Abstract
Choledocholithiasis is a frequently encountered problem on intraoperative cholangiography at the time of laparoscopic cholecystectomy. While numerous strategies have been described for dealing with this intraoperative scenario, most surgeons employ laparoscopic common bile duct exploration (LCBDE), open common bile duct exploration, or postoperative endoscopic retrograde cholangiopancreatography (ERCP) in this situation. It is important to understand the relative outcomes of each of these strategies in terms of stone clearance rates, morbidity, the need for secondary procedures, and other outcomes such as hospital length of stay. Although the data are limited, the initial procedure of choice may be LCBDE through a transcystic approach, followed by either transcholedochal exploration (laparoscopic or open) or postoperative ERCP depending on anatomic factors and available expertise.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Choledocholithiasis
- Bile duct exploration
- Open
- Laparoscopic
- Sphincterotomy
- Endoscopic retrograde cholangiopancreatography
- Cholangiography
Introduction
Choledocholithiasis is a common problem, occurring in approximately 10–15 % of all patients undergoing cholecystectomy [1]. In the “open ” surgical era, the standard of care for choledocholithiasis was open cholecystectomy with concurrent common bile duct exploration . The introduction of laparoscopic cholecystectomy , however, made conversion to open common bile duct exploration in the setting of choledocholithiasis discovered intraoperatively a less attractive option, leading to the increased utilization of endoscopic retrograde cholangiopancreatography (ERCP ) for the diagnosis and management of choledocholithiasis. The eventual development of laparoscopic common bile duct exploration, while expanding the available therapeutic options for choledocholithiasis, has made the algorithm for the management of choledocholithiasis more complex. This evidence-based chapter seeks to identify and analyze the best available evidence for the management of a frequently encountered scenario: choledocholithiasis discovered intra-operatively during laparoscopic cholecystectomy. While numerous options have been described for dealing with this scenario, the chapter will focus on the three main options of laparoscopic common bile duct exploration (LCBDE), open common bile duct exploration (OCBDE), and postoperative ERCP.
Search Strategy
A systematic search of the English language literature was conducted using PubMed and the PICO methodology (Table 23.1). The “filter” function was used to select articles classified as “Randomized Controlled Trial” in order to obtain the highest quality comparative studies. The search terms used included “laparoscopic bile duct exploration ,” “open bile duct exploration,” “bile duct exploration”, “ERCP ,” “endoscopic sphincterotomy ,” “choledocholithiasis ,” and “common bile duct stones.” Studies that directly compared at least two of the three interventions (OCBDE, LCBDE, or ERCP) were included. Studies that compared two different variations of a single intervention (e.g. LCBDE with choledochoscopy versus LCBDE with fluoroscopy alone) were excluded, as were studies involving intraoperative ERCP. Treatment outcomes of interest included stone clearance rate, morbidity including bile duct injury , and the need for secondary procedures. Event rates were reported as percentages or total numbers of patients, with means reported as mean ± standard deviation unless otherwise noted.
Results
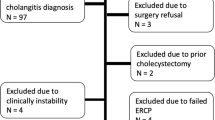
A literature search was conducted and included articles published prior to September 17th, 2014. A total of 590 articles were screened with a total of 16 randomized controlled trials (RCT) meeting the inclusion and exclusion criteria. Seven of these articles compared OCBDE to preoperative ERCP plus cholecystectomy [2–8], six articles compared LCBDE to preoperative ERCP plus cholecystectomy [9–14], one article compared OCBDE to LCBDE [15], and two articles compared LCBDE to laparoscopic cholecystectomy with postoperative ERCP [16, 17].
The most relevant RCTs to help determine the best evidence-based strategy for the management of choledocholithiasis found on intraoperative cholangiography are those that compare LCBDE to postoperative ERCP (Rhodes 1998; Nathanson 2005) [16, 17], and LCBDE to OCBDE (Grubnik 2012) [15] (Table 23.2). Unfortunately, there are no RCTs that have compared open cholecystectomy with OCBDE versus open cholecystectomy with postoperative ERCP.
