Abstract
Introduction
The purpose of this study is to determine the incidence of residual common bile duct (CBD) stones after preoperative ERCP for choledocholithiasis and to evaluate the utility of routine intraoperative cholangiography (IOC) during laparoscopic cholecystectomy (LC) in this patient population.
Methods
All patients who underwent preoperative ERCP and interval LC with IOC from 5/96 to 12/05 were reviewed under an Institutional Review Board (IRB)-approved protocol. Data collected included all radiologic imaging, laboratory values, clinical and pathologic diagnoses, and results of preoperative ERCP and LC with IOC. Standard statistical analyses were used with significance set at p < 0.05.
Results
A total of 227 patients (male:female 72:155, mean age 51.9 years) underwent preoperative ERCP for suspicion of choledocholithiasis. One hundred and eighteen patients were found to have CBD stones on preoperative ERCP, and of these, 22 had choledocholithiasis diagnosed on IOC during LC. However, two patients had residual stones on completion cholangiogram after ERCP and were considered to have retained stones. Therefore, 20 patients overall were diagnosed with either interval passage of stones into the CBD or a false-negative preoperative ERCP. In the 109 patients without CBD stones on preoperative ERCP, nine patients had CBD stones on IOC during LC, an 8.3% incidence of interval passage of stones or false-negative preoperative ERCP. In both groups, there was no correlation (p > 0.05) between an increased incidence of CBD stones on IOC and a longer time interval between ERCP and LC, performance of sphincterotomy, incidence of cystic duct stones, or pathologic diagnosis of cholelithiasis.
Conclusions
The overall incidence of retained or newly passed CBD stones on IOC during LC after a preoperative ERCP is 12.9%. Although the natural history of residual CBD stones after preoperative ERCP is not known, the routine use of IOC should be considered in patients with CBD stones on preoperative ERCP undergoing an interval LC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy (LC) is now the accepted standard treatment for benign diseases of the gallbladder. In the majority of uncomplicated cases of cholecystitis, cholelithiasis, and biliary colic, simple cholecystectomy is sufficient and definitive treatment, and no further intervention is usually necessary. However, when any of these situations is complicated by the ongoing presence of common bile duct (CBD) stones, there is less agreement as to the optimal treatment modality. The options available for the treatment of choledocholithiasis include various combinations of ERCP (with or without sphincterotomy), LC, intraoperative cholangiography (IOC), and surgical exploration with stone extraction.
Many practitioners advocate a single-stage approach of LC combined with IOC and laparoscopic common bile duct exploration (CBDE) to remove the CBD stones. This has generally been shown to be the most economical route due to shorter hospital stays and a low rate of complications. However, not all surgeons are facile in the laparoscopic approach to CBDE, and an open approach will usually negate the patient recovery and economic benefits of a short hospital stay.
Alternatively, laparoscopic cholecystectomy and intraoperative cholangiography may be combined with ERCP in a two-stage procedure. If the IOC indicates the presence of CBD stones at the time of surgery, then postoperative ERCP may be undertaken to remove the residual lithiasis. Unfortunately, postoperative ERCP has a failure rate of 4–10%. In order to prevent a return to the operating room for a common bile duct exploration, the ERCP with sphincterotomy may also be done preoperatively to facilitate removal of CBD stones. The patient then proceeds to a laparoscopic cholecystectomy. This sequence of events has the advantage of allowing the surgeon to visualize the bile ducts preoperatively from the ERCP images and subsequently at the time of operation via an IOC, and then take additional action (i.e., laparoscopic or open CBDE) should it be necessary.
This combination of preoperative ERCP followed by LC is now very commonly performed at those centers which have the benefit of a highly skilled team of endoscopists. However, such a sequence of procedures does not necessarily prevent the passage of existing stones from the gallbladder into the common bile duct. Additionally, the false negative rate of ERCP has not been well defined, and could contribute to the finding of CBD stones at IOC. As many surgeons do not routinely perform intraoperative cholangiography, it is foreseeable that undetected or newly passed stones could thus be left in situ at the time of LC. We therefore investigated our institution’s experience with intraoperative cholangiography at the time of laparoscopic cholecystectomy after preoperative ERCP in an attempt to define the incidence of residual common bile duct stones at the time of operation.
