Abstract
Background
Bariatric surgery is an efficient procedure for remission of type 2 diabetes (T2DM) in morbid obesity. However, in Asian countries, mean body mass index (BMI) of T2DM patients is about 25 kg/m2. Various data on patients undergoing gastric bypass surgery showed that control of T2DM after surgery occurs rapidly and somewhat independent to weight loss. We hypothesized that in non-obese patients with T2DM, the glycemic control would be achieved as a consequence of gastric bypass surgery.
Methods
From September 2009, the 172 patients have had laparoscopic single anastomosis gastric bypass (LSAGB) surgery. Among them, 107 patients have been followed up more than 1 year. We analyzed the dataset of these patients. Values related to diabetes were measured before and 1, 2, and 3 years after the surgery.
Results
The mean BMI decreased during the first year after the surgery but plateaued after that. The mean glycosylated hemoglobin level decreased continuously. The mean fasting and postglucose loading plasma glucose level also decreased.
Conclusion
After LSAGB surgery in non-obese T2DM patients, the control of T2DM was possible safely and effectively. However, longer follow-up with matched control group is essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a chronic debilitating metabolic disease which leads to a number of serious complications and mortality. Its representative causes are impairment of insulin release and/or insulin resistance. Ninety percent of diabetes mellitus are type 2, which occur mainly due to insulin resistance [1]. Type 2 diabetes mellitus (T2DM) has become the number one worldwide health problem because of its rapid increase, chronic course, and excess waste of time and money to control.
In Western countries, the association between obesity and T2DM is well-established because 90 % of patients with T2DM have excess body weight [2]. However, according to a recent survey by the Ministry of Health and Welfare of Korea, the mean body mass index (BMI) of T2DM patients in Korea is 24.9 ± 3.3 kg/m2 (the mean BMI of male T2DM patients is 24.3 kg/m2; the mean BMI of female T2DM patients is 25.5 kg/m2) [3]. That is, the majority of T2DM patients in Korea are not very obese. However, although not in the obese category (BMI ≤ 30 kg/m2), someone with BMI of 25 kg/m2 has eight times (female) or two times (male) higher diabetic risk than someone with BMI less than 22 kg/m2 [4, 5]. The reasons for this difference are the following: first, due to rapid economic development, there have been rapid changes in eating habits and lifestyles in Asia. Second, Asian people are more prone to central obesity, so they are more susceptible to insulin resistance. As a result, Asians tend to be vulnerable to insulin resistance. Also, Asians have weaker pancreatic islet cells than other ethnic groups [6, 7].
Despite multidisciplinary approaches to control T2DM which include intensive lifestyle intervention (ILI), oral hypoglycemic agents (OHA), and insulin, the effects are not satisfying [8]. In Korea, the rate of controlled T2DM (glycosylated hemoglobin (HbA1C) <6.5 %) among the patients who receive medical therapies are only 24.8 % [3].
Some types of weight loss surgery, especially Roux-en-Y gastric bypass (RYGB) and biliopancreatic diversion (BPD), generally result in a loss of about 70 % excess body weight (68.1 and 72 %, respectively) and cure diabetes in more than 80 % of patients [9]. It has been noted that glycemic control after weight loss surgery often occurs long before a significant weight loss [10]. The recovery of T2DM after these surgeries might have been related to other factors in addition to weight loss.
However, these bariatric procedures are somewhat complex to perform. In 2011, the International Diabetes Federation stated that the simplicity and reversibility of a procedure should be considered [11].
We modified the mini-gastric bypass (MGB) surgery by Dr. Rutledge [12]. We preserve the gastric fundus in order not to reduce the amount of ingested food and to secure simplicity and reversibility of the procedure. We made a single anastomosis between the stomach and small bowel which is 200 cm distal from Treitz ligament to exclude the foregut from the food passage and for nutrients to arrive in the distal part of the intestine faster. We hypothesized that the rerouting of the gastrointestinal tract, exclusion of the duodenum and proximal part of the jejunum, and rapid transit of food to the distal part of the small intestine might affect glucose metabolism and can lower the plasma glucose in non-obese T2DM patients [13–15].
