Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) in patients with BMI ≥ 60 presents technical challenges, that might be overcome by robotic surgery, but its effectiveness has not been rigorously evaluated. We compared the 30-day outcomes of LSG and robotic sleeve gastrectomy (RSG) in patients with BMI < 60 versus ≥ 60 and between LSG and RSG in patients with BMI ≥ 60.
Methods
Patients aged 18–65 years who underwent sleeve gastrectomy were included using the 2019–2022 MBSAQIP database. We performed a Propensity Score Matching analysis, with 21 preoperative characteristics. We compared 30-day postoperative outcomes for patients with BMI < 60 versus ≥ 60 using either a laparoscopic (Analysis 1) or robotic approach (Analysis 2) and compared LSG versus RSG in patients with BMI ≥ 60 (Analysis 3).
Results
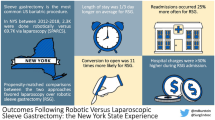
297,250 patients underwent LSG and 81,008 RSG. Propensity-matched¸ outcomes in analysis 1 (13,503 matched cases), showed that patients with BMI ≥ 60 had higher rates of mortality (0.1% vs. 0.0%, p = 0.014), staple line leak (0.3% vs. 0.2%, p = 0.035), postoperative bleeding (0.2% vs 0.1%, p = 0.028), readmissions (3.5% vs. 2.4%, p < 0.001), and interventions (0.7% vs. 0.5%, p = 0.028) when compared to patients with BMI < 60. In analysis 2 (4350 matched cases), patients with BMI ≥ 60 demonstrated longer operative times, length of stay, and higher rates of unplanned ICU when compared to patients with BMI < 60. In analysis 3 (4370 matched cases), patients who underwent RSG had fewer readmissions (2.9% vs. 3.7%, p = 0.037), staple line leaks (0.1% vs. 0.3%, p = 0.029), and postoperative bleeding (0.1% vs. 0.3%, p = 0.045), compared to LSG. Conversely, a longer operative time (92.74 ± 38.65 vs. 71.69 ± 37.45 min, p < 0.001) was reported.
Conclusion
LSG patients with BMI ≥ 60 have higher rates of complications compared to patients with a BMI < 60. Moreover, some outcomes may be improved with the robotic approach in patients with BMI ≥ 60. These results underscore the importance of considering a robotic approach in this super super obese population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Obesity has become a global health concern with an expected global rise from 14 to 24% of the population by 2035, as projected by the World Obesity Federation [1]. This alarming trend has intensified the demand for efficacious weight loss interventions, particularly bariatric procedures [2, 3]. With over 270,000 bariatric surgeries performed annually in the USA, sleeve gastrectomy (SG) stands out as one of the most popular bariatric surgery due to its safety and effectiveness in promoting weight loss and resolving obesity-related comorbidities [4,5,6,7].
The rise of minimally invasive surgery has established laparoscopic SG as a highly preferred technique, improving operative outcomes and lowering morbidity and mortality in the short and long term [8,9,10]. Following the pioneering robotic bariatric procedure in 2000, the adoption of robotic platforms is steadily on the rise, driven by technological advancements [11,12,13]. Robotic surgery brings a host of technical enhancements to the table, including precise tissue manipulation, improved three-dimensional imaging, and enhanced autonomy for the surgeon through self-assisting exposure capabilities [14]. Studies have demonstrated controversial results on robotics, some showing that bariatric robotic surgeries are associated with lower mortality and postoperative bleeding rates [15, 16]. On the other hand, Li et al., in a systematic review reported longer operative times and higher hospital costs compared to the laparoscopic approach [17].
Patients with super-super obesity, defined as those with a body mass index (BMI) ≥ 60 kg/m2, pose significant technical challenges during bariatric surgery. Despite the considerable number of patients with BMI ≥ 60 kg/m2, there is a scarcity of research on this particular patient population [18]. Robotic surgery presents a significant advantage with its improved dexterity and enhanced precision which could be a compelling option for this high-risk population to overcome the technical challenges [19].
We aim to compare the 30-day postoperative outcomes and bariatric-specific complications for patients with BMI < 60 versus ≥ 60 who underwent laparoscopic sleeve gastrectomy (LSG) or robotic sleeve gastrectomy (RSG) and to compare LSG versus RSG in patients with a BMI ≥ 60 through a comprehensive analysis of the 2019–2022 MBSAQIP database.