Materials and methods
Patient selection
Following Institutional Review Board approval, CPT codes were used to identify all those patients undergoing either ERCP or LC with an IOC at the Washington University Medical Center and Barnes-Jewish Hospital during the time period from May 1996 through December 2005. These patient populations were then cross-referenced by name and birth date in order to identify those patients who had undergone both procedures. Finally, ERCP and operative dates were manually compared to identify only that subset of patients who underwent ERCP prior to their operation. A retrospective clinical chart review was then conducted for all these patients who met the above inclusion criteria. Those patients undergoing ERCP for an indication other than gallstone disease were excluded, as were patients who had a laparoscopic cholecystectomy as a routine part of another procedure, such as laparoscopic gastric bypass. Also excluded were laparoscopic cases that were converted to open procedures.
Data collection
Data were collected on parameters such as patient demographics, timing and results of preoperative imaging, laboratory values, clinical and pathologic diagnoses, and intraoperative findings, including cholangiogram results. Furthermore, reports from all preoperative ERCP studies were obtained and data collected on parameters including cholangiogram findings, performance of a sphincterotomy, completeness of stone removal, and placement of a stent. In instances where more than one preoperative ERCP was performed, only the results and corresponding laboratory values from the procedure performed closest in time to that of the laparoscopic cholecystectomy were used.
Statistical analysis
Results were logged in a Microsoft Access database and then further analyzed using Microsoft Excel. Statistical analyses were performed using GraphPad InStat Software, and significance (p < 0.05) was determined using contingency tables with Fisher’s Exact Test and either a Wilcoxon matched-pairs test or Mann–Whitney test, where appropriate. Nonpercentile values are expressed as mean ± standard deviation (SD). This study was approved by the Washington University School of Medicine Human Studies Committee (protocol #06-0467).
Results
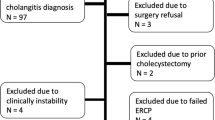
During the time course of this study, over 5,500 laparoscopic cholecystectomies were performed at our institution. ERCP was performed in 774 patients, of which 422 had an intraoperative cholangiogram performed at the time of LC. When those patients in this group undergoing only postoperative ERCP were identified and removed, a total of 254 patients were found to have undergone preoperative ERCP followed by LC with IOC. Of these patients, 227 (72 male, 155 female) met the inclusion criteria and were analyzed. This patient selection scheme is summarized in Fig. 1.
The Mean patient age was 51.9 ± 20.2 years with a range of 6 to 95 years. The majority of patients were overweight to obese, with a mean BMI of 29.9 ± 7.9. Pre-ERCP imaging included abdominal ultrasound in 191 patients (84.1%), which demonstrated cholelithiasis in 175 (91.6%). Furthermore, of those patients imaged with pre-ERCP ultrasound, 87 (45.5%) were found to have common bile duct stones, yet only four (2.1%) demonstrated stones within the intrahepatic bile ducts. Biliary ductal dilatation was seen by ultrasound in 50.7% of the total patient population, with 41 patients having a common bile duct diameter in the 6–8 mm range, and 74 patients with CBD dilatation to greater than 8 mm. Several patients also exhibited radiologic evidence of acute cholecystitis, with 40 (20.9%) and 13 (6.8%) presenting with gallbladder wall thickening and pericholecystic fluid, respectively, on ultrasound examination.
