340
Couser WG, Remuzzi G, Mendis S, Tonelli M (2011) The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int 80:1258–1270
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
U.S. Renal Data System (2011) USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, p 282. http://www.usrds.org/2011/pdf/v2_ch011_11.pdf. Accessed March 7, 2016.
Levey AS, Coresh J (2012) Chronic kidney disease. Lancet 379:165–180
Levey AS, Andreoli SP, DuBose T, Provenzano R, Collins AJ (2007) Chronic kidney disease: common, harmful, and treatable – World Kidney Day 2007. Clin J Am Soc Nephrol 2:401–405
White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, Haysom L, Craig JC, Salmi IA, Chadban SJ, Huxley RR (2009) Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis 54:248–261
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1–S266
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2 Suppl 4th Report):555–576
Selvin E, Manzi J, Stevens LA, Van Lente F, Lacher DA, Levey AS, Coresh J (2007) Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis 50:918–926
Centers for Disease Control and Prevention (CDC) (2015) National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey 2005–2006, Data Documentation, Codebook, and Frequencies. Standard Biochemistry Profile (BIOPRO_D). March 2008. http://wwwn.cdc.gov/Nchs/Nhanes/2005–2006/BIOPRO_D.htm. Accessed June 15, 2015
Counahan R, Chantler C, Ghazali S, Kirkwood B, Rose F, Barratt TM (1976) Estimation of glomerular filtration rate from plasma creatinine concentration in children. Arch Dis Child 51:875–878
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey 2007–2008, Data Documentation, Codebook, and Frequencies: Albumin & Creatinine – Urine (ALB_CR_E). September 2009. http://wwwn.cdc.gov/Nchs/Nhanes/2007–2008/ALB_CR_E.htm. Accessed June 15, 2015
Bender R, Blettner M (2002) Calculating the “number needed to be exposed” with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol 55:525–530
Miettinen OS (1974) Proportion of disease caused or prevented by a given exposure, trait, or intervention. Am J Epidemiol 99:325–332
Charlton JR, Springsteen CH, Carmody JB (2014) Nephron number and its determinants in early life: a primer. Pediatr Nephrol 29:2299–2308
Abitbol CL, Rodriguez MM (2012) The long-term renal and cardiovascular consequence of prematurity. Nat Rev Nephrol 8:265–274
Luyckx VA, Bertram JF, Brenner BM, Fall C, Hoy WE, Ozanne SE, Vikse BE (2013) Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet 382:273–283
Hodgin JB, Rasoulpour M, Markowitz GS, D’Agati VD (2009) Very low birth weight is a risk factor for secondary focal segmental glomerulosclerosis. Clin J Am Soc Nephrol 4:71–76
Koralkar R, Ambalavanan N, Levitan EB, McGwin G, Goldstein S, Askenazi D (2011) Acute kidney injury reduces survival in very low birth weight infants. Pediatr Res 69:354–358
Carmody JB, Swanson JR, Rhone ET, Charlton JR (2014) Recognition and reporting of AKI in very low birth weight infants. Clin J Am Soc Nephrol 9:2036–2043
Abitbol CL, Bauer CR, Montane B, Chandar J, Duara S, Zilleruelo G (2003) Long-term follow-up of extremely low birth weight infants with neonatal renal failure. Pediatr Nephrol 18:887–893
Askenazi DJ, Morgan C, Goldstein SL, Selewski DT, Moxey-Mims MM, Kimmel PL, Star RA, Higgins R, Laughon M (2015) Strategies to improve the understanding of long-term renal consequences after neonatal acute kidney injury. Pediatr Res. doi:10.1038/pr.2015.241
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, Kent AL (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473
Rhone ET, Carmody JB, Swanson JR, Charlton JR (2014) Nephrotoxic medication exposure in very low birth weight infants. J Matern Fetal Neonatal Med 27:1485–1490
Huxley RR, Shiell AW, Law CM (2000) The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens 18:815–831
Luyckx VA, Brenner BM (2015) Birth weight, malnutrition and kidney-associated outcomes—a global concern. Nat Rev Nephrol 11:135–149