Materials and methods
Study population
Patients who underwent either RSG or LSG within the MBSAQIP data registry from January 1, 2019 to December 31, 2022 were included in this study. Patients who underwent primary SG were identified within the 2020 and 2021 MBSAQIP participant use file (PUF) using the Current Procedural Terminology codes 43775.
Exclusion criteria included patients younger than 18 years old and older than 65 years old. Also, patients who had other approaches besides conventional laparoscopic and robotic-assisted such as hand-assisted, open, single incision, and natural orifice transluminal endoscopic surgery were excluded. Additionally, 30-day re-admission, re-operation, and intervention data were extracted from separate files by matching the unique case identification numbers. MBSAQIP data are de-identified and contain no personal health information, and consequently, data were publicly available in an anonymous manner. Existing de-identified datasets as MBSAQIP by federal regulations do not constitute strictly Human Subjects Research; therefore, the Institutional Review Board (IRB) of The Johns Hopkins Hospital approved the study under exempt status.
Data sources
The 2019, 2020, 2021, and 2022 MBSAQIP participant use files (PUF) were used for the study. The MBSAQIP-PUF is one of the largest bariatric-specific clinical data sets. There were 817,099 bariatric cases from approximately 924 MBSAQIP participating sites performed from January 1, 2019 to December 31, 2022 across the USA and Canada. The MBSAQIP-PUF is a bariatric surgery-specific clinical data set, which contains nearly 200 variables including preoperative patient characteristics, procedure details, as well as details on complications, reoperations, readmissions, or interventions within 30 days in both the inpatient and outpatient setting. The MBSAQIP-PUF does not identify hospitals or individual healthcare providers. The data registry collects prospective, risk-adjusted information based on previously standardized definitions for preoperative, intraoperative, and postoperative variables specific to bariatric surgery. Data are collected and audited at each center by trained reviewers.
Propensity score matching (PSM)
To overcome potential biases from the different distributions of covariates among patients who underwent LSG or RSG, a propensity score analysis was performed for each surgical approach. The PSM included 21 preoperative characteristics and comorbidities. We obtained a 1:1 nearest-neighbor matching with no replacement. To exclude bad matches, we imposed a caliper of 0.2 of the standard deviation of the logit of the propensity score. Propensity score analysis and matching were performed with the PS matching program that performs all analyses in R through the SPSS R-Plugin (SPSS R Essentials) and utilizes newly written R code as described by Thoemmes [20].
The preoperative characteristics and comorbidities that were matched include age, sex, ASA score, race, history of myocardial infarction, cardiac stent, cardiac surgery, diabetes mellitus, hypertension requiring medications, hyperlipidemia, deep venous thrombosis, pulmonary embolism, use of therapeutic anticoagulation, chronic obstructive pulmonary disease, smoker status, renal insufficiency, dialysis-dependent, sleep apnea, GERD, chronic corticosteroid/ immunosuppressive therapy, and functional status. After matching, we examined the balance of all observed covariates using absolute standardized mean differences which are the absolute value of the difference in means between groups.
Surgical outcomes
Eighteen postoperative outcomes within the first 30 days of operation were assessed. These included mortality, cardiac complications (cardiac arrest or myocardial infarction), pulmonary complications (pneumonia, unplanned intubation or mechanical ventilation for more than 48 h), renal complications (renal failure or dialysis requirement), sepsis (sepsis or septic shock), unplanned ICU, blood transfusions, re-admissions, re-operations, interventions, emergency visits, venous thromboembolism (VTE—including deep venous thrombosis or pulmonary embolism), wound disruption, incisional hernia, surgical site infection (SSI), non-home discharge, operative time, and length of hospital stay. In addition, we obtained eight composite outcomes that were coded in the suspected causes for re-operation, interventions, and re-admission files in the MBSAQIP data set. These composite outcomes were staple line leak, postoperative bleeding, stricture, gastrointestinal perforation, and gallstone disease.