Magnetic resonance cholangiopancreatography (MRCP) was performed prior to ERCP in 4 patients (1.8%), and 12 (5.3%) underwent biliary scintigraphy (HIDA scan). Neither of these imaging modalities suggested the diagnosis of choledocholithiasis in any of our patients. Nine patients had a percutaneous cholecystostomy tube placed for severe acute cholecystitis, and 20 underwent one or more percutaneous diagnostic cholangiograms, either via the indwelling tube or a temporary catheter. Percutaneous cholangiography demonstrated the presence of common bile duct stones in a total of 16 (7.0%) patients and an unspecified biliary stricture in 1 (0.4%).
All patients had undergone at least one preoperative ERCP, with 15 patients having had two, and 8 patients having undergone three or more (range, 1–5). Given the retrospective nature of this study, no specific indications were defined for those patients undergoing preoperative ERCP. In general, patients at our institution will undergo an initial ERCP for any of the following findings: (1) abdominal pain of suspected biliary or pancreatic origin, (2) evidence of common bile duct stones or biliary ductal dilatation on preoperative imaging studies, (3) laboratory elevations in liver transaminases and/or bilirubin, or (4) a diagnosis of ascending cholangitis or acute or recurrent pancreatitis. At the time of preoperative ERCP, 118 patients (52.0%) were found to have CBD stones while 109 (48%) had a negative ERCP. Complete stone removal was accomplished in 112 (95%) of these patients, with residual stones present in the other 6. A sphincterotomy was performed in 180 of 227 patients (79%), and biliary stents were placed in 21 patients (9.3%). A patent cystic duct was documented in 173 patients, while 23 of the 54 patients with an occluded cystic duct were noted to have cystic duct stones. Six patients were also noted to have hepatic duct stones. Immediate postprocedural complications were noted in only 4 of the 167 patients, for whom there was complete ERCP data. These included two small sphincterotomy bleeds that were managed conservatively and two patients who underwent transient oxygen desaturations that responded to supplemental oxygen therapy. No information on delayed complications (i.e., unrecognized iatrogenic injury, post-ERCP pancreatitis) was available at the time of this study.
At the time of LC, an IOC was attempted in all patients, with only six procedures (2.6%) being unsuccessful due to an inability to cannulate the cystic duct. Early in the series, five patients underwent intraoperative ultrasound (IOUS), rather than IOC, in order to assess the common bile duct. No bile duct injuries were noted and no complications occurred as a consequence of performing the IOC or IOUS procedure. In the 118 patients with CBD stones seen on ERCP, 22 (20.8%) had CBD stones diagnosed by IOC. However, two of these patients were those with residual stones on completion cholangiogram after preoperative ERCP and were considered to have retained stones. Additionally, nine patients had an initial ERCP cholangiogram that was negative, had no stone extraction, and yet were found to have CBD stones on IOC. Therefore, 29 (12.8%) patients overall were diagnosed with either interval passage of stones or a false-negative preoperative ERCP. Of these 29 patients with documented CBD stones on IOC, four had their stones successfully cleared by flushing with saline (either with or without glucagon administration), while two required a laparoscopic common bile duct exploration. Ten patients were referred for an immediate (<24 hour) postoperative ERCP, and four underwent ERCP at a later time point. For nine of these patients, no specific documentation of stone management was noted. CBD stones were generally described as “small filling defects”, and only one of the 29 operative reports indicated a specific stone size, in which a single 1.2 cm stone was successfully extracted via laparoscopic CBDE.
In the 118 patients with CBD stones seen on preoperative ERCP, there was no correlation (p > 0.05) between the incidence of CBD stones found at the time of IOC and the performance of sphincterotomy, placement of a biliary stent, presence of cystic duct stones or pathologic diagnosis of cholelithiasis. In the 109 patients without CBD stones on preoperative ERCP, 9 patients (8.3%) had CBD stones on IOC during LC. Similar to the other cohort, there was no correlation (p > 0.05) between the incidence of CBD stones seen on IOC and the performance of a sphincterotomy, biliary stent placement, preoperative presence of cystic duct stones, pathologic diagnosis of cholelithiasis or the performance of a completion cholangiogram upon finishing the preoperative ERCP. There also appeared to be no correlation between an increased incidence of retained or newly passed stones and a longer time interval between the ERCP and LC procedures, as the average time span was 85 days in the population without CBD stones on IOC, but only 10.6 days in patients with common bile duct stones seen on intraoperative cholangiography.