We aimed to investigate changes of glucose metabolism in non-obese T2DM patients after they have a laparoscopic single anastomosis gastric bypass (LSAGB) surgery.
Patients and Methods
The inclusion criteria for patients in this prospective study were the following: age 20–65 years, BMI lower than 30 kg/m2, fasting C-peptide ≥ 1.0 ng/ml, and HbA1C > 7.0 %. We have not considered the duration of the diabetes. The exclusion criteria were type 1 diabetes mellitus, any contraindications to general anesthesia, history of previous gastrointestinal surgery, and the inability to comply with study protocols or regular follow-up. All patients gave informed consent and understood that this surgery was not an established therapeutic modality of their diabetes. This prospective study has been approved by the Institutional Review Board for Human Research of Soonchunhyang University Hospital (No. 2010-47, 2011-69).
From September 2009, the 172 patients have been enrolled in this study. Among these patients, 107 patients have been followed up for more than 1 year. We analyzed the dataset of these patients.
We progressed through the postoperative course in the standardized manner in most patients after the surgery: leak test with blue dye and upper gastrointestinal (UGI) series with water soluble contrast media on postoperative day 1, and if there is no finding of leak, we start the patient on a diet. The patients have sips of water after the negative leak test and are put on a liquid diet at dinner. The patients resume a soft diet on postoperative day 2 and are discharged on postoperative day 4. Due to distance, some patients chose to go home on postoperative day 7.
If someone had a random blood glucose level more than 200 mg/dL owing to the postsurgical stress during the hospital stay, he or she got insulin sliding to lower the chance of the postoperative surgical site infection.
After the discharge, we followed the patients regularly during the first week, first month, third month, sixth month, twelfth month, and yearly through the outpatient department with serial laboratory and/or imaging studies.
Our therapeutic target has been HbA1C level of lower than 7 % according to the criteria of the American Diabetes Association (ADA) [16].
Laparoscopic Single Anastomosis Gastric Bypass
All patients underwent a LSAGB with five-trocar method: four 12-mm trocars and one 5-mm trocar. At first, the stomach was divided by using endo-staplers (Endo GIA™ 60 mm Articulating Medium/Thick Reload with Tri-Staple™ Technology, COVIDIEN Autosuture, Mansfield, MA, USA) along the lesser curvature from 2 cm proximal to the pylorus aiming to the gastric fundus. The volume of the gastric pouch was individually adjusted according to the patient’s BMI—<25 or ≥ 25 kg/m2—by adjusting the size of the gastric body. However, we preserve the fundus in every case. After the formation of the vertical gastric pouch, an anchoring suture was laid between the middle part of the gastric pouch and the afferent limb for acute angulation of the afferent limb. And then, the small intestine which is 200 cm distal from the ligament of Treitz was anastomosed to the distal portion of the gastric pouch by using an endo-stapler (Endo GIA™ 45 mm Articulating Vascular/Medium Reload with Tri-Staple™ Technology, COVIDIEN Autosuture, Mansfield, MA, USA) in side-to-side, ante-colic, isoperistaltic fashion, and consequently, part of the gastric antrum and the body, entire duodenum including the pylorus, and proximal jejunum were bypassed (Fig. 1). The stapler insertion site was manually sutured in a continuous fashion. As a result, a parallel line between the gastric pouch and the efferent limb could be maintained. In addition, the holes for stapler insertion were made at the anterior surface of the stomach and the posterior surface of the jejunum. This structure enabled the physiologic flow, that is, less reverse flow toward the afferent limb or reflux toward the gastric pouch. An intraoperative leak test was performed using blue dye and air to confirm negative leak at the anastomosis site.
