Abstract
Introduction
Acute colonic obstruction is a frequent emergency condition in a general surgical setting. The use of an endoscopic self-expanding stent can relieve obstruction and eventually prepare the patient for elective laparoscopic or open surgery.
Materials and Methods
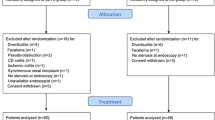
From September 2001 to March 2006 we treated 25 patients with acute left or transverse colonic obstruction. In 23 patients stents were positioned planning an elective procedure to be performed. In two patients with multiple liver metastases and malignant ascites only a palliation was intended (2 of 25 patients).
Results
Mean age was 66.6 years. The 23 patients who underwent resection, 14 females and nine males, had a mean age of 65.5 years. Obstructions were located in the rectum (five), in the sigmoid (16) and in the transverse colon (two). In one patient stricture was due to radiotherapy, in twenty four cases it was due to primary cancer. Stents were successfully placed in 24 patients. In one of them two stents had to be placed due to the slippage of the first one beyond the stricture. Excellent resumption of colonic transit was achieved in all the patients. No complications were observed. In 23 patients resection was performed (19 laparoscopy; four open). Complications occurred in one patient in open group (pancreatic fistula after splenectomy) and was treated conservatively. Mean postoperative stay was 18.5 (range 9–35) days for the open group and 12 (range 9–20) for the laparoscopic group. Mean follow-up was 36 months.
Conclusions
use of self expanding endoscopic colonic stents can provide excellent palliation in acute obstruction, aiming both to prepare the colon to elective surgery after adequate preparation or to palliate the stricture in case of unresectable advanced tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute colonic obstruction is a common condition in a general surgical setting, often leading to emergency surgery and frequently followed by severe complications, such as dehiscence of the anastomosis, surgical site infection, pneumonia, cardiovascular complications, venous thrombosis and so on. Moreover, mortality rate in emergency setting accounts for 3% to 45% according to the series (0.9%-6.0% in elective surgery [1–8]) and a preoperative study of the patient is not possible. Furthermore, even after adjustment for the TNM stage, survival rate is significantly lower after emergency surgery compared with elective procedures [6, 8] (classification for cancers T = tumours, N = nodes, M = metastasis). Half of the patients are not suitable for a single-stage operation, thus requiring a second or even a third admission to avoid permanent colostomy.
Initially, the technique has provided a palliative role for patients deemed to have unresectable cancer [9, 10].
Recently the use of colonic self-expandable stents to resolve obstruction has been advocated in the management of the acute phase so to schedule patients for elective surgery [11–13]. In these cases a complete intestinal preparation and patient evaluation can be accomplished.
Laparoscopic colon resections, introduced in the early 1990s, have consistently been shown to ameliorate the postoperative course, reducing postoperative morbidity, improving patient comfort, and shortening hospital stay [14, 15].
The aim of this study is to assess the feasibility, effectiveness and safety of endoscopically placed self-expandable stents in colonic obstruction, both as a bridge-to-surgery and palliation.
Materials and methods
From September 2001 to March 2006, 25 patients with symptoms of left bowel obstruction, such as severe constipation longer than 48 h, abdominal distension, nausea, vomiting and cramping abdominal pain were admitted to our department and within 24 hours a water-soluble contrast enema was performed to confirm the diagnosis and localize the stenosis. Stents were placed in patients with symptoms and radiological evidence of colorectal obstruction. Informed consent was obtained from each patient. Patients with clinical and/or radiological evidence of bowel perforation, peritonitis or massive gastrointestinal bleeding were not involved in the study. Stents were positioned in the radiological department by means of a combination of fluoroscopy and endoscopy. Patients were sedated with intravenous midazolam and petidine as needed. A guide wire was passed through the stenosis under fluoroscopic guidance and a catheter was then introduced over the guidewire. Water-soluble contrast was then delivered through the catheter to carefully characterize the length of the stenosis and to allow proper choice of the stent (Enteral Wallstent Microvasive, Boston Scientific, Minnesota USA). According to the stenosis 6 cm or 9 cm stents were used (Figs. 1 and 2). They were deployed under fluoroscopic guidance allowing the stent to extend 1–2 cm on both sides of the stenosis (Fig. 3). After placing the stent, a plain X-ray film was obtained to confirm its correct position (Fig. 4).
Data regarding the endoscopic procedure, complications and patient outcome were prospectively collected. Endoscopy was technically successful when the colonic stent was correctly deployed across the stricture. The correct placement of the stent was assessed by evidence of restoration of bowel function (Fig. 5). Clinical success was defined as colonic decompression and relief of obstructive symptoms within 24 h after stent placement with reprise of oral. Two to four days after the placement of the stent surgical resection was performed when indicated. Preoperative bowel cleansing was obtained in all surgical cases without difficulties. Surgical resection consisted in open or laparoscopic left colectomy according to the indications.