Contingency table analysis did, however, show a significant correlation between common bile duct stones seen on preoperative ERCP and the presence of choledocholithiasis on IOC (p = 0.0322). The sensitivity and specificity of ERCP-proven CBD stones predicting choledocholithiasis at the time of LC were 70.9% and 51.0%, respectively, with a positive predictive value of 18.6% and a negative predictive value of 91.7%. With the exception of the serum albumin level, all liver function test (LFT) values such as ALT, AST, alkaline phosphatase, and total bilirubin showed significant improvement/resolution during the time interval between ERCP and LC, as shown in Table 1. At the time of operation, however, only the serum AST showed a significant difference between patients with versus those without retained CBD stones seen on IOC. There were no significant differences in the pre-ERCP laboratory values between those patients that developed retained CBD stones compared to those who did not. These results are shown in Table 2.
Discussion
As modern surgical techniques become increasingly less invasive, they are more frequently combined with endoscopic or endoluminal approaches to achieve their desired outcome. One such combination of laparoscopic and endoscopic approaches that is commonly employed is the use of preoperative ERCP followed by LC as a two-stage procedure for the treatment of cholecystitis and/or biliary colic and a presumptive or confirmed diagnosis of choledocholithiasis. This option is potentially attractive in that it allows for immediate decompression of the biliary tract and clearance of the CBD stones with elective LC at a later time. This is especially useful in the situation in which the patient presents with sepsis or has multiple medical comorbidities, and would thus be a poor candidate for immediate surgery. After being initially decompressed endoscopically, the patient can be fully resuscitated and/or medically optimized before being taken to the operating room in a controlled fashion. ERCP also provides the surgeon with a preoperative cholangiogram that may identify aberrant anatomy and assist in the performance of a safe surgical procedure. Additionally, sphincterotomy can facilitate the passage of stones in the future, should new stones migrate out of the gallbladder during the interval between ERCP and surgery. However, the results of this study show that the performance of a preoperative ERCP does not de facto guarantee that stones will not become lodged in the common bile duct prior to the time of surgery. It is our opinion that most surgeons performing LC will generally assume that the CBD is stone-free due to the preoperative ERCP. This assumption may be reinforced by a normalization in patient lab values such as serum transaminases and total bilirubin levels. For this reason, it is likely that many, if not most, surgeons will forego the performance of an intraoperative cholangiogram in order to confirm CBD clearance.
In large published series in the literature, the incidence of common bile duct (CBD) stones at the time of laparoscopic cholecystectomy (LC), as visualized by intraoperative cholangiography (IOC), is reported to be between 3% and 12% [1–3]. However, it might be expected that this incidence would be lower in those patients undergoing a preoperative ERCP and/or sphincterotomy with stone extraction. The purpose of this study was to determine the incidence of retained CBD stones after ERCP and evaluate the utility of performing routine IOC in this patient population.
At our institution, based on both personal preference and/or the desire to teach the procedure to surgical residents, many of our surgeons perform intraoperative cholangiography on a routine basis, regardless of preoperative interventions or laboratory values. We thus have an extensive experience with cholangiography and were able to identify 227 patients in which preoperative ERCP was performed and who received IOC at the time of LC. Our results demonstrated that, of 118 patients with choledocholithiasis on ERCP, 22 (21%) also had CBD stones on IOC. This incidence of residual choledocholithiasis as detected by intraoperative imaging is consistent with the results of a similarly sized study published in 1998 [4]. Endoscopic stone extraction was initially attempted in all of these 22 stone-positive patients, with complete removal in 91% (20/22) as confirmed by completion cholangiogram. Given that two patients had incomplete stone extraction, they should be considered to have retained stones and would be expected to have persistent choledocholithiasis at the time of surgery. In contrast, 20 patients with a negative completion cholangiogram after ERCP were found to have previously unappreciated stones at the time of LC, for an overall incidence of approximately 17%. This incidence of recurrent stones is comparable to the rates commonly reported in the literature, which have ranged from 4–24% [5, 6]. It can be safely assumed that these patients either had a false-negative completion cholangiogram or had stones migrate from the gallbladder during the interval between ERCP and LC. We also identified 9 of 109 patients (8.3%) with common bile duct stones at the time of LC who initially had a negative ERCP, and thus no initial stone extraction procedure. This finding also suggests an approximately 8% incidence of either a false-negative ERCP cholangiogram, interval passage of stones from the gallbladder or cystic duct, or a combination thereof.
