Abstract
Introduction
Laparoscopy has a clear patient benefit related to postoperative morbidity but may not be as commonly performed in low-and middle-income countries. The decision to convert to laparotomy can be complex and involve factors related to the surgeon, patient, and procedure. The objective of this work is to analyze the factors associated with conversion in laparoscopic surgery in a low-resource setting.
Methods
This is a single-center prospective study of patients who underwent laparoscopic surgery between May 1, 2018 and October 31, 2021. The parameters studied were age, sex, body mass index (BMI), intraoperative complication (e.g., accidental enterotomy, hemorrhage), equipment malfunction (e.g., technical failure of the equipment, break in CO2 supply line), operating time, and conversion rate.
Results
A total of 123 laparoscopic surgeries were performed. The average age of patients was 31.2 years (range 11–75). The procedures performed included appendix procedures (48%), followed by gynecological (18.7%), gallbladder (14.6%), digestive (10.56%), and abdominal procedures (4%). The average length of hospitalization was 3 days (range 1–16). Conversion to laparotomy was reported in 8.9% (n = 11) cases. Equipment malfunction was encountered in 9.8% (n = 12) cases. Surgical complications were noted in 11 cases (8.9%). Risk factors for conversion were shown to be BMI > 25 kg/m2 (OR 4.6; p = 0.034), intraoperative complications (OR 12.6; p = 0.028), and equipment malfunction (OR 9.4; p = 0.002).
Conclusion
A better understanding of the underlying factors associated with high conversion rates, such as overweight/obesity, intraoperative complications, and equipment failure, is the first step toward surgical planning to reduce postoperative morbidity in low-resource settings.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most abdominal surgical procedures can be performed through minimally invasive techniques with clear benefits to patients. This has been paired with a significant reduction in morbidity and mortality for many simple and complex abdominal surgical procedures. In contrast, laparoscopy has not been widely adopted in low-and middle-income countries (LMICs) [1, 2].
Many barriers exist for safe and efficient laparoscopic surgery in LMICs, resulting in open surgery remaining the preferred surgical approach [3, 4]. Hospital systems in LMICs such as Senegal, with a gross domestic product (GDP) per capita of $1636, face many financial and infrastructural challenges compared to those in the United States, a high-income country (HIC) with a GDP per capita of $70,248 [2]. For example, the regular maintenance of laparoscopic equipment, including repair and/or replacement of fiber optic cables, cameras, lenses, and other broken or lost parts, can incur exorbitant costs which are often prohibitive for hospitals in LMICs [5]. To properly function throughout the duration of a procedure, laparoscopic instruments also require a continuous power source which may not be readily available in many LMICs [6]. These obstacles can lead to instances where unplanned conversion, or the intraoperative transition from laparoscopy to open surgery, a commonly reported problem in hospitals throughout LMICs [3, 4].
In HICs like the United States, minimally invasive approaches have been widely implemented with favorable short- and long-term outcomes for patients [7,8,9]. In this setting, unplanned conversion to laparotomy is largely considered a quality metric that may indicate a lack of advanced training or surgical case volume [10,11,12]. Failure of laparoscopic instrumentation, which is commonly encountered in LMICs and can contribute to conversion, is generally underreported in the United States [1, 2, 5, 13].
Multiple retrospective series from HICs have shown unplanned conversion to laparotomy is associated with higher morbidity and mortality rates, longer lengths of hospitalization, and increased risk of additional procedures [14, 15]. The decision to convert to open surgery can be complex and involve factors related to the surgeon, patient, and procedure [4]. A study of these factors in LMICs would allow better preparation and preoperative planning to reduce the risk of complications for these underserved patient populations. As such, the objective of this work is to analyze the factors associated with unplanned conversion to laparotomy in a low-resource setting.
Materials and methods
The present study was conducted at the Department of Surgery at Saint-Louis Regional Hospital, a tertiary care center in West Africa, between May 1, 2018 and October 31, 2021. All patients undergoing laparoscopic surgery were prospectively studied.