Statistical Analysis
Data are presented as means ± SD unless otherwise stated. The paired t test was used to compare data from before and after the surgery. Statistical significance was generally set at p values <0.05. However, we adjusted statistical significance when we compared each mean value with the previous value after Bonferroni correction. Data were analyzed using SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Subject Characteristics
Subject characteristics are shown in Table 1. The mean age was 46 ± 11 years. There were 53 female patients and 54 male patients, with type 2 diabetes of 9.6 ± 5.2-year duration. The mean preoperative BMI was 25.3 ± 3.2 kg/m2. The mean glycosylated hemoglobin (HbA1C) was 9.0 ± 1.7 %. The mean fasting plasma glucose (FPG) was 188.9 ± 63.9 mg/dL, and 2 hours after glucose (75 g) loading, the plasma glucose level was 317.0 ± 94.9 mg/dL. The mean C-peptide level was 2.8 ± 1.2 ng/mL. The 19 patients were treated with insulin and 63 with oral hypoglycemic agent (OHA). Seventeen patients were treated with both insulin and OHA. Others had no medication for reasons of noncompliance, side effects, or had herbal medication.
Perioperative Outcomes
The perioperative outcomes are shown in Table 2. The mean operation time was 87 ± 34 min. The mean postoperative hospital stay was 4.5 ± 1.0 days (range 3 to 7 days). There were five minor early complications within postoperative day 30. There were two cases of postoperative bleeding, one case of efferent stasis, and one case of infected fluid collection. All these events were managed conservatively, i.e., transfusion and observation, hydration and NPO, and percutaneous drainage (PCD). There was one anastomotic leakage, and therefore, enterocutaneous fistula occurred, which failed to be controlled with conservative management. We reoperated on the patient and converted to Roux-en-Y gastrojejunostomy. There was a conversion to open surgery because of postoperative—previous nephrectomy—adhesion. There were no mortalities.
Changes in Outcome Values
These changes are shown in Table 3.
-
1.
Changes in BMI
-
The patients’ BMI was reduced significantly after the surgery during the first year. The mean BMI values between pre- and post-1, 2, and 3 years after the LSAGB were 25.3, 22.9, 22.5, and 22.4 kg/m2, respectively. There was a statistical significance at only a year after the surgery. After that, the BMI almost plateaued.
-
There has been no patient who has gained weight during the first year after the surgery. After more than 1 year, there have been a total of 34 patients having gained weight. Among these patients, there have been nine patients (26.5 %) who have experienced continuous decreased HbA1C despite weight gain. There also have been 17 patients (50 %) who have shown increased HbA1C a bit but less than 6.5 %, and 8 patients (23.5 %) have shown increased HbA1C more than 6.5 % along with weight gain. In other words, 76.5 % of the patients who have experienced weight gain have shown stably maintained HbA1C level less than 6.5 %.
-
-
2.
Changes in glucose parameters—HbA1C, fasting, and 2-h postprandial serum glucose
-
The mean HbA1C decreased continuously. Its values were 9.0, 6.9, 6.7, and 6.0 %, respectively, at preoperation, 1 year, 2 years, and 3 years after the surgery. Between the second and third year, although the changes in values seemed to decrease significantly (from 6.7 to 6.0 %), there was no actual significance (p = 0.584). The percentages of subjects who have met the target (HbA1C < 7 %) are 53, 63 and 90 % in the first, second, and third years after the surgery.
-
The mean fasting glucose also decreased continuously. The mean 2-h plasma glucose after 75-g glucose loading also seemed to decrease except the value of the second year. This was because only a few 2-h postglucose loading plasma glucose levels were measured. There were also tendencies of more decreases in values between the second and third year. However, there was no statistical significance (p = 0.571).
-
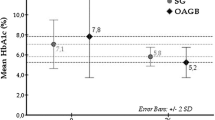
We compared the results between those patients who were on insulin and those who were not. Interestingly, there were no differences between groups which had been treated with insulin or not before the surgery. One year after the surgery, mean HbA1C of patients who had been treated with insulin was 7.1 % and mean HbA1C of those who had not been was 6.9 % (p = 0.654). Two years after the surgery, mean HbA1C of patients who had been treated with insulin was 6.8 % and mean HbA1C of those who had not been was 6.5 % (p = 0.577). At third year after the surgery, mean HbA1c of patients who had been treated with insulin or not was 6.1 and 5.6 %, respectively (p = 0.346).