Taken together, the 9 patients with an initially negative ERCP cholangiogram along with the 22 patients with a negative completion cholangiogram yield an overall IOC positivity rate of 13.6% (31/227). Of these 31 patients with residual choledocholithiasis, 11 (35%) had a preoperative diagnosis of cholelithiasis, while 20 (65%) had no prior diagnosis of gallbladder stones. Similarly, 4 of the 31 patients (13%) with CBD stones on IOC had cystic duct stones found at the time of preoperative ERCP, whereas 27 (87%) had no evidence of cystic duct stones preoperatively. While both of these preoperative conditions might seems to be predictors of finding CBD stones at the time of LC, contingency table analysis show that neither of these conditions is significantly correlated with the presence of choledocholithiasis on IOC. In contrast, the presence or absence of common bile duct stones at the time of preoperative ERCP does correlate with whether or not stones are found at the time of laparoscopic cholecystectomy (p = 0.0322). In this study, the sensitivity and specificity of the finding of CBD stones on ERCP are 71% and 51%, respectively, with a positive predictive value of 18.6% and a negative predictive value of 91.7%.
In addition to preoperative findings of cholelithiasis and cystic duct stones being likely predictors of future choledocholithiasis at the time of laparoscopic cholecystectomy, it would also seem logical that a longer time period between the two procedures would correlate with a greater percentage of patients having choledocholithiasis at the time of LC. This, however, was not demonstrated in the current study. We analyzed time points of 1 week, 1 month, 2 months, and 3 months between ERCP and LC, none of which showed any significant difference in the incidence of stones found at the time of LC. Similarly, in the 31 patients found to have choledocholithiasis on IOC, no statistically significant difference in the incidence of CBD stones in those 25 patients (81%) undergoing sphincterotomy versus the 6 patients in which no sphincterotomy was preformed (19%, p > 0.05). In fact, this finding suggests that even the performance of a sphincterotomy is unlikely to prevent the reaccumulation of CBD stones by the time of surgery.
Therefore, it would appear from this study that none of the parameters we evaluated, other than the presence of CBD stones on preoperative ERCP, and possibly the preoperative serum ALT, are reliable predictors of whether or not a patient will develop new CBD stones during the interval between ERCP and LC. Therefore, the only way to accurately determine if residual choledocholithiasis exists is to perform intraoperative cholangiography or ultrasound at the time of LC. In addition to delineating the ductal anatomy and possibly helping the surgeon avoid or recognize a bile duct injury, the information gained from the IOC will allow the surgeon to perform an appropriate intervention should choledocholithiasis be discovered.
Such action may include expectant management, thus allowing ductal stones to pass on their own, or completion of the laparoscopic cholecystectomy followed by postoperative ERCP. The former option may not be advisable for stones greater than 2 mm in size due to the potential for the patient to develop recurrent symptoms of CBD obstruction. The second option is currently practised at those centers with highly skilled interventional endoscopists, although the failure rate of postoperative ERCP is reported to be 4–18% [7–9]. Unfortunately, this three-stage strategy subjects the patient to an additional postoperative procedure and a correspondingly increased hospital stay.