The primary outcome was the frequency of unplanned conversion to laparotomy. The factors analyzed were age, sex, body mass index (BMI), length of hospitalization, existence of an intraoperative complication (e.g., accidental enterotomy, hemorrhage), equipment malfunction (e.g., failure of the equipment, break in CO2 lines), and operative time.
Data were prospectively retrieved from operating notes and patient records. The study was approved by our institution’s ethics committee.
Statistical analysis
All baseline characteristics were summarized with descriptive statistics. Categorical characteristics were reported as a frequency and percentage. Continuous characteristics were reported as mean ± standard deviation if normally distributed or median with interquartile range if not normally distributed. Skewness and kurtosis tests were used to assess normality of variables. Continuous variables were compared using Student’s t-test, and categorical variables were compared using Fischer exact tests or chi-squared tests where appropriate.
Bivariate analysis was performed to select variables associated with conversion from the study population. All variables that met threshold criteria (p < 0.20) were included for analysis in the final multivariable model. Independent factors associated with conversion were identified using logistic regression with calculation of Odds Ratios (OR) and confidence intervals (CI) according to the top-step method with Wald’s test. All hypothesis tests were two-sided with a significance threshold of p < 0.05. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA).
Results
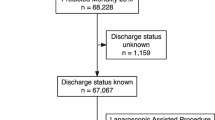
Over the study period, 123 laparoscopic surgeries were performed, representing 1.1% (23/11034) of total procedures at our institution in the same period. The average age of patients was 31.2 years (range 11–75) and there were 66 (53.6%) women. 22.7% (n = 28) had a BMI > 25 kg/m2. The average BMI was 22.5 kg/m2 ± 2.7. The procedure was urgent in 68 cases (55.2%). Diagnostic laparoscopy was performed in 19% of cases, therapeutic in 76.5% of patients and both diagnostic and therapeutic in 4.8%. The average operative time was 80.5 min (range 20–210 min). The average length of hospitalization was 3 days (range 1–16 days). The procedures performed included appendix procedures (48%), followed by gynecological (18.7%), gallbladder (14.6%), digestive (10.56%), and abdominal wall (4%). The baseline characteristics and distribution of surgical procedures according to procedure type are detailed in Tables 1 and 2. Equipment malfunction was encountered in 9.8% (n = 12) cases and surgical complications were noted in 11 cases (8.9%). The mean operative time was 86 min (range 20–210 min).
In 11 cases (8.9%), conversion to open surgery was needed. The reasons for conversion are shown in Table 3. Logistic regression found the following factors related to conversion: BMI > 25 kg/m2 (OR 4.6; p = 0.034), the existence of an intraoperative complication (OR 12.6; p = 0.028), and equipment malfunction (OR 9.4; p = 0.002). The results of the bivariate and multivariate analyses are detailed in Tables 4 and 5.
Postoperative complications were noted in 7.3% (n = 9), including: trocar site infection (n = 2), biliary leak (n = 3), missed enterotomy (n = 1), postoperative peritonitis (n = 1), and wound dehiscence (n = 2). Two deaths (1 bile leak, 1 pulmonary embolism) were recorded, leading to a mortality rate of 1.6% for this study.
Discussion
Our study represents a single-center experience describing factors that lead to laparoscopic to open conversion in a sub-Saharan LMIC. In this series of 123 laparoscopic procedures in a low-resource setting, we showed that BMI > 25, intraoperative complications, and equipment failure are associated with conversion. Existing literature on risk factors for unplanned conversion to laparotomy in LMICs is limited to case reports, short case series, or retrospective studies [2]. A better understanding of the factors associated with unplanned conversion is needed to improve procedural planning and gain insight into training and equipment needs in LMICs [16]. Notably, although Saint-Louis Regional Hospital is among the largest tertiary care centers in Senegal, the 123 laparoscopic procedures recorded in the study period comprised a small minority of total surgical procedures at this institution. This is consistent with practice patterns from other LMICs, such as the Philippines, whose largest tertiary government medical center reported 55% of cholecystectomies performed using an open approach in 2013 [17]. These findings from low-resource settings further suggest that slow adoption of laparoscopy likely prevails due to a combination of financial, infrastructural, and educational barriers [1,2,3,4].
