Abstract
Background
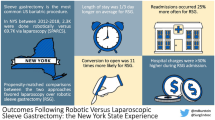
Sleeve gastrectomy (SG) is an effective treatment option for patients with obesity. Robotic sleeve gastrectomy (RSG) is reported to have worse short-term patient outcomes compared to laparoscopic SG (LSG), but prior studies may not have accounted for evolving technology, including stapler utilization.
Objective
This study compared RSG and LSG outcomes over different time periods.
Setting
Academic Hospital.
Material and Methods
The 2015 to 2021 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MBSAQIP) databases were used. Matched cohort analyses compared adverse outcomes within 30 days for the 2015–2018 and 2019–2021 cohorts. Bivariate and regression models compared cohorts using Stata/MP 17.0.
Results
Seven hundred sixty-eight thousand and sixty-nine SG were analyzed. Over the 7-year study period, all patient outcomes, operation length (OL), and length of stay (LOS) trended downward for RSG, except surgical site infection (SSI). In the 2015–2018 cohort, leak was significantly higher with RSG (OR 1.53), and OL and LOS longer (p < 0.001). In the 2019–2021 cohort which corelated with a significant increase in robotic cases, leak (OR 1.36), SSI (OR 1.46), and morbidity (OR 1.11) were higher with RSG. While the mean difference in OL and LOS decreased between the two time periods, they remain longer for RSG (p < 0.001).
Conclusion
While RSG and LSG are safe with similar mortality, RSG continues to be associated with higher rates of morbidity, leak, and SSI, as well as longer OL, hospital LOS, and higher cost. The study is limited by the ability to account for the impact of surgeon experience and stapler utilization on outcomes.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleeve gastrectomy is the most common metabolic and bariatric surgery (MBS) procedure performed, representing over 60% of all MBS cases in the U.S. [1] It has been shown to be an effective treatment modality for patients with severe obesity, with low mortality 0.36% [2, 3] and morbidity rates 6–9% [4,5,6], as well as achieving long-term total body weight loss of 21.7 ± 10.7% [7] and excess body weight loss of 55.5 ± 27.5% [7,8,9] with significant improvement in weight-related comorbid disease in all age groups [10,11,12,13].
While most sleeve gastrectomies are performed with conventional laparoscopy [14], the robotic platform has been increasingly used [15, 16]. Overall, SG is associated with a 5–6% complication rate and a 3–4% reoperation rate [14, 17, 18]. Early comparative studies have shown no clear benefits of robotic sleeve gastrectomy, when compared to laparoscopic sleeve gastrectomy [19, 20]. Several studies have shown longer operative duration associated with robotic sleeve gastrectomy [21,22,23]. Studies have also shown higher rates of surgical site infections (SSI) [22, 24] and leak [22] associated with robotic sleeve gastrectomy.
In addition to robotic metabolic surgery volume growth, technology associated with the robotic platform also continues to evolve and may impact surgical outcomes for cases performed using this platform [25]. This includes robotic stapling technology advancement with introduction of the SureForm stapler, an Intuitive Surgical Inc. proprietary device, in mid-2018 [26, 27]. The extent to which robotic volume growth and evolving technology have impacted outcomes of robotic sleeve gastrectomy is unclear. In this study, we aimed to compare outcomes of RSG and LSG performed during different time periods.
Material and Methods
Using the 2015–2021 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MBSAQIP) databases, we performed a matched retrospective cohort analysis. Due to the de-identified nature of the data contained in the MBSAQIP registry, institutional review board (IRB) approval or patient consent was not required.
Inclusion, Exclusion, and Study Cohorts
We included patients receiving a primary sleeve gastrectomy (SG) (CPT 43,775) between 2015 and 2021, performed only by conventional laparoscopic or robotic assisted. We excluded patients identified as having a revision or conversion procedure, missing data, having a procedure other than a primary SG, or performed with a surgical approach other than conventional laparoscopic or robotic assisted (Fig. 1). Three study cohorts were evaluated, including (1) an overall cohort taking into consideration all included SG performed between 2015 and 2021, (2) a subset including all surgeries performed between 2015 and 2018, and (3) all surgeries occurring between 2019 and 2021. The rationale for comparing cases performed in 2015–2018 and 2019–2021 is due to the introduction of the SureForm stapler in mid-2018.