-
-
3.
Changes in insulin and C-peptide
-
The mean values of insulin and C-peptide seemed to decrease slightly. However, there was no significance or large difference.
-
-
4.
Changes in insulin resistance (HOMA-IR)
-
The mean value of homeostatic model assessment of insulin resistance (HOMA-IR) was 5.18 ± 2.98 preoperatively. After the surgery, the mean values of HOMA-IR decreased continuously, 3.57 ± 2.21, 2.32 ± 1.22, and 2.08 ± 0.65 in the first, second, and third years after the surgery (p < 0.001, p = 0.893, and p = 0.86, respectively).
-
Late Complications (After More Than 1 Year)
The most common complications were marginal ulcers (22 cases), which are diagnosed with gastrofiberscope. Among them, two subjects had reoperations (conversion to Roux-en-Y) for stenosis and perforation. The rest of the subjects were easily managed with proton pump inhibitor.
The second most common complications were iron deficiency anemias (12 cases). We managed this with IV or oral iron supplements.
A 54-year-old woman suffered from stomatitis, odynophagia, and desquamation on her hands and feet beginning about 1 year after the surgery. We checked her laboratory profile but could not find abnormalities except her serum zinc level. Her zinc level decreased significantly. We managed her with IV trace elements with amino acid infusions, and her symptoms improved.
Discussion
Improvement of metabolic syndrome including a glycemic control has been reported in morbidly obese patients after bariatric surgery such as RYGB or BPD [17, 18]. It has long been hypothesized that there might be an “anti-diabetic mechanism” of the surgery which works independently to the weight loss because the glycemic control has occurred immediately after the surgery before a significant weight loss [10, 13–15].
There are several possible mechanisms of action of gastrointestinal manipulation to remit the type 2 diabetes [19–21]: (1) increased insulin sensitivity after caloric restriction and/or weight loss, (2) decreased secretion of ghrelin and anti-incretin factor (also known as the factor X or Rubino’s factor), and recovery of stimulated response of K-cells due to the exclusion of the foregut from exposure to nutrients as a result of rerouting of the gastrointestinal tract, (3) improvement of the action of glucose-dependent insulinotropic polypeptide (GIP), (4) increased secretion of glucagon-like peptide 1 (GLP-1) as a result of early exposure of nutrients in the hindgut, therefore increased secretion of insulin, and (5) changes in the metabolic homeostasis and/or sensitivity to OHAs as a result of rerouting of the gastrointestinal tract.
Several studies have focused on the changes in secretion and action of the incretin after rerouting of the gastrointestinal tract and have reported favorable results [22–26]. The enteroinsular axis describes the connection between the gut and the pancreatic islets. This axis encompasses nutrient, neural, and hormonal signals from the gut to the islets. The hormonal part of the axis, known as the “incretin,” is released by nutrients, and it stimulates the secretion of insulin. The two main incretins are GIP from the foregut and GLP-1 from the hindgut [27, 28].
Both GLP-1 and GIP affect meal-related insulin secretion [29, 30]. GLP-1 is secreted by L-cells of the distal ileum. In the pancreas, GLP-1 is a powerful secretagogue of the β cells for the glucose-dependent secretion of insulin (insulinotropic activity). GLP-1 also delays gastric emptying, decreases appetite, inhibits glucagon, and may improve insulin sensitivity, having anti-diabetogenic effects [31, 32]. GIP is secreted by enteroendocrine K-cells of the proximal gut. The GIP has additive insulinotropic effects during hyperglycemia [33]. In normal subjects, release of both GLP-1 and GIP contributes to stimulation of insulin secretion after a meal and to glucose storage in the peripheral tissues. However, in all T2DM patients, the loss of this effect, defined as enteroinsular impairment, is characteristic [34]. In type 2 diabetic patients, the action of GIP is blunted. It has been hypothesized that high amount of easily absorbable (high glycemic index) nutrients overstimulate the proximal gut; therefore, the receptor of GIP is downregulated [35, 36]. There is relatively less available nutrients in the distal gut. In type 2 diabetic patients, serum GIP level is increased and serum GLP-1 level is decreased [37, 38].