Similar to this study, others have reported similar risk factors although the reported rates of conversion vary significantly. Pizzol et al. reported a conversion rate of 1.9% due to intraoperative complications in a retrospective series of 363 patients in Mozambique who underwent laparoscopic appendectomy and gynecological procedures [2]. In contrast to the present study, the relatively low conversion rate reported by Pizzol et al. is explained by the fact that diagnostic laparoscopy was the primary indication, although the reasons for conversion were similar [2]. In South Africa, Matsevych et al. studied 318 patients who received laparoscopy for abdominal trauma and detailed a conversion rate of 12.9% [18]. Uncontrolled intrabdominal bleeding was the primary reason for conversion. This study from the same continent demonstrated a higher conversion rate than the present study (8.9%), which may give insight into potential variability in laparoscopic practice patterns and outcomes across LMICs from similar regions. Similar to our findings, a recent retrospective study of 52 patients in Colombia who underwent laparoscopy for abdominal trauma showed a conversion rate of 7.7% also due to uncontrolled intraabdominal bleeding [19]. The relatively high rate of conversion due to intraoperative complications described in our study, in conjunction with the here reported studies, may be attributed to deficiencies in training or equipment availability in LMICs across multiple continents. Improved reporting on outcomes of laparoscopy, including operative time and potential intraoperative complications, is the first step for surgical teams to better anticipate complications and improve patient outcomes.
The present study also highlights instrument failure as a critical factor of conversion to laparotomy. This has been previously described in studies detailing resource-limited environments with frequent instrument reuse or lack of maintenance of laparoscopic instruments. For example, an 8-year prospective study from a single institution in Pakistan found 14.8% of conversions to have been converted to laparotomy due to instrument failure [20]. Similarly, a 2-year retrospective study in India found an alarming 71.4% of converted cases to have been caused by failure of laparoscopic instrumentation [21]. In our study, instrument failure was reported in 36.4% of converted cases. Despite the wide variability, all three studies illustrate technological shortcomings as contributing to unplanned conversion in low-resource settings. Despite the benefits associated with laparoscopic surgery, instrument failure represents an additional obstacle to the implementation of minimally invasive surgery in LMICs [22].
While most studies from LMICs report high conversion rates for low complexity laparoscopy, HICs largely report low conversion rates for high complexity laparoscopy. In Japan, a retrospective study of 208 patients who underwent laparoscopic liver resection showed a conversion rate of 3.8% and only determined uncontrollable intraoperative bleeding as a factor associated with conversion [23]. This experience from a HIC showed a lower conversion rate and fewer risk factors than our analysis. Notably, absent from the identified risk factors was instrument failure and obesity, which contrasts with our findings but is in line with others from HICs. A systematic review and meta-analysis of conversion during laparoscopic cholecystectomy by Rothman et al. identified 32 prospective and observational studies from HICs (including 460,995 total patients) and determined older age and male gender to be significant risk factors [24]. A total of 13 studies evaluated BMI as a preoperative risk factor, of which only six studies determined obesity to be associated with conversion to open surgery [24]. However, the quality of evidence among these 6 studies was highly heterogenous and subsequently demonstrated to be very low using the GRADE approach, leading researchers to recommend further inquiry to verify the role of BMI [24]. A recent retrospective series of 356 patients undergoing laparoscopic hysterectomy in the Netherlands showed a conversion rate of 2.8%, lower than that of the present study, due to poor intraoperative visibility [25]. With 79.8% of patients in this cohort reporting a BMI > 25 kg/m2, this nine-year experience suggested that conversion rates do not significantly change with increasing BMI, which is consistent with previous literature from HICs [25,26,27]. Overall, in contrast to our experience in Senegal, laparoscopy in HICs encounters a lower incidence of conversion for more complex surgical procedures, and weight or instrument failure are generally not demonstrated to be factors related to conversion.
Structured laparoscopic training is limited in low-resource settings such as Senegal. If present, formal training can lead to decreased conversion rates [10, 11]. Yi et al. detail a 9-year prospective experience and surgical training intervention in the Philippines, wherein 521 patients undergoing laparoscopic cholecystectomy experienced an overall conversion rate of 3.3% resulting from intraoperative complications [28]. The overall conversion rate decreased following completion of a 1-week surgical training course for laparoscopic naïve surgeons in this low-resource setting [28]. These findings help corroborate previous literature which suggests an association between the learning curve and rates of unplanned conversion to laparotomy [10, 11, 29].