Dependent Variables
The primary outcome for this study was death within 30 days of operation. Secondary outcomes include venous thromboembolism (VTE), leak, surgical site infection (SSI), bleeding, morbidity, operation length in minutes, and length of stay in days.
Independent Variables
The primary independent variable was robotic assisted versus conventional laparoscopic surgical approach. Patient-specific variables include age, race, body mass index (BMI) category (≤ 30, 31–40, 41–50, > 50 kg/m2), pre-operative albumin lab category (< 3, 3–3.5, > 3.5 g/dl), gender, American Society of Anesthesiologists (ASA) class, functional health status (independent, partially dependent, totally dependent), gastroesophageal reflux disease (GERD) requiring medication, hypertension requiring medication, history of myocardial infarction, hyperlipidemia, venous status, vein thrombosis requiring therapy, history of pulmonary embolism, history of IVC filter, diabetes, dialysis, current smoker within 1 year, chronic obstructive pulmonary disease (COPD), obstructive sleep apnea (OSA), and previous obesity or foregut surgery.
Statistical Analyses
Means and standard deviations or frequencies and percentages were used to describe variables. Pearson’s chi-squared tests were used to evaluate categorical variables, and the Kruskal–Wallis tests were used to assess continuous variables. In each cohort, a 1:1 caliper match was used to identify robotic-assisted and laparoscopic SG cases for comparison. The match allowed for a 5-year difference in age between the groups, and all other independent variables required an exact match. Model balance was determined by assessing differences between the matched groups for each variable. In each model, there were no identified differences between the cohorts. Conditional fixed-effects logistic regression models were then used to assess differences in the categorical variables and linear regression for continuous variables outcomes using the matched groupings generated through the caliper match. In each case, adjusted odds ratios, 95% confidence intervals, and p-values are reported. Stata/MP 17.0 was used to conduct statistical analyses, and a p-value < 0.05 and a 95% confidence interval excluding 1.0 were considered significant.
Results
Of 768,069 SG cases analyzed, 79.92% were female, 62.5% were non-Hispanic white (NHW), 21.2% non-Hispanic black (NHB), and 16.3% Hispanic patients. Eight-seven percent of cases were performed with conventional laparoscopic (LSG) and 13% with robotic assistance (RSG).
At baseline, there were significant differences in patient demographics and pre-operative comorbidities between the LSG and RSG cohorts (Table 1). Mean patients’ age was higher in LSG patients (p < 0.001). A higher proportion of RSG was performed in NHB patients. LSG patients were more likely to have a history of myocardial infarction (MI) (1.11% vs. 1.03%), diabetes mellitus (DM), smoking within 1 year (8.18% vs. 7.55%), and prior obesity/foregut surgery (1.35% vs. 1.08%). All other pre-existing conditions were more prevalent in the RSG cohort, including gastroesophageal reflux (GERD), hyperlipidemia (HLD), deep vein thrombosis (DVT), venous stasis, prior inferior vena cava (IVC) filter, dialysis dependent, obstructive sleep apnea (OSA), and chronic obstructive pulmonary disease (COPD) (Table 1). 1:1 caliper matching compared 74,077 LSG and 74,077 RSG cases. After matching, all demographics and pre-existing comorbidities were similar between surgical approach cohorts.
In unmatched RSG and LSG outcomes, mean operation length (91 min vs. 68 min) and hospital length of stay (1.45 days vs. 1.42 days) were longer for RSG. Leak (0.33% vs. 0.26%), SSI (0.67% vs. 0.49%), and overall morbidity (3.67% vs. 3.46%) were also higher in the RSG cohort, while venous thromboembolism (VTE) (0.51% vs. 0.50%) and mortality (0.06%) were similar, and bleeding (0.17% vs. 0.22%) lower in the RSG cohort. 1:1 caliper matching compared 148,154 RSG and LSG cases. In matched analyzed cohorts, operation length (OL) (90.68 min vs. 66.26 min, p < 0.001) and hospital postoperative length of stay (LOS) (1.40 days vs. 1.35 days, p < 0.001) remained longer in the RSG cohort. While mortality, VTE, and bleeding were similar between RSG and LSG cohorts (Table 2), leak (0.32% vs. 0.23%, p 0.001), surgical site infection (SSI) (0.64% vs. 0.478%, p < 0.001), and overall morbidity (3.3% vs 3.0%, p 0.004) remain higher with RSG.