Silverwood RJ, Pierce M, Hardy R, Sattar N, Whincup P, Ferro C, Savage C, Kuh D, Nitsch D (2013) Low birth weight, later renal function, and the roles of adulthood blood pressure, diabetes, and obesity in a British birth cohort. Kidney Int 84:1262–1270
American Academy of Pediatrics. Committee on Practice and Ambulatory Medicine and Committee on Fetus and Newborn (1996) The role of the primary care pediatrician in the management of high-risk newborn infants. Pediatrics 98:786–788
Wang CJ, McGlynn EA, Brook RH, Leonard CH, Piecuch RE, Hsueh SI, Schuster MA (2006) Quality-of-care indicators for the neurodevelopmental follow-up of very low birth weight children: results of an expert panel process. Pediatrics 117:2080–2092
Carmody JB, Charlton JR (2013) Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics 131:1168–1179
Brandt JR, Jacobs A, Raissy HH, Kelly FM, Staples AO, Kaufman E, Wong CS (2010) Orthostatic proteinuria and the spectrum of diurnal variability of urinary protein excretion in healthy children. Pediatr Nephrol 25:1131–1137
Jefferson IG, Greene SA, Smith MA, Smith RF, Griffin NK, Baum JD (1985) Urine albumin to creatinine ratio—response to exercise in diabetes. Arch Dis Child 60:305–310
Nguyen S, McCulloch C, Brakeman P, Portale A, Hsu CY (2008) Being overweight modifies the association between cardiovascular risk factors and microalbuminuria in adolescents. Pediatrics 121:37–45
Klahr S (1989) The kidney in hypertension: villain and victim. N Engl J Med 320:731–733
Fadrowski JJ, Neu AM, Schwartz GJ, Furth SL (2011) Pediatric GFR estimating equations applied to adolescents in the general population. Clin J Am Soc Nephrol 6:1427–1435
McMahon GM, Preis SR, Hwang SJ, Fox CS (2014) Mid-adulthood risk factor profiles for CKD. J Am Soc Nephrol 25:2633–2641
Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D (2004) Predictors of new-onset kidney disease in a community-based population. JAMA 291:844–850
Coon ER, Quinonez RA, Moyer VA, Schroeder AR (2014) Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics 134:1013–1023
Falkner B, Gidding SS, Portman R, Rosner B (2008) Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics 122:238–242
Redwine KM, Acosta AA, Poffenbarger T, Portman RJ, Samuels J (2012) Development of hypertension in adolescents with pre-hypertension. J Pediatr 160:98–103
Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, Derazne E, Tzur D, Gershnabel D, Grossman E, Karasik A, Shamiss A, Shai I (2010) Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension 56:203–209
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Staples A, LeBlond R, Watkins S, Wong C, Brandt J (2010) Validation of the revised Schwartz estimating equation in a predominantly non-CKD population. Pediatr Nephrol 25:2321–2326
Kensara OA, Wootton SA, Phillips DI, Patel M, Jackson AA, Elia M (2005) Fetal programming of body composition: relation between birth weight and body composition measured with dual-energy X-ray absorptiometry and anthropometric methods in older Englishmen. Am J Clin Nutr 82:980–987
O'Sullivan JJ, Pearce MS, Parker L (2000) Parental recall of birth weight: how accurate is it? Arch Dis Child 82:202–203
Naglie G, Krahn MD, Naimark D, Redelmeier DA, Detsky AS (1997) Primer on medical decision analysis: Part 3—Estimating probabilities and utilities. Med Decis Making 17:136–141
Greenbaum LA, Munoz A, Schneider MF, Kaskel FJ, Askenazi DJ, Jenkins R, Hotchkiss H, Moxey-Mims M, Furth SL, Warady BA (2011) The association between abnormal birth history and growth in children with CKD. Clin J Am Soc Nephrol 6:14–21
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The research ethics review board of the National Center for Health Statistics approved all study protocols, and both written consent from the participant’s guardian and verbal assent from the adolescent were obtained.
Funding
None.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Khalsa, D.D.K., Beydoun, H.A. & Carmody, J.B. Prevalence of chronic kidney disease risk factors among low birth weight adolescents. Pediatr Nephrol 31, 1509–1516 (2016). https://doi.org/10.1007/s00467-016-3384-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3384-7