Although technical skills are crucial to consider for the conversion rate, there is also a substantial body of literature emphasizing the significance of non-technical skills. Specifically, studies conducted in LMICs have suggested that relying solely on technical skills may not be sufficient for enhancing the quality of laparoscopic surgery. Therefore, it would be important to incorporate training on non-technical surgical skills, such as clinical decision-making and team communication, into the laparoscopy training program [30].
Professional surgical organizations are critical in ensuring safe and effective practice of laparoscopy by raising surgical standards across LMICs through modular training programs and hospital accreditation. The College of Surgeons of East, Central, and Southern Africa (COSECA) recently distributed a laparoscopic surgery needs assessment across its 44 accredited teaching hospitals in 16 different countries and found a lack of consumables, limited quantity of equipment, scarcity of skilled minimally invasive surgeons, and prohibitory costs associated with laparoscopic procedures as the main barriers of further developing laparoscopy [31, 32]. Despite the efforts of COSECA over the past two decades, these factors limit the practice of laparoscopy across COSECA hospitals and keep minimally invasive surgery inaccessible to millions of patients. To help fill this gap, the aid organizations Surgeons for Africa and Operation Hernia have implemented a structured laparoscopic surgical training program for postgraduate surgical trainees in east Africa, successfully educating 36 trainees in both mesh and non-mesh hernia repair over a 3-year period [33]. Such programs have tremendous potential to reduce unplanned conversion to laparotomy, postoperative morbidity, and mortality in low-resource settings by improving access to structured laparoscopic training. Further targeted development by national and international organizations can encourage improvements in surgical care throughout resource-limited settings.
In our institution, while some surgeons have received training in laparoscopy, we have observed that other members of the surgical team, such as OR nurses and other support staff, do not possess the necessary training in laparoscopic techniques. This lack of comprehensive training across the entire team can hinder the seamless integration of laparoscopic surgery into routine practice. Furthermore, it is worth noting that the administration’s perception of laparoscopy as an urgent and essential need may not always align with other surgical priorities such as obstetrics or open surgeries. This discrepancy in prioritization could result in limited investment in laparoscopic resources and infrastructure. The acquisition of materials and equipment supplies for laparoscopy can be costly and challenging to establish due to intricate procurement processes, even if reusable materials are utilized. These factors collectively contribute to the underutilization of laparoscopic surgery in our setting.
Limitations
The present study has a number of limitations. The single-center design and small number of patients limit the generalizability of the results, although these limitations are characteristic of the low-resource setting in Senegal. In addition, the analysis of conversion factors was not evaluated for the same types of surgical techniques. In addition, as conversion is related to a mix of patient, procedural, surgeon, and environmental factors, we did not analyze surgeon factors (e.g., age, years in practice, laparoscopic experience, subspecialty training). Despite these limitations, our study had the strength of prospective data collection over a 3-year study period.
Conclusion
Conversion is necessary when the proposed laparoscopic approach can no longer be pursued without significant risk. Understanding the factors associated with conversion, including BMI > 25 kg/m2, intraoperative complications, and equipment malfunction as per our analysis, may facilitate better procedural planning to reduce postoperative morbidity in low-resource settings such as LMICs.