Year-to-year outcome trends in matched LSG and RSG cohorts are detailed in Figs. 2, 3, and 4. In matched year-by-year cohort comparison, OL and LOS decreased over time for RSG, but remained longer compared to LSG (Fig. 2). Overall morbidity also decreased over time for RSG but remains higher compared to LSG (Fig. 3). In matched year-to-year comparison, leak and bleeding also decreased with RSG, while SSI remains relatively unchanged and higher in RSG (Fig. 4).
To account for possible technological advancements with robotic stapling, matched cohort analyses were stratified by operation period, comparing cases performed 2015–2018 to those performed 2019–2021. While mean difference in OL between RSG and LSG decreases between the early (27.6 min) and late (22.5 min) study periods, RSG remained associated with a longer OL (p < 0.001). Mean difference in LOS also decreased between the early (0.08 days) and late (0.04 days) study periods but remains higher for RSG (p < 0.001).
For both study periods, mortality, VTE, and bleeding were similar between LSG and RSG cohorts (Table 3). While the likelihood of bleeding was lower with RSG (OR 0.91; OR 0.76) for both study periods, the difference was not significant. In the earlier study period (2015–2018), RSG was associated with an increased likelihood of leak (OR 1.53, CI 1.17–2, p 0.002), but to a lesser extent in the later study period (OR 1.36, CI 1.01–1.82, p 0.04). Compared to the early study period (OR 1.22, CI 0.97–1.54, p 0.089), RSG seems to be increasingly associated with SSI (OR 1.46, CI 1.23–1.74, p < 0.001) in the later study period. RSG was also associated with an increased likelihood of overall morbidity in the late study period (OR 1.11, CI 1.03–1.2, p 0.007), compared to the early study period (OR 1.1, CI 1–1.2, p 0.051).
Discussion
Studies comparing RSG and LSG have shown similar mortality, but overall morbidity, some complications, OL, and LOS have remained higher in RSG, when compared to LSG [23]. The impact of robotic technological advancement, including introduction of the SureForm stapler, remains unknown. In these matched analyses of 7-year aggregate data comparing RSG and LSG, we found no significant mortality, VTE, or bleeding differences, but higher rates of leak, SSI, and overall morbidity, and longer OL and LOS associated with RSG. We also noted a year-to-year improving trend in OL, LOS, morbidity, bleeding, and leak associated with use of the robotic platform for SG. Given robotic stapling technology advancements, we presume that the early study period (2015–2018) reflects a hybrid period during which a variety of stapling techniques were used, and the later study period (2019–2021) may reflect a more consistent period with utilization of the SureForm stapler, an Intuitive Surgical Inc. proprietary device. In our matched analysis comparing the 2015 to 2018 and 2019 to 2021 cohorts, mortality, VTE, and bleeding risk remained similar between study periods, the likelihood of leak decreased, while the likelihood of SSI and morbidity increased in the 2019–2021 RSG study cohort. While mean difference in OL and LOS decreased in the 2019–2021 matched cohort compared to the 2015–2018 matched cohort, both remain longer for RSG.
Staple line leak after SG is a significant postoperative complication associated with increased morbidity and mortality [28,29,30]. In our study, while the likelihood of leak decreased between the two study periods, leak remains significantly higher in the RSG cohorts, which is consistent with previously published studies. Alizadeh et al. showed threefold increase while Moon et al. showed a twofold higher leak rate in RSG compared to LSG [22, 31]. The incidence of leaks after SG has been reported to be 0.4 to 2.4% [32,33,34]. Risk factors for leak after SG is multifactorial [28, 35] and may include patient-related variables such as male gender, higher BMI, and sleep apnea [36], surgeon’s experience [36], bougie size [36, 37], or staple utilization.
While leak rate is reported to be lower with use of staple line reinforcement and oversewing [36], there remains little understanding about the impact of actual staplers used in performing SG.