Alternatively, for surgeons with appropriate expertise, the residual common bile duct stones may be managed intraoperatively via laparoscopic transcystic CBDE, or via a choledochotomy. Either minimally invasive modality requires proper instrumentation and OR staffing, as well as a significant amount of skill and procedural knowledge on the part of the performing surgeon. Additionally, he or she must be willing to devote the additional time required for laparoscopic CBDE to the operative procedure. A lack of any of these factors will likely compel the surgeon to seek a postoperative ERCP as described earlier. However, the success rate of the single-stage procedure is somewhat higher at 80–98%, and published series have shown it to be superior to the two-stage procedure in terms of a shortened hospital stay [7, 10]. In fact, in a recent study by Rhodes et al., patients with choledocholithiasis at the time of LC were randomized to undergo either postoperative ERCP or laparoscopic CBDE, with an observed ductal clearance rate of 93% for the former procedure and 100% for the latter [11].
One question that remains incompletely answered is whether or not residual choledocholithiasis has any measurable impact on patient morbidity and mortality. Several recent studies have attempted to address this issue, as well as that of whether or not routine IOC should be employed, with differing results. In a 2002 study by Thornton et al., 377 patients underwent laparoscopic cholecystectomy without intraoperative cholangiogram; of these 103 had previously undergone ERCP, as they were deemed to be at high risk for CBD stones [12]. Following LC, 18 patients (4.8%) presented with symptoms suggestive of recurrent stone disease, but only 4 were confirmed to have or found to be highly suspicious for having retained stones. Only a single repeat ERCP was required for symptom resolution, leading the authors to conclude that IOC is not beneficial, as the incidence of retained stones is low and any sequelae are easily managed. More recently, Collins et al. reported a series of 997 laparoscopic cholecystectomies with IOC performed in 96% of the cases [13]. Forty-six patients (4.6%) had filling defects and were left with indwelling cholangiocatheters for follow-up cholangiograms. Approximately 25% of these patients had a negative study at 48 hours postoperatively, and an additional 25% were negative by 6 weeks. Although the remaining 22 patients with positive cholangiograms at 6 weeks ultimately underwent repeat ERCP, the authors conclude that 50% of those patients with a positive cholangiogram at the time of surgery can be expectantly managed and spared an additional ERCP or other intervention.
In contrast, Boerma et al. performed a prospective, randomized trial in which 120 patients underwent ERCP with sphincterotomy and were then randomized to either watchful waiting or LC [14]. In the watchful waiting group, 47% of patients experienced recurrent biliary symptoms, compared to only 2% in the LC group. Moreover, the watchful waiting patients with recurrent symptoms who did eventually undergo LC experienced a longer hospital stay (9 versus 7 days), higher morbidity (32% versus 14%), and greater than twofold increase in the rate of conversion to an open procedure (55% versus 23%). A recent prospective trial with similar randomization from Hong Kong involved 187 patients and reported, at a median follow-up of 5 years, that 24% of patients in the watchful waiting group re-presented with biliary obstructive symptoms compared to 7% of those who received LC. Both studies conclude that ERCP with sphincterotomy alone is not sufficient to prevent recurrent symptoms if the gallbladder is left in situ. However, neither study mentioned the use of intraoperative cholangiography, even those patients who underwent LC had recurrent symptoms in 2% and 7% of the cases, indicating that a single ERCP with sphincterotomy may not have been adequate to maintain clearance of the CBD at the time of surgery.
Because our study did not include a patient cohort that did not undergo intraoperative cholangiography we were not able to precisely demonstrate the additional time required for this procedure. However, at our institution, where we frequently use IOC, the procedure typically adds approximately 10–15 min of additional time to a standard laparoscopic cholecystectomy. This additional time is also in agreement with the current literature, in which several recent large studies report the additional time for and IOC as being between 8 and 13 min [3, 15, 16]. Additionally, Ludwig et al. add that, in their 2002 series out of Germany, the cost of an IOC was only 30–50 USD, compared to 100–150 USD for an additional ERCP [3]. Regardless of the surgeon’s preference, using IOC to identify residual choledocholithiasis allows the surgeon to perform laparoscopic common bile duct exploration during the laparoscopic cholecystectomy, convert to an open CBDE, or complete the LC and have an interventional endoscopist perform postoperative ERCP, which may be done as early as the day of surgery. In a Western population, where primary bile duct stones are rare, such perioperative common bile duct clearance should prevent further stone-related complications and obviate the need for readmission and/or additional procedures.