Statistical analysis
Univariate analyses were performed using either the Pearson × 2 test (or Fisher’s exact test for rare events) for categorical variables. Independent sample t-test was used for normally distributed continuous variables and Mann–Whitney test for skewed continuous variables. The results were reported as the frequency and percentage for categorical variables and mean (± standard deviation) for continuous variables. After PSM analyses, matched pair cohort was assessed using the paired McNemar test for categorical variables, paired t-test for continuous variables normally distributed or Wilcoxon signed-rank sum test for non-normally distributed continuous variables. Any p value < 0.05 was considered statistically significant. All analyses were performed with computer software (IBM SPSS Statistics, Version 29.0, IBM Corp., Armonk, NY).
Results
Patient demographic characteristics
A total of 378,258 patients met the inclusion criteria. 297,250 and 81,008 were included for LSG (78.6%) and RSG (21.4%), respectively. In analysis 1, patients who underwent LSG with BMI < 60 (n = 283,723) were compared to patients with BMI ≥ 60 (n = 13,527), whereas in analysis 2, patients who underwent RSG with BMI < 60 (n = 76,636) were compared to patients with BMI ≥ 60 (n = 4372). In the analysis, 3 patients with BMI ≥ 60 who underwent LSG (n = 13,527) were compared to patients who underwent RSG (n = 4372). Propensity score matching analysis was performed to adjust for preoperative characteristics and comorbidities. Statistically significant variables before propensity score matching in analyses 1, 2, and 3 are displayed in Tables 1, 2, and 3.
In all three analyses, a 1:1 PSM analysis was performed. In Analysis 1; 13,503 patients were obtained. There were no statistically significant differences in preoperative patient variables after PSM. All the standardized differences were ≤ 0.10. The highest standardized mean difference after matching was found in dependent functional status with a value of d = 0.012 (Table 1). In Analysis 2, 4350 patients were obtained. There were no statistically significant differences in preoperative patient variables after PSM. All the standardized differences were ≤ 0.10. The highest standardized mean difference after matching was found in white ethnicity with a value of d = 0.030 (Table 2). In Analysis 3, 4370 patients were obtained. There were no statistically significant differences in preoperative patient variables after PSM. All the standardized differences were ≤ 0.10. The highest standardized mean difference after matching was found in sleep apnea with a value of d = 0.034 (Table 3).
Outcomes of matched cohorts
After propensity matching in analysis 1, patients with BMI ≥ 60 showed higher rates of mortality (0.1% vs. 0.0%, p = 0.014), staple line leak (0.3% vs. 0.2%, p = 0.035), and postoperative bleeding (0.2% vs 0.1%, p = 0.028), when compared to patients with BMI < 60. Similarly, longer operative times (72.22 ± 37.54 min vs. 66.38 ± 32.92 min, P < 0.001), length of stay (1.45 ± 1.25 days vs. 1.31 ± 1.14 days, p < 0.001), and higher rates of renal complications (0.3% vs. 0.2%, p = 0.045), non-home discharge (30.1% vs. 27.8%, P < 0.001), readmissions (3.5% vs. 2.4%, P < 0.001), interventions (0.7% vs. 0.5%, p = 0.028), and unplanned ICU admissions (1.1% vs. 0.5%, p < 0.001) were found in patients with BMI > 60 (Table 4).
In analysis 2, patients with BMI ≥ 60 demonstrated longer operative times (92.73 ± 38.67 min vs. 86.72 ± 35.47 min, p < 0.001), length of stay (1.46 ± 1.79 days vs 1.30 ± 0.87 days, p < 0.001), and higher rates of unplanned ICU admissions (0.9% vs 0.5%, p = 0.015) when compared to patients with BMI < 60. Other 30-day outcomes such as mortality, staple line leak, postoperative bleeding, readmissions, and interventions were comparable between these groups (Table 5).
In analysis 3, patients who underwent RSG reported fewer readmissions (2.9% vs. 3.7%, p = 0.037), staple line leaks (0.1% vs. 0.3%, p = 0.029), and postoperative bleeding (0.1% vs. 0.3%, p = 0.045), compared to LSG. Conversely, a longer operative time (92.74 ± 38.65 min vs. 71.69 ± 37.45 min, p < 0.001) was found for RSG compared to LSG (Table 6).
Disclosures
Alba Zevallos, Jorge Cornejo, Jennifer Brown, Joaquin Sarmiento, Fatemeh Shojaeian, Farzad Mokhtari-Esbuie, Christina Li and Raul Sebastian have no conflicts of interest or financial ties to disclose. Alisa Coker accepts honoraria for teaching, speaking, and consulting for Intuitive Surgical. Gina Adrales reports an unrelated disclosure of honoraria for consulting for Caresyntax, Inc and Ethicon Johnson and Johnson Advisory Board.