The etiology of higher leak rates in SG cases remains unclear. Given the reported technological advancement with robotic stapling, the expectation would be equivalent staple line–related complications such as bleeding and leak. However, while bleeding associated with RSG and LSG is equivalent, leak remains higher with RSG. Like laparoscopic SG, patient factors, surgeon experience, and stapler utilization may be contributing factors. Prior to availability of the SureForm stapler, an Intuitive Surgical Inc. proprietary device, RSG cases were likely performed with a variety of stapling technology, including mechanical laparoscopic staplers, and powered laparoscopic staplers requiring a bedside assistant or use of earlier generations of the robotic stapler. This variability in practice may have contributed to the higher RSG leak rate seen in our 2015–2019 study cohort (OR 1.53). There may also be other contributing factors, as studies have made associations between first assistant type and adverse outcomes in MBS [38,39,40]. The reasons for reduced risk of leak in RSG performed between 2019 and 2021 (OR 1.36) compared to 2015 and 2019 (OR 1.53) are unclear. It is possible that this may reflect stapler technology evolution and changes in utilization, including a more consistent use of the SureForm stapler, an Intuitive Surgical Inc. proprietary device. However, given the lack of stapler data points in the MBSAQIP databases, this would be an assumption not supported by data analyzed for the current study.
While leaks associated with RSG show an improving trend, it remains higher compared to LSG. There are several potential reasons for this ongoing differential outcome in leak rate between the two surgical platforms. First, RSG performed between 2015 and 2018 ranged from 6 to 10% [41] compared to 22.8% RSG performed in 2021. This significant growth in RSG may translate into new robotic surgeons who are on varying trajectory of their robotic learning curve, resulting in variability in surgeon experience that may impact outcomes. As the MBSAQIP databases provide no data on surgeon experience, our study cannot confirm a direct correlation between surgeon experience and RSG outcomes.
Prior studies have shown a clear correlation between surgeon learning curve and bariatric surgery outcomes. Surgeon’s learning curve seems to play an important role in bariatric surgery outcomes, with higher number of cases done by a surgeon associated with less operative time, complications, and overall mortality rates [42, 43]. Studies have also reported a case volume of sixty LSG cases to achieve surgeon’s proficiency and acceptable postoperative complication rates [44, 45]. Similar to LSG, RSG also has a required learning curve of about twenty cases to achieve proficiency and safe patient outcomes [46]. While surgeon’s RSG learning curve may contribute to the ongoing higher adverse outcomes compared to LSG, the MBSAQIP databases do not provide granular data on provider case volume or learning curve. Therefore, while we assume a possible relationship between surgeon experience and RSG outcomes, no one could not confirm any definitive association in our study.
In addition to the increased use of the robotic platform for sleeve gastrectomy (SG), there is also continued evolution in stapler technology that may impact outcomes of SG. While the SureForm stapler, an Intuitive Surgical proprietary device, may now be more consistently used, the MBSAQIP databases used for this study, as well as others, lack granularity about the type of staplers used, as well as the use of staple line reinforcement. Therefore, based on analysis of the MBSAQIP databases, no conclusion could be drawn about the potential impact of stapler technology evolution and utilization on SG outcomes. Prior studies have suggested that staple line reinforcement (SLR) use may be associated with lower rates of leak, hemorrhage, and overall complications [47, 48]. The type of reinforcement used may also affect leak rate, as studies found that the use of absorbable polymer membrane staple line reinforcement (APM) is associated with lower leaks compared to oversewing, bovine pericardial strips (BPS), and no reinforcement [49, 50] Given the limitations of the current data, further studies with more granular data is needed to further evaluate leak outcomes associated with RSG, compared to LSG, and any association with stapling technology or surgeon experience.
Several studies have also reported higher rates of SSI associated with RSG compared to LSG [22, 51, 52] Compared to our early study period, RSG performed between 2019 and 2021 was associated with a higher likelihood of SSI. The etiology for this remains unclear. Given the declining trend in RSG-related leaks, the steady higher rate of SSI in RSG versus LSG is unlikely to be related to leaks. Studies have suggested that there might be a learning curve effect that correlates with increased SSI outcomes. The increased growth in RSG may be associated with increased variations in practice that may increase SSI risk. Early learning curve surgeons may also correlate with longer procedure and increased SSI risk. Staple line management may also be a contributing factor. In a recent study by Bennett et al., use of staple line reinforcement was associated with reduced organ space SSI (RR, 0.68, CI 0.49–0.94), while oversewing increased SSI risk (RR, 1.70, CI 1.19–2.42) [26]. Conversely, a study conducted by Sebastian et al. did not yield statistically significant disparities in the rate of SSI between patients who underwent RSG and those who underwent LSG (p = 0.25) [53].