For each patient, clinical information was accumulated in a prospective database including age, gender, American Society of Anaesthesiology (ASA) classification, diagnosis, place of stricture along the colon. Operative data included operative time as measured from the first skin incision to the application of dressings, kind of procedure (laparoscopic or open), need of laparotomic conversion, need of colostomy, surgical TNM, postoperative length of hospital stay.
Postoperative follow-up was performed by means of clinical examination, while other data was obtained through chart and computer reviews of surgical notes and referring outpatients ambulance follow-up visits. Relevant information included complications and wound infections.
Results
Patient characteristics
Twenty-five patients were admitted to our department with signs and symptoms of colonic obstruction between September 2001 and March 2006. The mean age was 66.6 years (range 50–81). They all were submitted to abdominal X-rays and colonoscopy. In all patients (n = 25) there were radiological signs of acute large-bowel obstruction (Fig. 6).
In two cases the stent was positioned as a palliative treatment: a 71-year-old woman and an 81-year-old man who presented abdominal pain, diarrhoea and anaemia. Dilation of the bowel, liver metastases and malignant ascites were found during computerized tomography (CT) scan examination. They have a malignant stenosis at 57 and 40 cm from the anal verge. Remission of the symptoms was achieved and the patients were discharged with supportive therapy.
In 23 patients, 14 female and nine male, stents were positioned planning an elective procedure, and stenting was considered a bridge to surgery. Here, obstructions were localized in the rectum (five cases), in the sigmoid (16 cases), and in the transverse colon (two cases). Patients’ mean age was 65.5 years, ASA score was 2 for 10 patients and 3 for the other 13.
In all patients stent placement was successfully achieved in a single procedure (mean operative time 30 min). In one case two stents were necessary due to displacement of the first one beyond the stenosis, during the procedure. In all patients prompt remission of the symptoms was obtained. In two patients the stent was passed through the anus. The first case was a woman with a post-actinic stenosis of the rectum after a low anterior resection. The second was a woman in which a pneumatic dilation of the stenosis was done after placement of the stent.
Results of laparoscopic resection
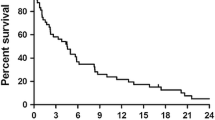
Nineteen patients underwent a laparoscopic left colon resection (operative time 150 min, range 120–180 mins). Complications were two wound infection of minilaparotomy according to Pfannenstiel. Mean postoperative stay was 12 days (range 9–20) and stoma placement was not necessary. Stages of resected tumors were: T3N0M0 for nine patients, T3N1M0 for four patients, T4N0M0 for one patient, and T4N1M0 for five patients. All patients who underwent laparoscopic resection are still alive with a median follow up of 36 months.
Results of open resection
Four patients underwent open resection instead of a laparoscopic one. The first patient underwent open resection of rectal post-actinic stricture and repair of a large incisional hernia with a mesh. She had undergone low anterior resection for cancer in 2001 and laparotomy for occlusion in early 2002. Another patient underwent open resection because the mass in the left colon was palpable and fixed to the abdominal wall. Liver metastases were present. The two last patients underwent open resection because the lesion was in the transverse colon and was infiltrating the abdominal wall and the spleen. Complications were one pancreatic fistula following splenectomy due to infiltration (treated with percutaneous drainage) and one minor wound infection. Mean operative time for laparotomic resection was 223 min (range 160–300). Mean postoperative stay was 18.5 days (range 9–35). One patient affected by rectal post actinic stricture required stoma placement, because of compromised intestinal trophism due to Radiotherapy (RT). Moreover, she had developed adhesions due to previous operations and was in malnourished state. The stages of the resected tumors were: T3N1M1, T3N2, T4N0, respectively. All patients who underwent open resection are still alive with a median follow up of 36 months.
Discussion
Acute colonic obstruction is a common condition in a general surgical setting, accounting for 7% to 29% of colorectal cancer [2, 16, 17]; it is a surgical emergency because it evolves rapidly to metabolic and electrolyte modifications, intestinal ischemia with perforation, and finally sepsis and death [18]. Patients are often elderly and tumors are in an advanced stage. Because of such conditions surgical risk is usually very high, both for systemic and local factors. Surgery usually requires decompression by colostomy and, whenever possible, resection and anastomosis. On the other hand, elective colonic resections (with a cleansed colon) are associated with a mortality rate lower than 5%, in contrast to emergency resections, which are associated with a postoperative mortality as high as 23% [19].
Recent studies suggest that early placement of a colonic stent may be more effective that the traditional approach of emergency surgery for management of patient with acute malignant colonic obstruction; specifically use of a colonic stent may minimize expensive sequential operations, reduce stoma requirements vs. initial emergency surgery (15.4% vs. 58.6%; 7% vs. 43%) [20, 28]. Actually these are the studies in the literature that report the best results in terms of reduction of stoma requirement rate using colonic stents.