Discussion
The current 2019–2022 MBSAQIP database analysis is the first study comparing 30-day postoperative outcomes and bariatric-specific complications between patients with BMI < 60 versus ≥ 60 using either a laparoscopic or robotic approach and between LSG and RSG in patients with BMI ≥ 60. Our study revealed that patients with BMI ≥ 60 undergoing LSG are at higher risk of perioperative complications and 30-day mortality compared with patients with BMI < 60, a risk that is not associated with RSG. Moreover, when we sub-analyzed only patients with BMI ≥ 60, we found that patients who underwent RSG had lower rates of perioperative complications in terms of readmissions, staple line leaks, and postoperative bleeding compared to LSG.
In our Analysis 1, comparing patients with BMI < 60 vs BMI ≥ 60, who underwent LSG, other authors reported similar results to our study regarding mortality (0.0% vs. 0.1%; p = 0.014). Nasser et al. in a large cohort study reported a significantly higher mortality rate in the super-super obese group at 0.18%, compared to super obese (0.08%) and patients with morbid obesity (0.04%) [21]. Furthermore, patients with BMI ≥ 60 who underwent LSG showed higher rates of staple line leak (0.3% vs. 0.2%, p = 0.035), and postoperative bleeding (0.3% vs. 0.2%, p = 0.028) compared to patients with BMI < 60, leading to a significant increase in readmissions (3.5% vs. 2.4%, p < 0.001), interventions (0.7% vs. 0.5%, p = 0.028), and unplanned ICU admissions (1.1% vs. 0.5%, p < 0.001).
LSG in patients with super super obesity poses significant challenges due to the increased abdominal wall thickness, and visceral fat [22,23,24]. We hypothesize that there is a higher risk of staple line leak and bleeding due to the hindering of appropriate exposure to the operative field, making mobilization and visualization difficult. Consistent with this hypothesis, Gaillard et al. found that visceral obesity > 85 cm2/m2 increases the risk for staple line leak rates by fivefold [23], whereas Han et al. in a small population study reported that a visceral fat area > 100 cm2 increases the risk by sixfold of early postoperative complications including bleeding [24].
On the other hand, in Analysis 2, comparing patients with BMI < 60 versus ≥ 60 who underwent RSG, our study did not find statistical differences in mortality, staple line leak, postoperative bleeding, readmissions, and interventions. However, we found significant differences regarding unplanned ICU admissions (0.9% vs 0.5%, p = 0.015), longer operative times (92.73 ± 38.67 min vs. 86.72 ± 35.47 min, p < 0.001), and length of stay (1.46 ± 1.79 days vs. 1.30 ± 0.87 days, p < 0.001) in patients with BMI ≥ 60. RSG may be a better alternative in patients with super super obesity. However, with either approach, patients with BMI ≥ 60 have a higher rate of complications.
Finally, in Analysis 3, when comparing LSG versus RSG in patients with BMI ≥ 60, patients who underwent RSG had fewer readmissions (2.9% vs. 3.7%, p = 0.037), staple line leaks (0.1% vs. 0.3%, p = 0.029), and postoperative bleeding (0.1% vs. 0.3%, p = 0.045), compared to LSG. These findings might be attributed to the surgeons’ experience and the unique properties of the robotic platform which provides a three-dimensional image, filters out tremors, improves precision, and facilitates delicate movements in limited spaces, thereby minimizing tissue damage. Moreover, the utilization of robotic-controlled surgical staplers featuring Smartfire or Fire-fly technology offers surgeons improved engagement and compression control before and during stapling [25, 26]. Conversely, the operative time was significantly increased in the RSG group (92.74 ± 38.65 min vs. 71.69 ± 37.45 min, p < 0.001). Our operative time findings are similar to other studies. Scarritt et al. examined outcomes over four years in robotic bariatric surgery, and showed similar results, highlighting that although operative time remained significantly longer with the robotic approach, postoperative outcomes improved as the robotic platform's utilization increased [27]. Therefore, we suggest the use of the robotic platform for a sleeve gastrectomy in patients with super super obesity.