We modified the size of gastric pouch, the method of anastomosis, and the length of bypassed limb of the original MGB procedure [12]. There have been several reports on outcomes of MGB in obese patients [12, 39–42]. These reports have shown that MGB is a relatively simple and reversible procedure with good weight loss, reduction of comorbidities such as T2DM and dyslipidemia, and acceptable morbidity rate. MGB causes weight loss and metabolic effects by both restrictive and more malabsorptive mechanisms. And this procedure is easy to learn, fast to perform, and safe compared to other bariatric procedures because of just single anastomosis, lower location of anastomosis, better blood supply to gastric tube, and needless of mesenteric division.
Lee et al. and Garcia-Caballero et al. have studied outcomes of procedures which modified MGB for non-obese T2DM patients. They modified the size of gastric tube or the length of bypassed small bowel to draw more metabolic effects through malabsorptive mechanism of this procedure. They reported good outcomes as well [25, 43].
On the other hand, although many studies have revealed that MGB and its modified procedures are safe and effective, there have been reports on drawbacks of these procedures. Dang et al. reported a case about a patient who needed revisional surgery after MGB because of protein malnutrition, vitamin deficiencies, or intractable bile reflux [44]. In a multicenter review of their medical record, a total of 32 patients were identified undergoing surgical revision after a MGB procedure because of the foregoing reasons [45]. However, they did not state the total number of patients undergoing MGB procedure. According to the literatures, there have been about 5 % of bile refluxes or marginal ulcers after MGB. Proponents of the procedure hypothesize that they can reduce these complications by modifying the procedure a little such as one or two anchoring sutures, parallel physiologic arrangement of gastrojejunostomy.
It is difficult to compare our outcomes exactly with other reports of MGB because of the differences in detailed procedure—the size of gastric pouch, the method of anastomosis, or the length of bypassed limb—in patient’s BMI, and so on.
We focused on the complete foregut exclusion and early hindgut exposure while performing the surgery and therefore modified MGB as a simple and effective procedure. There are no patients who have shown severe weight loss or weight loss below the underweight category (BMI < 18.5 kg/m2) although there has been significant weight loss during the first year after the surgery. The reason for this weight loss could be due to the malabsorptive mechanism of bypassing the 200-cm-small intestine. However, patients could have the same amount of food with preoperative period in 2 to 4 weeks after the surgery. After more than 1 year of the surgery, the mean BMI was plateaued as there might have been some adaptive mechanisms. We identified widened efferent loops in reoperated cases.
The levels of the fasting plasma glucose, 2-hour postglucose loading plasma glucose, and HbA1C decreased continuously despite of the plateaued BMI. The levels of the fasting C-peptide and insulin also showed decreasing pattern, but there were no statistical significances. We have not measured postglucose loading C-peptide or insulin levels, and this is one of the limitations of this study.
We have considered the possibility of late response because the values of HbA1C and plasma glucose level decreased more between the second and third year after the surgery. It could be explained in the way that the patients who have less beta cell mass may take more time to have enough beta cell mass in response to incretin. However, there are no statistical significances between the second and third year after the surgery; it could be explained with small subject number.
In addition, early after the surgery, there can be shown “short gut effect” such as loose stool, frequent bowel movements, or even weight loss because of shortening of small bowel which absorbs digested nutrients. It is known that it takes about more than 6 months to adapt to such a circumstance by increasing the number of villi or widening the surface area of small bowel. Thus, it was possible to have shown metabolic effects without further weight loss after a certain period of time. Besides, as mentioned above, the possible reason for more improvement in glucose control without further weight loss between the second and third year is that it might take some period of time for pancreatic beta cells to proliferate on the basis of recovery of incretin imbalance. That is, there is a highly possible mechanism which improves glucose metabolism by recovering the function and number of beta cells and by improving insulin resistance regardless of weight change a bit late after the surgery.