References
Pallas G, Simon F, Sockeel P, Chapuis O, Jancovici R (2000) Inguinal hernia in Africa and laparoscopy: utopia or realism? Méd Trop Rev Corps Santé Colon 60:389–394
Pizzol D, Trott M, Grabovac I, Antunes M, Colangelo AC, Ippoliti S et al (2021) Laparoscopy in low-income countries: 10-year experience and systematic literature review. Int J Environ Res Public Health 18:5796. https://doi.org/10.3390/ijerph18115796
Schwartz M, Jeng CJ, Chuang LT (2017) Laparoscopic surgery for gynecologic cancer in low-and middle-income countries (LMICs): an area of need. Gynecol Oncol Rep 20:100–102. https://doi.org/10.1016/j.gore.2017.03.016
Jawale S, Jesudian G (2019) Low-cost laparoscopy for rural areas: the flexible video laparoscope. Trop Doct 49(1):68–70. https://doi.org/10.1177/0049475518808622
Higgins RM, Frelich MJ, Bosler ME, Gould JC (2017) Cost analysis of robotic versus laparoscopic general surgery procedures. Surg Endosc 31(1):185–192. https://doi.org/10.1007/s00464-016-4954-2
Farquharson DV, Jaramillo P, Samaras C (2018) Sustainability implications of electricity outages in sub-Saharan Africa. Nat Sustain 1:589–597
Crocker AB, Vega EA, Kutlu OC et al (2022) Is minimally invasive surgery for large gastric GIST actually safe? A comparative analysis of short- and long-term outcomes. Surg Endosc 36(9):6975–6983. https://doi.org/10.1007/s00464-022-09066-4
Ozair A, Collings A, Adams AM et al (2022) Minimally invasive versus open hepatectomy for the resection of colorectal liver metastases: a systematic review and meta-analysis. Surg Endosc 36(11):7915–7937. https://doi.org/10.1007/s00464-022-09612-0
PelvEx Collaborative (2018) Minimally invasive surgery techniques in pelvic exenteration: a systematic and meta-analysis review. Surg Endosc 32(12):4707–4715. https://doi.org/10.1007/s00464-018-6299-5
Massarotti H, Rodrigues F, O’Rourke C, Chadi SA, Wexner S (2017) Impact of surgeon laparoscopic training and case volume of laparoscopic surgery on conversion during elective laparoscopic colorectal surgery. Colorectal Dis 19(1):76–85. https://doi.org/10.1111/codi.13402
Schlachta CM, Mamazza J, Grégoire R, Burpee SE, Pace KT, Poulin EC (2003) Predicting conversion in laparoscopic colorectal surgery. Fellowship training may be an advantage. Surg Endosc 17(8):1288–1291. https://doi.org/10.1007/s00464-002-8920-9
Abelson JS, Afaneh C, Rich BS, Dakin G, Zarnegar R, Fahey TJ 3rd, Pomp A (2015) Advanced laparoscopic fellowship training decreases conversion rates during laparoscopic cholecystectomy for acute biliary diseases: a retrospective cohort study. Int J Surg 13:221–226. https://doi.org/10.1016/j.ijsu.2014.12.016
Cooper MA, Ibrahim A, Lyu H, Makary MA (2015) Underreporting of robotic surgery complications. J Healthc Qual 37(2):133–138. https://doi.org/10.1111/jhq.12036
Harboe KM, Bardram L (2011) The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc 25(5):1630–1641. https://doi.org/10.1007/s00464-010-1453-8
Bastawrous AL, Landmann RG, Liu Y, Liu E, Cleary RK (2020) Incidence, associated risk factors, and impact of conversion to laparotomy in elective minimally invasive sigmoidectomy for diverticular disease. Surg Endosc 34(2):598–609. https://doi.org/10.1007/s00464-019-06804-z
Warchałowski Ł, Łuszczki E, Bartosiewicz A et al (2020) The analysis of risk factors in the conversion from laparoscopic to open cholecystectomy. Int J Environ Res Public Health 17(20):7571. https://doi.org/10.3390/ijerph17207571
Santos-Belen KD, Perez A, Mendoza M (2016) Outpatient laparoscopic cholecystectomy: experience of a university group practice in a developing country. HPB. https://doi.org/10.5348/ijhpd-2016-58-OA-15
Matsevych O, Koto M, Balabyeki M, Aldous C (2018) Trauma laparoscopy: when to start and when to convert? Surg Endosc 32(3):1344–1352. https://doi.org/10.1007/s00464-017-5812-6