Differences in patient characteristics may also contribute to differences in SSI rates reported in RSG compared to LSG. In our study, we believe this to be less of a contributor as we compared matched cohorts. We do acknowledge that despite matching, SSI risk variables may have still been unaccounted for and impacted our findings. The databases used for our study also lack additional data granularity that were unaccounted for and may have contributed to the differential outcomes reported and may include but not limited to wound class and antibiotic utilization.
The higher morbidity rate in RSG cases noted in our study is also consistent with the published literature [22, 54]. The increased morbidity may be associated with the persistent higher rate of SSI, and the declining but higher rate of leaks with RSG. Both SSI and leaks are also associated with other adverse outcomes, including readmission, reintervention, and reoperation that may also correlate with morbidity [55]. The correlation between SSI and other adverse outcomes and cost is well established [56,57,58,59]. Dang et al. showed that a 50% decrease in leak rates lead to a 1% decrease in readmission rates [57]. Daigle et al. showed that SSI increased reoperation (RR = 5.2, CI: 4.1–6.6) and readmission (RR = 3.7, CI: 3.2–4.3) risk, and postoperative leak also has a significant impact on reoperation (RR = 40.3, CI: 35.7–45.5) and readmission [58] (RR = 14.5, CI: 13.1–16) risk, as well as costs of care [59].
While our study shows the mean difference in OL time between RSG and LSG decreased between the early and late study periods, OL for RSG remains longer, which is consistent with prior studies [19, 21, 60, 61]. This may have implications for increased cost [51, 62, 63], and other adverse patient outcomes such as venous thromboembolism (VTE) [64]. There remains a need for more robust analysis to determine differential cost of care associated with RSG compared to LSG. The currently ongoing ROBOCOSTES trial may provide future insight [65]. While prolong MBS has been associated with increased VTE risk, the differences noted between RSG and LSG OL did not correlate with increase VTE risk in our study, which in consistent with studies by Vosburg et al. [66] and Sebastian et al. [53].
Regarding LOS, the available literature presents conflicting results regarding the postoperative LOS associated with RSG versus LSG [14, 19, 21, 67, 68]. While the mean difference in LOS reduced between the two time periods in our study, LOS remains longer for RSG. Given the marginal difference in LOS, the clinical and cost of care significance remains unclear. Nonetheless, it is consistent with other studies showing longer LOS associated with RSG [14, 19, 24, 69]. Not all comparative studies have shown this result, as a study by Alizadeh et al. [22] demonstrated no significant difference in LOS between RSG and LSG.
This study shows that RSG and LSG are both safe with no mortality difference. However, the higher morbidity, leak, and SSI associated with RSG suggest that it may not be as safe as LSG. From this database analysis, it remains unclear what impact the recent significant growth in utilization of the robotic platform for sleeve gastrectomy has on current outcomes and requires analysis of more granular databases to determine. In addition to the higher morbidity, leak, and SSI rates, the higher cost associated with RSG must also be considered in the decision to utilize the platform for SG cases.
Our study has several limitations to highlight. Firstly, our analysis is limited to short-term outcomes and studies focusing on long-term outcomes are also needed. The lack of granular data in the MBSAQIP registry about surgeon experience and stapler utilized represents a notable limitation to this study as well as other studies, as there are potential confounders that may not have been accounted for. Previous research has established that surgeon experience and case volume can have a significant effect on bariatric surgery outcomes, and the absence of this information in the current dataset prevents an accurate assessment of their impact on the outcomes under investigation. Additionally, as a retrospective analysis of clinical data, this study is susceptible to biases that are associated with such analyses. The timeliness and completeness of data entry by bariatric Clinical Nurse Reviewers can impact data quality and introduce limitations to any analysis utilizing this database. Despite these limitations, this study provides valuable insights into the outcomes associated with RSG compared to LSG and highlights the need for increased granular data to ensure appropriate comparative analysis of these surgical platforms.