Conclusions
In this study, the incidence of residual common bile duct stones at the time of laparoscopic cholecystectomy is 16.9% in a cohort of patients with documented choledocholithiasis at the time of preoperative ERCP. The corresponding rate is 8.3% in a similar cohort of patients without choledocholithiasis on ERCP, for an overall rate of 12.8% for the entire group of patients. Furthermore, preoperative laboratory values, the presence of gallbladder or cystic duct stones, performance of sphincterotomy, and the time interval between ERCP and LC are poor predictors of which patients will harbor residual CBD stones. In a population similar to ours, many patients with choledocholithiasis diagnosed on intraoperative cholangiography at the time of laparoscopic cholecystectomy may benefit from an intraoperative or perioperative procedure to address the residual CBD stones. Thus, we recommend the liberal use of IOC at the time of interval LC when CBD stones have been documented on preoperative ERCP.
References
Koo KP, Traverso LW (1996) Do preoperative indicators predict the presence of common bile duct stones during laparoscopic cholecystectomy? Am J Surg 171:495–499
Traverso LW, Hauptmann EM, Lynge DC (1994) Routine intraoperative cholangiography and its contribution to the selective cholangiographer. Am J Surg 167:464–468
Ludwig K, Bernhardt J, Lorenz D (2002) Value and consequences of routine intraoperative cholangiography during cholecystectomy. Surg Laparosc Endosc Percutan Tech 12:154–159
Sbeih F, Aljohani M, Altraif I, Khan H (1998) Role of endoscopic retrograde cholangiopancreatography before and after laparoscopic cholecystectomy. Ann Saudi Med 18:117–119
Sultan S, Baillie J (2004) Recurrent bile duct stones after endoscopic sphincterotomy. Gut 53:1725–1727
Vezakis A, Davides D, Ammori BJ, Martin IG, Larvin M, McMahon MJ (2000) Intraoperative cholangiography during laparoscopic cholecystectomy. Surg Endosc 14:1118–1122
Hungness ES, Soper NJ (2006) Management of common bile duct stones. J Gastrointest Surg 10:612–619
Tranter SE, Thompson MH (2002) Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg 89:1495–1504
Williams GL, Vellacott KD (2002) Selective operative cholangiography and perioperative endoscopic retrograde cholangiopancreatography (ERCP) during laparoscopic cholecystectomy: a viable option for choledocholithiasis. Surg Endosc 16:465–467
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB (1999) E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 13:952–957
Rhodes M, Sussman L, Cohen L, Lewis MP (1998) Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet 351:159–161
Thornton DJ, Robertson A, Alexander DJ (2002) Laparoscopic cholecystectomy without routine operative cholangiography does not result in significant problems related to retained stones. Surg Endosc 16:592–595
Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC (2004) A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg 239:28–33
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, Boerma EJ, Obertop H, Huibregtse K, Gouma DJ (2002) Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 360:761–765
Bresadola V, Intini S, Terrosu G, Baccarani U, Marcellino MG, Sistu M, Scanavacca F, Bresadola F (2001) Intraoperative cholangiography in laparoscopic cholecystectomy during residency in general surgery. Surg Endosc 15:812–815
Amott D, Webb A, Tulloh B (2005) Prospective comparison of routine and selective operative cholangiography. ANZ J Surg 75:378–382
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pierce, R.A., Jonnalagadda, S., Spitler, J.A. et al. Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg Endosc 22, 2365–2372 (2008). https://doi.org/10.1007/s00464-008-9785-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9785-3