The HOMA-IR also decreased continuously. It could be thought as improvement of the insulin resistance. However, we have to identify whether there are any changes in early and late phase insulin secretion after the glucose loading or mixed meal test. We performed the pilot study about incretin and insulin secretion after the LSAGB in 12 subjects. All of the patients showed significant increased insulin secretion, significant decreased GIP secretion, and significant increased GLP-1 secretion after 75-g glucose loading 1 month after the surgery (unpublished data). Although it is difficult to generalize this result because of the limitations of the study—small subject numbers, no control group, and early period after the surgery (only 1 month after the surgery)—this result suggests the possibility of increase in insulin secretion in response to the glucose load after the LSAGB surgery.
One issue of concern about the LSAGB is bile reflux from the loop-type anastomosis. Although there have been concerns that the bile stimulation to gastric mucosa could be ulcerogenic or even oncogenic, the loop-type gastrojejunostomy has been one of the current methods of anastomosis after the conventional gastric surgeries. Also, as mentioned above, we made the anchoring suture at the mid-portion of the gastric pouch with the jejunum, so that we could make parallel line between the pouch and the efferent loop. We reduced bile refluxes through more physiologic position of the anastomosis and direction of bile flow—lower position of the anastomosis inside the abdomen and anastomosis between the anterior aspect of the stomach and the posterior aspect of the jejunum. Although the Braun anastomosis prevents bile reflux toward the stomach, the foregut exclusion cannot be achieved because of the backward movement of ingested food bolus, and the possibility of morbidity can increase as the number of anastomosis is increased. However, symptomatic patients should be managed with acid-lowering agents such as proton pump inhibitors and be closely followed up with serial gastrofiberscopy (GFS).
There has also been a concern about remnant—bypassed—gastric cancer. However, there have been only several case reports about the remnant gastric cancer. Surgeons can consider the evaluation of the remnant stomach with the use of the retrograde enteroscope if there are experienced hands in their institute and consider serial imaging study for surveillance. Considering that the risk of the gastric cancer is more related with environmental factors such as processed food, smoking, etc., the risk of the gastric cancer might be higher in the gastric pouch than the bypassed stomach. However, the surgery that leaves the remnant stomach has to be thought twice if the patient corresponds to high risk group of gastric cancer—the presence of the premalignant lesions on preoperative GFS, positive result of H. pylori, and/or positive family history of gastric cancer.
The increased risk of the marginal ulcer after the gastrointestinal anastomosis is related to non-absorbable suture mate rials, smoking and other situations with high amount of acid secretion, etc. [46]. The marginal ulcer can occur in any gastrointestinal procedures such as standard Whipple’s operations, pylorus-preserving pancreaticoduodenectomies, or RYGBs as well as LSAGB or billroth II gastrojejunostomies. There have been 22 cases of marginal ulcers after the surgery. Every 22 patients were smokers and had the surgery with the use of non-absorbable suture materials. After switching to use of absorbable suture material for the procedure and educating the patients to quit smoking prior to surgery, the incidence of the marginal ulcer decreased.
The iron deficiency anemia or megaloblastic anemia can occur as a result of decrease in absorption of the iron or vitamin B12/folate in the proximal gut. However, there have been no severe anemias that need to have transfusion in our subjects. And patients showed good response to iron supplementation. And we have not experienced any megaloblastic anemias so far.
Every 36 patients who had had insulin to control their blood sugar could stop the insulin injection. Although there has been a group of patients who have had intermittent OHAs after the surgery, the number of the patients decreased as time went on. There could have been changes in plasma level or bioavailabilities of OHAs after the surgery in response to the change of the gastrointestinal tract [20, 21]. Future studies should be planned to reveal the changes of action, metabolism, and requirement of OHAs.