Conclusion
Robotic and laparoscopic sleeve gastrectomy are safe with similar mortality. However, in this analysis of the MBSAQIP databases over two time periods, RSG is associated with higher rates of morbidity, leak, and surgical site infection, as well as higher cost associated with longer operative duration and hospital length of stay, compared to LSG. It remains unclear how the increased utilization of the robotic platform for sleeve gastrectomy has contributed to these findings, including how current robotic metabolic surgery growth may have impacted surgeon’s experience and learning curve, and possible outcomes observed in this study.
Data Availability
Data is from national ACS-MBSAQIP data registry and will not be available.
References
Clapp B, et al. American Society for Metabolic and Bariatric Surgery 2022 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2024;20(5):425–31.
Sánchez-Santos R, et al. Short- and mid-term outcomes of sleeve gastrectomy for morbid obesity: the experience of the Spanish National Registry. Obes Surg. 2009;19(9):1203–10.
Gagner M, et al. The Second International Consensus Summit for Sleeve Gastrectomy, March 19–21, 2009. Surg Obes Relat Dis. 2009;5(4):476–85.
Singhal R, et al. 30-day morbidity and mortality of sleeve gastrectomy, Roux-en-Y gastric bypass and one anastomosis gastric bypass: a propensity score-matched analysis of the GENEVA data. Int J Obes. 2022;46(4):750–7.
Soto FC, et al. Sleeve gastrectomy in the elderly: a safe and effective procedure with minimal morbidity and mortality. Obes Surg. 2013;23(9):1445–9.
Spaniolas K, et al. Early morbidity and mortality of laparoscopic sleeve gastrectomy and gastric bypass in the elderly: a NSQIP analysis. Surg Obes Relat Dis. 2014;10(4):584–8.
Ben-Porat T, et al. Weight loss outcomes and lifestyle patterns following sleeve gastrectomy: an 8-year retrospective study of 212 patients. Obes Surg. 2021;31(11):4836–45.
Alger-Mayer S, Polimeni JM, Malone M. Preoperative weight loss as a predictor of long-term success following Roux-en-Y gastric bypass. Obes Surg. 2008;18(7):772–5.
Diamantis T, et al. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83.
Alqahtani AR, Elahmedi MO, Al Qahtani A. Co-morbidity resolution in morbidly obese children and adolescents undergoing sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(5):842–50.
Rodríguez-Otero Luppi C, et al. Laparoscopic sleeve gastrectomy in patients over 60 years: impact of age on weight loss and co-morbidity improvement. Surg Obes Relat Dis. 2015;11(2):296–301.
Todkar JS, et al. Long-term effects of laparoscopic sleeve gastrectomy in morbidly obese subjects with type 2 diabetes mellitus. Surg Obes Relat Dis. 2010;6(2):142–5.
Chopra A, et al. Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc. 2012;26(3):831–7.
Magouliotis DE, et al. Robotic versus laparoscopic sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis. Obes Surg. 2017;27(1):245–53.
Dimou FM, et al. Understanding the current role of robotic-assisted bariatric surgery. Obes Surg. 2021;31(7):3130–7.
Scarritt T, et al. Trends in utilization and perioperative outcomes in robotic-assisted bariatric surgery using the MBSAQIP database: a 4-year analysis. Obes Surg. 2021;31(2):854–61.
Frezza EE, et al. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19(6):684–7.
Lalor PF, et al. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2008;4(1):33–8.
Romero RJ, et al. Robotic sleeve gastrectomy: experience of 134 cases and comparison with a systematic review of the laparoscopic approach. Obes Surg. 2013;23(11):1743–52.
Pepper VK, et al. Robotic vs. laparoscopic sleeve gastrectomy in adolescents; reality or hype. Obes Surg. 2016;26(8):1912–7.
Elli E, et al. Laparoscopic and robotic sleeve gastrectomy: short- and long-term results. Obes Surg. 2015;25(6):967–74.
Fazl Alizadeh R, et al. Robotic versus laparoscopic sleeve gastrectomy: a MBSAQIP analysis. Surg Endosc. 2019;33(3):917–22.
Li K, et al. Robotic versus laparoscopic bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2016;26(12):3031–44.
Nasser H, et al. Perioperative outcomes of robotic versus laparoscopic sleeve gastrectomy in the super-obese. J Surg Res. 2020;249:34–41.