The MBSAQIP is the most comprehensive resource for analyzing the field of bariatric surgery. Nevertheless, there are some limitations of the dataset to consider. First, some relevant variables are not recorded in this database such as visceral fat and abdominal wall thickness. Second, the robotic stapler and featured technology (Smartfire or Fire-fly) are not reported. Third, the surgeon’s experience in the robotic field is not reported. Fourth, our study exclusively captures 30-day postoperative data; thus, determining long-term outcomes is beyond the scope of this study. Despite these limitations, our study provides an analysis of one of the largest samples from a national bariatric-specific database.
We conclude that LSG patients with a BMI ≥ 60 have a higher rate of mortality, staple line leaks, postoperative bleeding, and readmissions compared to patients with a BMI < 60. Moreover, patients who underwent RSG with BMI ≥ 60 have lower rates of readmissions, staple line leaks, and postoperative bleeding compared to RSG. These results validate the importance of considering the robotic approach in this super-super obese population.
Change history
18 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00464-024-11000-9
References
World Obesity Foundation (2023) World obesity atlas 2023. https://s3-eu-west-1.amazonaws.com/wof-files/World_Obesity_Atlas_2023_Report.pdf
Arterburn DE, Courcoulas AP (2014) Bariatric surgery for obesity and metabolic conditions in adults. BMJ 349:g3961. https://doi.org/10.1136/bmj.g3961
Wolfe BM, Kvach E, Eckel RH (2016) Treatment of obesity: weight loss and bariatric surgery. Circ Res 118:1844–1855. https://doi.org/10.1161/CIRCRESAHA.116.307591
American Society for Metabolic and Bariatric Surgery (n.d.) Estimate of bariatric surgery numbers, 2011–2022. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers/
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N (2018) IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28:3783–3794. https://doi.org/10.1007/s11695-018-3450-2
Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L (2020) Changes in utilization of bariatric surgery in the united states from 1993 to 2016. Ann Surg 271:201–209. https://doi.org/10.1097/SLA.0000000000003554
Chang D-M, Lee W-J, Chen J-C, Ser K-H, Tsai P-L, Lee Y-C (2018) Thirteen-year experience of laparoscopic sleeve gastrectomy: surgical risk, weight loss, and revision procedures. Obes Surg 28:2991–2997. https://doi.org/10.1007/s11695-018-3344-3
Kikkas EM, Sillakivi T, Suumann J, Kirsimägi Ü, Tikk T, Värk PR (2019) Five-year outcome of laparoscopic sleeve gastrectomy, resolution of comorbidities, and risk for cumulative nutritional deficiencies. Scand J Surg 108:10–16. https://doi.org/10.1177/1457496918783723
Salminen P, Helmiö M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, Hurme S, Soinio M, Nuutila P, Victorzon M (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic roux-en-y gastric bypass on weight loss at 5 years among patients with morbid obesity: the sleevepass randomized clinical trial. JAMA 319:241–254. https://doi.org/10.1001/jama.2017.20313
Emile SH, Elfeki H, Elalfy K, Abdallah E (2017) Laparoscopic sleeve gastrectomy then and now: an updated systematic review of the progress and short-term outcomes over the last 5 years. Surg Laparosc Endosc Percutan Tech 27:307–317. https://doi.org/10.1097/SLE.0000000000000418
Bauerle WB, Mody P, Estep A, Stoltzfus J, El Chaar M (2023) Current trends in the utilization of a robotic approach in the field of bariatric surgery. Obes Surg 33:482–491. https://doi.org/10.1007/s11695-022-06378-1
Bindal V, Bhatia P, Dudeja U, Kalhan S, Khetan M, John S, Wadhera S (2015) Review of contemporary role of robotics in bariatric surgery. J Minim Access Surg 11:16–21. https://doi.org/10.4103/0972-9941.147673
Horgan S, Vanuno D (2001) Robots in laparoscopic surgery. J Laparoendosc Adv Surg Tech A 11:415–419. https://doi.org/10.1089/10926420152761950