Gómez EJI, Vargas LFC, Lozada-Martinez ID et al (2022) Laparoscopy has better performance than laparotomy in the treatment of stable penetrating abdominal trauma: a retrospective cross-sectional study in a trauma referral hospital in Colombia. Health Sci Rep 5(3):e640. https://doi.org/10.1002/hsr2.640
Shamim M, Memon AS, Bhutto AA, Dahri MM (2009) Reasons of conversion of laparoscopic to open cholecystectomy in a tertiary care institution. J Pak Med Assoc 59(7):456–460
Jaffary SA, Shamim MS, Raza SJ, Dastagir A (2006) Instrument failure; a preventable cause of conversion in laparoscopic cholecystectomy. Pak J Surg 23(2):92–95
Cissé M, Konaté I, Ka O, Dieng M, Tendeng J, Diop B et al (2009) La laparoscopie en urgence à la clinique chirurgicale de l’hôpital Aristide Le Dantec de Dakar: les 100 premiers cas. e-mém l’Acad Natl Chir 8:78
Masuda T, Endo Y, Amano S et al (2022) Risk factors of unplanned intraoperative conversion to hand-assisted laparoscopic surgery or open surgery in laparoscopic liver resection. Langenbecks Arch Surg 407(5):1961–1969. https://doi.org/10.1007/s00423-022-02466-z
Philip Rothman J, Burcharth J, Pommergaard HC, Viereck S, Rosenberg J (2016) Preoperative risk factors for conversion of laparoscopic cholecystectomy to open surgery—a systematic review and meta-analysis of observational studies. Dig Surg 33(5):414–423. https://doi.org/10.1159/000445505
Haveman I, van Weelden WJ, Roovers EA, Kraayenbrink AA, Dijkhuizen FPHLJ (2022) Robot-assisted total laparoscopic hysterectomy in different classes of obesity: a cohort study. JSLS 26(1):e2021.00077. https://doi.org/10.4293/JSLS.2021.00077
Iavazzo C, Gkegkes ID (2016) Robotic assisted hysterectomy in obese patients: a systematic review. Arch Gynecol Obstet 293(6):1169–1183. https://doi.org/10.1007/s00404-016-4028-7
Cusimano MC, Simpson AN, Dossa F et al (2019) Laparoscopic and robotic hysterectomy in endometrial cancer patients with obesity: a systematic review and meta-analysis of conversions and complications. Am J Obstet Gynecol 221(5):410-428.e19. https://doi.org/10.1016/j.ajog.2019.05.004
Yi W, Perez J, Rosen C, Akalal F, Hassan I, Soriano I (2023) promoting a culture of safety in cholecystectomy (COSIC) over a decade at a Philippine public regional hospital after the SAGES international proctoring course in laparoscopic cholecystectomy course. Surg Endosc 37(1):613–616. https://doi.org/10.1007/s00464-022-09355-y
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91. https://doi.org/10.1097/01.sla.0000167857.14690.68
Scott J, Revera Morales D, McRitchie A, Riviello R, Smink D, Yule S (2016) Non-technical skills and health care provision in low-and middle-income countries: a systematic review. Med Educ 50(4):441–455
James J (2006) College of surgeons of East, Central and Southern Africa. Trop Doct 36(4):196. https://doi.org/10.1258/004947506778604661
Nyundo M, Umugwaneza N, Bekele A, Chikoya L, Gashegu J, Detry O (2003) Assessment of resource capacity and barriers to effective practice of laparoscopic surgery in training hospitals affiliated with the College of Surgeons of East, Central and Southern Africa (COSECSA). Surg Endosc. https://doi.org/10.1007/s00464-023-09985-w
Lorenz R, Oppong C, Frunder A et al (2021) Improving surgical education in East Africa with a standardized hernia training program. Hernia 25(1):183–192. https://doi.org/10.1007/s10029-020-02157-y
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Abdourahmane Ndong, Adja C. Diallo, Armaun D. Rouhi, Mohamed L. Diao, William Yi, Jacques N. Tendeng, Noel N. Williams, Mamadou Cisse, Kristoffel R. Dumon, Ibrahima Konaté have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ndong, A., Diallo, A.C., Rouhi, A.D. et al. Factors associated with conversion in laparoscopic surgery in a low-resource setting: a single-center prospective study. Surg Endosc 37, 8072–8079 (2023). https://doi.org/10.1007/s00464-023-10373-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10373-7