Pastrana M, et al. Evolution of outcomes of robotic bariatric surgery: first report based on MBSAQIP database. Surg Obes Relat Dis. 2020;16(7):916–22.
Bennett WC, et al. Comparison of robot-assisted sleeve gastrectomy outcomes in multiple staple line treatment modalities from 2015 to 2019: a 5-year propensity score-adjusted MBSAQIP® analysis. Surg Endosc. 2023;37(2):1401–11.
Bindal V, Goel T, Panday D, Gupta S. Robotic staplers in bariatric surgery: our short-term experience. Int J Adv Robot Innov Syst. 2023;1(1):25–8.
Benedix F, et al. Staple line leak after primary sleeve gastrectomy—risk factors and mid-term results: do patients still benefit from the weight loss procedure? Obes Surg. 2017;27(7):1780–8.
Márquez MF, et al. Gastric leak after laparoscopic sleeve gastrectomy. Obes Surg. 2010;20(9):1306–11.
Hughes D, Hughes I, Khanna A. Management of staple line leaks following sleeve gastrectomy—a systematic review. Obes Surg. 2019;29(9):2759–72.
Moon RC, et al. Management of staple line leaks following sleeve gastrectomy. Surg Obes Relat Dis. 2015;11(1):54–9.
Bashah M, Khidir N, El-Matbouly M. Management of leak after sleeve gastrectomy: outcomes of 73 cases, treatment algorithm and predictors of resolution. Obes Surg. 2020;30(2):515–20.
Gagner M. Decreased incidence of leaks after sleeve gastrectomy and improved treatments. Surg Obes Relat Dis. 2014;10(4):611–2.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26(6):1509–15.
Iossa A, et al. Leaks after laparoscopic sleeve gastrectomy: overview of pathogenesis and risk factors. Langenbecks Arch Surg. 2016;401(6):757–66.
Sánchez-Santos R, et al. Prognostic factors for morbimortality in sleeve gastrectomy. the importance of the learning curve. A Spanish-Portuguese multicenter study. Obes Surg. 2016;26(12):2829–36.
Yuval JB, et al. The effects of bougie caliber on leaks and excess weight loss following laparoscopic sleeve gastrectomy. Is There an Ideal Bougie Size? Obes Surg. 2013;23(10):1685–91.
Coker, A., et al., Do advances in technology translate to improved outcomes? Comparing robotic bariatric surgery outcomes over two-time intervals utilizing the MBSAQIP database. Surgical Endoscopy, 2023
Edwards MA, Terhaar H, Spaulding A. Resident first assistance in bariatric surgery: do patients pay a price? Surg Obes Relat Dis. 2022;18(6):738–46.
First assistant level of training as a predictor of perioperative outcomes in primarybariatric surgery. Bariatric Surgical Practice and Patient Care. 0(0): p. null.
Bauerle WB, et al. Current trends in the utilization of a robotic approach in the field of bariatric surgery. Obes Surg. 2023;33(2):482–91.
Doumouras, A.G., et al., Mastery in bariatric surgery: the long-term surgeon learning curve of Roux-en-Y gastric bypass. Annals of Surgery, 2018; 267(3)
Shin RB. Evaluation of the learning curve for laparoscopic Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2005;1(2):91–4.
Carandina S, et al. Laparoscopic sleeve gastrectomy learning curve: clinical and economical impact. Obes Surg. 2019;29(1):143–8.
Zacharoulis D, et al. Influence of the learning curve on safety and efficiency of laparoscopic sleeve gastrectomy. Obes Surg. 2012;22(3):411–5.
Vilallonga R, et al. The initial learning curve for robot-assisted sleeve gastrectomy: a surgeon’s experience while introducing the robotic technology in a bariatric surgery department. Minim Invasive Surg. 2012;2012:347131.
Demeusy A, Sill A, Averbach A. Current role of staple line reinforcement in 30-day outcomes of primary laparoscopic sleeve gastrectomy: an analysis of MBSAQIP data, 2015–2016 PUF. Surg Obes Relat Dis. 2018;14(10):1454–61.
Wang Z, et al. The efficacy of staple line reinforcement during laparoscopic sleeve gastrectomy: a meta-analysis of randomized controlled trials. Int J Surg. 2016;25:145–52.