Jung MK, Hagen ME, Buchs NC, Buehler LH, Morel P (2017) Robotic bariatric surgery: a general review of the current status. Int J Med Robot. https://doi.org/10.1002/rcs.1834
Sebastian R, Howell MH, Chang K-H, Adrales G, Magnuson T, Schweitzer M, Nguyen H (2019) Robot-assisted versus laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a propensity score-matched comparative analysis using the 2015–2016 MBSAQIP database. Surg Endosc 33:1600–1612. https://doi.org/10.1007/s00464-018-6422-7
Zhang Z, Miao L, Ren Z, Li Y (2021) Robotic bariatric surgery for the obesity: a systematic review and meta-analysis. Surg Endosc 35:2440–2456. https://doi.org/10.1007/s00464-020-08283-z
Li K, Zou J, Tang J, Di J, Han X, Zhang P (2016) Robotic versus laparoscopic bariatric surgery: a systematic review and meta-analysis. Obes Surg 26:3031–3044. https://doi.org/10.1007/s11695-016-2408-5
Stephens DJ, Saunders JK, Belsley S, Trivedi A, Ewing DR, Iannace V, Capella RF, Wasielewski A, Moran S, Schmidt HJ, Ballantyne GH (2008) Short-term outcomes for super-super obese (BMI > or =60 kg/m2) patients undergoing weight loss surgery at a high-volume bariatric surgery center: laparoscopic adjustable gastric banding, laparoscopic gastric bypass, and open tubular gastric bypass. Surg Obes Relat Dis 4:408–415. https://doi.org/10.1016/j.soard.2007.10.013
Gray KD, Pomp A, Dakin G, Amanat S, Turnbull ZA, Samuels J, Afaneh C (2018) Perioperative outcomes and anesthetic considerations of robotic bariatric surgery in a propensity-matched cohort of super obese and super-super obese patients. Surg Endosc 32:4867–4873. https://doi.org/10.1007/s00464-018-6241-x
Thoemmes FJ, Kim ES (2011) A systematic review of propensity score methods in the social sciences. Multivar Behav Res 46:90–118. https://doi.org/10.1080/00273171.2011.540475
Nasser H, Ivanics T, Leonard-Murali S, Shakaroun D, Genaw J (2019) Perioperative outcomes of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in super-obese and super-super-obese patients: a National Database Analysis. Surg Obes Relat Dis 15:1696–1703. https://doi.org/10.1016/j.soard.2019.07.026
Pasanta D, Htun KT, Pan J, Tungjai M, Kaewjaeng S, Chancharunee S, Tima S, Kim HJ, Kæwkhao J, Kothan S (2021) Waist circumference and BMI are strongly correlated with mri-derived fat compartments in young adults. Life (Basel) 11:643. https://doi.org/10.3390/life11070643
Gaillard M, Esposito A, Lainas P, Cerbelaud P, Voican CS, Courie R, Chague P, Perlemuter G, Rocher L, Dagher I, Tranchart H (2021) Computed tomography assessment of fat distribution and staple-line leak risk after sleeve gastrectomy. Obes Surg 31:2011–2018. https://doi.org/10.1007/s11695-020-05199-4
Han L, Deng C, Zhao R, Wan Q, Zhang X, Wang X, Chen Y (2023) Excess visceral fat area as an independent risk factor for early postoperative complications in patients with obesity undergoing bariatric surgery. Front Endocrinol (Lausanne) 14:1072540. https://doi.org/10.3389/fendo.2023.1072540
Morrell ALG, Morrell AC, Morrell-Junior AC, Mendes JM, Tustumi F, Morrell AG (2021) Indocyanine green fluorescence imaging in robotic surgery: state of art, tips and tricks in current applications. Arq Gastroenterol 58:61–70. https://doi.org/10.1590/S0004-2803.202100000-11
Giffen Z, Ezzone A, Ekwenna O (2021) Robotic stapler use: is it safe?-FDA database analysis across multiple surgical specialties. PLoS ONE 16:e0253548. https://doi.org/10.1371/journal.pone.0253548
Scarritt T, Hsu C-H, Maegawa FB, Ayala AE, Mobily M, Ghaderi I (2021) Trends in utilization and perioperative outcomes in robotic-assisted bariatric surgery using the mbsaqip database: a 4-year analysis. Obes Surg 31:854–861. https://doi.org/10.1007/s11695-020-05055-5
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zevallos, A., Cornejo, J., Brown, J. et al. A superior approach? The role of robotic sleeve gastrectomy in patients with super super obesity using the 2019–2022 MBSAQIP database. Surg Endosc 38, 4594–4603 (2024). https://doi.org/10.1007/s00464-024-10955-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10955-z