Moreover, an initial colonic stent leads to a higher likelihood of stoma requirement only when the rate of technical failure of stent placement exceeds 26%, but no published case series analysis of the rate of technical success has demonstrated a success rate below 75% [28]. Therefore, it is unlikely that colonic stent insertion will lead to excessive stoma requirement.
Despite the small number of prospective studies, stent insertion has been proven feasible, safe and effective, with a rate of technical and clinical success greater than 90% [29, 30, 31, 32].
In our study no stoma was necessary in all laparoscopic resections. This data is probably due to the clinical success rate of stent placement (100%) with resumption of colonic transit and relief of obstructive symptoms in the absence of perforations and obstructions in all the patients, thus demonstrating that bowel preparation and planned resection must be the goal of this approach to colonic obstruction [20, 28].
Efficient palliation of symptoms can also be achieved by stenting in patients which will not undergo resection, both for refusal or end-stage disease [21].
In our small series we demonstrate that stent placement is feasible and effective in relieving symptoms. Several types of stents are available, either covered or uncovered. We believe that uncovered stents (such as Enteral Wallstent, Microvasive, Boston Scientific, Minnesota USA) are more flexible and provide good results. Transit is always restored by the stent and dilation can cause, as in our case, slippage of the stent. After displacement of the stent no symptoms of re-occlusion were detected.
By the way, in other studies complications were observed, mainly colonic perforations, minor bleeding and anal pain [22–24].
Using a self-expanding stent can avoid emergency surgery, and all risks related to resection and anastomosis of a dilated and unprepared bowel. Moreover it allows high-risk patients to be hydrated and prepared for elective surgery, by means of bowel washout. Large rectal tumors can be submitted to neoadjuvant chemo-radiotherapy, allowing sphincter-saving resections [25]. Quality of life without the need for colostomy or multistage operations has to be stressed.
Recent reviews of the literature have found an increasing number of papers dealing with this approach to acute colonic obstruction [26, 27]. These papers report relief of obstruction in more than 90% of patients. Minor complications attributable to stenting in reported studies were successfully managed with medical or supportive treatment in the majority of cases. Perforation is the most severe complication observed, usually leading to an emergency Hartmann procedure.
In our series the postoperative complications were: a wound infection in a very complex patient who underwent her third laparotomy and had a large incisional hernia repair at the end of the resection (operative time 300 minutes); a low-output pancreatic fistula observed in a patient who presented with a transverse colon stenosis that was infiltrating the upper left abdominal wall and the inferior pole of the spleen. In the latter case, Ultrasound (US)-guided percutaneous drainage and total parenteral nutrition resolved the fistula in 15 days.
Conclusion
Endoscopic and fluoroscopic guided self-expandable metallic stenting of acute colonic obstructions plays a role in treating patients which have a poor surgical risk. Lowering the need for colostomy, one-stage surgical procedure and a lower complication rate seem to be major advantages.
Further studies, i.e. randomised controlled studies with operative controls are needed to confirm these initial findings.
References
Griffith RS (1992) Preoperative evaluation: medical obstacles to surgery. Cancer 70: 1333–1341
Deans GT, Krukowski ZH, Irwin ST (1994) Malignant obstruction of the left colon. Br J Surg 81: 1270–1276
Witzig JA, Morel P, Erne M, Egeli R, Borst F, Rohner A (1993) Chirurgie des cancer digestifs des patients de plus de 80 ans. Helv Chir Acta 59: 767–769
Messmer P, Thoni F, Ackermann C, Herzog U, Schuppiser JP, Tondelli P. Perioperative morbidity and mortality of colon resection in colonic carcinoma
Buechter KJ, Bounstany C, Caillouete R (1998) Surgical management of the acutely obstructed colon. Am J Surg 156:163–168
Runkel NS, Schlag P, Schwarz V, Herfarth C (1991) Outcome after emergency surgery for cancer of the large intestine. Br J Surg 78: 183–188
Fielding LP, Stewart-Brown S, Blesovsky L (1979) Large bowel obstruction caused by cancer: a prospective study. Br Med J 2: 515–517
Scott NA, Jeacock J, Kingston RD (1995) Risk factors in patients presenting as an emergency with colorectal cancer. Br J Surg 82: 321–323