Gagner M, Kemmeter P. Comparison of laparoscopic sleeve gastrectomy leak rates in five staple-line reinforcement options: a systematic review. Surg Endosc. 2020;34(1):396–407.
Gagner M, Buchwald JN. Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis. 2014;10(4):713–23.
Villamere J, et al. Utilization and outcome of laparoscopic versus robotic general and bariatric surgical procedures at Academic Medical Centers. Surg Endosc. 2015;29(7):1729–36.
Papasavas P, et al. Robot-assisted sleeve gastrectomy and Roux-en-y gastric bypass: results from the metabolic and bariatric surgery accreditation and quality improvement program data registry. Surg Obes Relat Dis. 2019;15(8):1281–90.
Sebastian R, et al. Robot-assisted versus laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a propensity score-matched comparative analysis using the 2015–2016 MBSAQIP database. Surg Endosc. 2019;33(5):1600–12.
Nasser H, et al. Comparative analysis of robotic versus laparoscopic revisional bariatric surgery: perioperative outcomes from the MBSAQIP database. Surg Obes Relat Dis. 2020;16(3):397–405.
Kushner BS, et al. Infection prevention plan to decrease surgical site infections in bariatric surgery patients. Surg Endosc. 2022;36(4):2582–90.
Garg T, et al. National prevalence, causes, and risk factors for bariatric surgery readmissions. Am J Surg. 2016;212(1):76–80.
Dang JT, et al. Trends and outcomes of laparoscopic sleeve gastrectomy between 2015 and 2018 in the USA and Canada. Obes Surg. 2021;31(2):675–81.
Daigle CR, et al. Which postoperative complications matter most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcomes. Surg Obes Relat Dis. 2018;14(5):652–7.
Bransen J, et al. Costs of leaks and bleeding after sleeve gastrectomies. Obes Surg. 2015;25(10):1767–71.
Ecker BL, et al. Resident education in robotic-assisted vertical sleeve gastrectomy: outcomes and cost-analysis of 411 consecutive cases. Surg Obes Relat Dis. 2016;12(2):313–20.
Diamantis T, et al. Initial experience with robotic sleeve gastrectomy for morbid obesity. Obes Surg. 2011;21(8):1172–9.
Wilson EB, Sudan R. The evolution of robotic bariatric surgery. World J Surg. 2013;37(12):2756–60.
Schraibman V, et al. Comparison of the morbidity, weight loss, and relative costs between robotic and laparoscopic sleeve gastrectomy for the treatment of obesity in Brazil. Obes Surg. 2014;24(9):1420–4.
Chao GF, et al. Venous thromboembolism: risk factors in the sleeve gastrectomy era. Surg Obes Relat Dis. 2021;17(11):1905–11.
Ielpo, B., et al., Cost-Effectiveness of robotic vs. laparoscopic surgery for different surgical procedures: protocol for a prospective, multicentric study (ROBOCOSTES). Front Surg, 2022. 9
Wesley Vosburg R, Haque O, Roth E. Robotic vs. laparoscopic metabolic and bariatric surgery, outcomes over 5 years in nearly 800,000 patients. Obes Surg. 2022;32(7):2341–8.
Kannan U, et al. Laparoscopic hand-assisted versus robotic-assisted laparoscopic sleeve gastrectomy: experience of 103 consecutive cases. Surg Obes Relat Dis. 2016;12(1):94–9.
Robot-assisted sleeve gastrectomy for super-morbidly obese patients. J LaparoendoscAdv Surg Tech, 2011; 21(4): p. 295-299
Moon RC, et al. Robot-assisted versus laparoscopic sleeve gastrectomy: learning curve, perioperative, and short-term outcomes. Obes Surg. 2016;26(10):2463–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to Participate
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• RSG versus LSG was associated with longer operation duration.
• RSG versus LSG was associated with longer hospital stay.
• RSG and LSG had similar mortality rates.
• Leak rate improved over time but remained higher for RSG versus LSG.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Edwards, M.A., Falstin, M., Alomari, M. et al. Robotic Versus Laparoscopic Sleeve Gastrectomy Outcome Trends Over Time: Are We Improving?. OBES SURG 34, 2596–2606 (2024). https://doi.org/10.1007/s11695-024-07334-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07334-x