Possible mechanisms of failing in decreasing of plasma glucose level after the surgery are the following: almost absent viable beta cell mass because of the severe T2DM (longer duration of the disease and severe exhausted beta cell mass), the action of glucagonotropic gastrointestinal hormone such as ghrelin (we have not excluded the gastric fundus and upper body), and the genetic variations of the GIP receptors which are shown in some Asians so that the recovery from the downregulated GIP receptors would be difficult [47].
There are several limitations in this study: (1) not identifying postglucose loading insulin response, (2) a considerable loss of follow-up—the percentage of patients being followed up was 74, 56, and 45 % in the first, second, and third years after the surgery. We have been trying to follow the protocol and to reduce follow-up loss as much as possible even though it is somewhat difficult because our patients come to our hospital from all parts of the country and even overseas countries for the surgery. As the data of this study has still been being collected, we should make an effort to perform a study with better quality. Future study also should be the controlled one with the age, BMI, and disease severity-matched groups and should identify the changes of insulin response and the incretin in response to the meal.
Conclusion
Longer follow-up and more subjects are needed, and the changes in fasting and postglucose loading plasma glucose along with the changes in insulin secretion after the meal should be identified. However, there have been no relapsed cases of the T2DM yet, and the LSAGB can control the T2DM safely and effectively.
References
Zimmer P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–87.
Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Korea Health Statistics 2010: Korea National Health and Nutrition Examination Study, the Ministry of Health and Welfare, 2010 (http://knhanes.cdc.go.kr) (KNHANES V-1).
Chan JM, Rimm EB, Colditz GA, et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17:961–9.
Colditz GA, Willett WC, Rotnitzky A, et al. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med. 1995;122:481–6.
Ambady R, Ronald Ching WM, Chamukuttau S. Diabetes in Asia. Lancet. 2010;375:408–18.
Juliana CN, Vasanti M, Weiping J, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–37.
Oh JY, Hong YS, Sung YA, et al. Prevalence and factor analysis of metabolic syndrome in an urban Korean population. Diabetes Care. 2004;27:2027–32.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Mingrone G, DeGaetano A, Greco AV, et al. Reversibility of insulin resistance in obese diabetic patients: role of plasma lipids. Diabetologia. 1997;40:599–605.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. Diabet Med. 2011;28:628–42.
Rutledge R. The mini-gastric bypass: experience with the first 1274 cases. Obes Surg. 2001;11:276–80.
Pories WJ, Albrecht RJ. Etiology of type 2 diabetes mellitus: role of the foregut. World J Surg. 2001;25:527–31.
Rubino F, Gagner M. Potential of surgery for curing type 2 diabetes mellitus. Ann Surg. 2002;236:554–9.
Scott EG, Frank LG, Stanley K. Effects of obesity surgery on non-insulin-dependent diabetes mellitus. Arch Surg. 2002;137:1109–17.
American Diabetes Association. Diabetes management in correctional institutions. Diabetes Care. 2010;33:S75–81.
Scopinaro N, Marinari G, Camerini GB, et al. Specific effects of biliopancreatic diversion on the major components of metabolic syndrome: a long-term follow-up study. Diabetes Care. 2005;28:2406–11.
Tejirian T, Jensen C, Dutson E. Bariatric surgery and type 2 diabetes mellitus: surgically induced remission. J Diabetes Sci Technol. 2008;2:685–91.
Bose M, Olivan B, Teixeira J, et al. Do incretins play a role in the remission of type 2 diabetes after gastric bypass surgery: what are the evidence? Obes Surg. 2009;19:217–29.
Padwal RS, Gabr RQ, Sharma AM, et al. Effect of gastric bypass surgery on the absorption and bioavailability of metformin. Diabetes Care. 2011;34:1295–300.
Patti ME, Houten SM, Bianco A, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity. 2009;17:1671–7.
Laferrere B, McGinty J, Heshka S, et al. Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care. 2007;30:1709–16.
Rubino F, R’bibo SL, del Genio F, et al. Metabolic surgery: the role of the gastrointestinal tract in diabetes mellitus. Nat Rev Endocrinol. 2010;6:102–9.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244:741–9.