Choo IW, Do YS, Suh SW, Chun HK, Choo SW, Park HS, Kang SK, Kim SK (1998) malignant colorectal obstruction: treatment with a flexible covered stent. Radiology 2006: 415–421
Turegano-Fuentes F, Echenagusia-Belda A, Simon-Muerza G, Camunez F, minoz-Jimenez F, Della Valle Hernandez E, Quintas-Rodriguez A (1998) Transanal self-expanding metal stents as an alternative to palliative colostomy in selected patients with malignant obstruction of the left colon. Br J Surg 85: 232–235
Tejero E, Mainar A, Fernandez L, Tobio R, De Gregorio MA (1994) New method for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum 37: 1158–1159
Saida Y, sumiyama Y, Nagao J, Takase M (1996) Stent endoprosthesis for obstructing colorectal cancers. Dis Colon Rectum 39: 552–555
Akle CA (1998) Endoprostheses for colonic strictures. Br J Surg 85: 310–314
Hoffman G, Baker J, Fitchett C, Vansant J (1994) Laparoscopic assisted colectomy: Initial experience. Ann Surg 219: 732–743
Lacy AM, Garca-Valdecasas J, Pacheco JL, Visa J (1995) Short-term outcome analysis of a randomized study comparing laparoscopic vs. open colectomy for colon cancer. Surg Endosc 9: 1101–1105
Regland JJ, Londe AM, Spratt JS (1971) Correlation of the prognosis of obstructing colorectal carcinoma with clinical and pathologic variables. Am J Surg 121:552–556
Serpell JW, McDermott FT, Katrivessus H, Huhes ESR (1989) Carcinomas of the colon causing intestinal occlusion. Br J Surg 2: 549–554
Leithman IM, Sullivan JD, Brams D, DeCosse JJ (1992) Multivariate analysis of morbidity and mortality from the initial surgical management of obstructing carcinoma of the colon. Surg Gynecol Obstet 174: 513–518
Mauro MA, Koehler RE, Baron TH (2000) Advances in gastrointestinal intervention: the treatment of gastroduodenal and colorectal obstruction with metallic stents. Radiology 215: 659–669
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M (2002) Self-expandable stent bifore elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rate. Dis Colon Rectum 45: 401–406
Law WL, Chu KW, Ho JWC, Tung HM, Law SYK, Chu KM (2000) Self-expanding metallic stent in the treatment of colonic obstruction caused by advanced malignancy. Dis Colon Rectum 43: 1522–1527
Mainar A, De Gregorio Ariza MA, Tejero E, Tobio R, Alfonso E, Pinto I, Herrera M, Fernandez JA (1999) Acute colorectal obstruction treatment with self-expandable metallic stents before scheduled surgery. Results of a multicenter study. Radiology 10: 65–69
Camunez F, Echenagusia A, Simo G, Turegano F, Vazquez J, Barreiro-Meiro I (2000) Malignat colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation. Radiology 216: 492–497
Ely CA, Arregui ME (2003) The use of enteral stents in colonic and gastric outlet obstruction. Surg Endosc 17: 89–94
Liberman H, Adams DR, Blatchford GJ, Ternent CA, Christensen MA, Thorson AG (2001) Clinical use of the self-expanding metallic stent in the management of colorectal cancer. Am J Surg 180: 407–412
Harris GJC, Senagore AJ, Lavery IC, Fazio VW (2001) The management of neoplastic colorectal obstruction with colonic endoluminal stenting devices. Am J Surg 181: 499–506
Dauphine CE, Tan P, Beart Jr RW, Vukasin P, Cohen H, Corman ML (2002) Placement of self-expanding metal stents for acute malignant large-bowel obstruction: a collective review. Ann Surg Oncol 9: 574–579
Laura E. Targownik, Brennan M. Spiegel, Jonathan Sack, Oscar J. Hines, Gareth S. Dulai, Ian M. Gralnek, James J. Farrell (2004) Colonic stent vs. emergency surgery for management of acute left-side malignant colonic obstruction: a decision analysis. Gastrointest Endosc 60: 865–74
Crosta C, Trovato C, Fiori G, Ravizza D, Tamayo D, Zampino MG, Biffi R (2006) Metal stent placement in acute malignant colorectal obstruction. Digestive and Liver Disease 38: 341–346
Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plantaniotis G, et al. (2004) Stenting or stoma creation for patients with inoperable malignant colonic obstruction? Results of a study and cost-effectiveness analysis. Surg Endosc 18: 421–6
Khot UP, Lang AW, Murali K, Parker MC (2002) Systematic review of the efficay and safety of colorectal stents. Br J Surg 89: 1096–102
Dulucq J-L, Wintringer P, Beyssac R, Barberis C, Talbi P, Mahajna A (2006) One stage laparoscopic colorectal resection after placement of self-expanding metallic stents for colorectal obstruction. Dig Dis Sci 2006 Nov 1; [epub ahead of print]
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Olmi, S., Scaini, A., Cesana, G. et al. Acute colonic obstruction: endoscopic stenting and laparoscopic resection. Surg Endosc 21, 2100–2104 (2007). https://doi.org/10.1007/s00464-007-9352-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9352-3