Garcia-Caballero M, Valle M, Martinez-Moreno JM, et al. Resolution of diabetes mellitus and metabolic syndrome in normal weight 24-29 BMI patients with one anastomosis gastric bypass. Nutr Hosp. 2012;27:623–31.
Rubino F, Gagner M, Gentileschi P, et al. The early effect of the Roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004;240:236–42.
Roger HU, Anna ME. Entero-insular axis. Arch Intern Med. 1969;123:261–6.
Creutzfeldt W. The incretin concept today. Diabetologia. 1979;16:75–85.
Perley MJ, Kipnis DM. Plasma insulin responses to oral and intravenous glucose: studies in normal and diabetic subjects. J Clin Invest. 1967;46:1954–62.
Preitner F, Ibberson M, Franglin I, et al. Gluco-incretins control insulin secretion at multiple levels as revealed in mice lacking GLP-1 and GIP receptors. J Clin Invest. 2004;113:635–45.
Timothy JK, Joel FH. The glucagon-like peptides. Endocr Rev. 1999;20:876–913.
Fiona MG, Leanne W, Anna KS, et al. A novel glucose-sensing mechanism contributing to glucagon-like peptide-1 secretion from the GLUTag cell line. Diabetes. 2003;52:1147–54.
Juris JM, Michael AN, Wolfgang ES, et al. Gastric inhibitory polypeptide: the neglected incretin revisited. Regul Pept. 2002;107:1–13.
Creutzfeldt W. The entero-insular axis in type 2 diabetes—incretins as therapeutic agents. Exp Clin Endocrinol Diabetes. 2001;109(Suppl2):S288–303.
Santoro S, Castro LC, Velhote MC, et al. Sleeve gastrectomy with transit bipartition. A potent intervention for metabolic syndrome and obesity. Ann Surg. 2012;256:104–10.
Vilsboll T, Krarup T, Sonne J, et al. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab. 2003;88:2706–13.
Vilsboll T, Krarup T, Deacon CF, et al. Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes. 2001;50:609–13.
Fetner R, McGinty J, Russell C, et al. Incretins, diabetes, and bariatric surgery: a review. Surg Obes Relat Dis. 2005;1:589–98.
Wang W, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15(5):648–54.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8.
Piazza L, Ferrara F, Leanza S, et al. A laparoscopic mini-gastric bypass: short-term single-institute experience. Updat Surg. 2011;63(4):239–42.
Noun R, Skaff J, Riachi E, et al. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012;22(5):697–703.
Lee WJ, Wang W, Lee YC, et al. Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg. 2008;18(3):294–9.
Dang H, Arias E, Szomstein S, et al. Laparoscopic conversion of distal mini-gastric bypass to proximal Roux-en-Y gastric bypass for malnutrition: case report and review of the literature. SORD. 2009;5:383–6.
Johnson WH, Fernanadez AZ, Farrell TM, et al. Surgical revision of loop gastric bypass procedure: multicenter review of complications and conversions to Roux-en-Y gastric bypass. SORD. 2007;3:37–41.
Azagury DE, Abu Dayyeh BK, Greenwalt IT, et al. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43:950–4.
Kim YG, Hahn S, Oh TJ, et al. Differences in the glucose-lowering efficacy of dipeptidyl peptidase-4 inhibitors between Asians and non-Asians: a systematic review and meta-analysis. Diabetologia. 2013;56:696–708.
Acknowledgments
The point of this work was presented at the International Federation for the Surgery of Obesity and Metabolic disorders–Asia Pacific Chapter (IFSO-APC) meeting 2013 in Taiwan. This work was supported in part by the Soonchunhyang University Research Fund. Authors appreciate sincerely Su Yoon Go (Suzanne Burrows) for her help to revise this manuscript.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, M.J., Hur, K.Y. Short-Term Outcomes of Laparoscopic Single Anastomosis Gastric Bypass (LSAGB) for the Treatment of Type 2 Diabetes in Lower BMI (<30 kg/m2) Patients. OBES SURG 24, 1044–1051 (2014). https://doi.org/10.1007/s11695-014-1202-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1202-5