LCBDE Versus Postoperative ERCP
‘The study by Rhodes et al. recruited 480 patients undergoing laparoscopic cholecystectomy [17]. Eighty patients (17 %) in the study group had cholangiograms demonstrating common bile duct (CBD) stones. The patients with choledocholithiasis were randomized intraoperatively to LCBDE or postoperative ERCP . For patients in the LCBDE group, a transcystic approach was attempted for patients with small CBD stones (<9 mm). A transcholedochal approach was instead used for patients with larger stones, proximal stones, a failed transcystic approach, and as long as the CBD was at least 6 mm to decrease the risk of postoperative stricture . Inability to clear the ducts with LCBDE led to postoperative ERCP. Patients randomized to postoperative ERCP underwent cholecystectomy followed by ERCP within 48 h of surgery . Inability to clear the duct with postoperative ERCP was followed by repeat ERCP attempt (s) 1 week later. The initial stone clearance rate for both groups was equivalent (75 %). Morbidity was similar between groups (18 % for LCBDE versus 20 % for postoperative ERCP). Morbidity for LCBDE included conversion to open surgery (2.5 %), urinary retention (2.5 %), readmission for pain of unclear etiology (5 %), and bile leak related to transcholedochal exploration (7.5 %). Morbidity for the postoperative ERCP group included hemorrhage requiring laparoscopic re-operation (2.5 %), bile leak while waiting for ERCP (2.5 %), bleeding from sphincterotomy site (7.5 %), and inability to clear CBD after repeated ERCP attempts (7.5 %). The need for postoperative ERCP was 25 % in the LCBDE group. Ten patients in the LCBDE group required additional procedures (nine ERCPs and one conversion to OCBDE). Ten patients randomized to postoperative ERCP required a second ERCP, with five of these patients requiring a third ERCP for a total of 15 additional ERCPs. Final stone clearance rate was 100 % for LCBDE patients and 93 % for postoperative ERCP patients. Median hospital length of stay was significantly shorter for the LCBDE group (1 day, range 1–26 days) versus the postoperative ERCP group (3.5 days, range 1–11 days, p = 0.0001). The conclusions of this study were that LCBDE can be performed with equivalent stone clearance rates, similar morbidity , but a shorter hospital stay compared to postoperative ERCP.
Martin et al. reported on the technical evolution of a laparoscopic approach to patients with choledocholithiasis , achieving successful stone clearance in 90 % of patients using a combination of transcystic or transcholedochal exploration [18]. Given the higher morbidity with transcholedochal versus transcystic exploration in their series, however, the same investigators (Nathanson et al.) then sought to study whether patients who had failed transcystic stone clearance were better off with immediate transcholedochal LCBDE or postoperative ERCP [16]. They enrolled 372 patients undergoing an attempt at transcystic LCBDE. The 23 % of patients (n = 86) who failed transcystic LCBDE were randomized intraoperatively to transcholedochal LCBDE versus postoperative ERCP. Initial stone clearance rates were similar (98 % for transcholedochal and 96 % for postoperative ERCP). One patient in the LCBDE group required postoperative ERCP for a retained stone, while two postoperative ERCP patients required LCBDE for retained stones. Overall morbidity was similar between groups and included bile leak (six patients for transcholedochal LCBDE, none for ERCP), clinical pancreatitis (one patient in each group), severe sepsis (one patient in each group), retained stone (two patients for postoperative ERCP and one patient for LCBDE), gastrointestinal bleeding (two patients for postoperative ERCP), early re-operation (two for transcholedochal LCBDE, and two for postoperative ERCP), and late re-operation for a biliary stricture (one patient in each group) possibly representing a bile duct injury from the procedure (s). Hospital length of stay was similar (mean of 6.4 versus 7.7 days for transcholedochal LCBDE and postoperative ERCP, respectively). The conclusions of this study were that either transcholedochal LCBDE or postoperative ERCP could be performed with similar results for patients who had failed attempted transcystic LCBDE. The authors recommended that transcholedochal LCBDE be avoided in patients with a CBD less than 7 mm or in the setting of severe inflammation. They advocated the use of transcholedochal LCBDE in patients with a history of a Billroth II reconstruction, in those who failed ERCP, or in those who otherwise would experience long delays in being transferred to other centers for ERCP.
The results of these studies suggest that for patients found to have choledocholithiasis on intraoperative cholangiography , LCBDE can achieve similar stone clearance rates and morbidity compared to postoperative ERCP , and yet result in a shorter length of stay and a decreased number of procedures.
LCBDE Versus OCBCE
How does LCBDE compare to OCBDE, the gold standard for choledocholithiasis during the “open era,” in patients found to have choledocholithiasis on intraoperative cholangiography ? A single, randomized controlled trial from Eastern Europe addresses this question (Grubnik 2012) [15]. This trial enrolled 256 patients with suspected choledocholithiasis, confirmed on intraoperative cholangiography, and randomized them to LCBDE (n = 138) or OCBDE (n = 118). Bile duct exploration was performed using an initial transcystic approach followed by a transcholedochal approach if unsuccessful. Stone clearance rates for LCBDE were 71 % with an initial transcystic approach and 94 % with a subsequent transcholedochal approach. Stone clearance rate with a transcystic approach was 10 % for OCBDE and 96.6 % with a subsequent transcholedochal or transduodenal (one patient) approach. Four patients (6.5 %) in the LCBCE group required postoperative ERCPs for stone clearance, resulting in a 100 % final stone clearance rate. In the OCBDE group four patients (3.3 %) required ERCP with one patient requiring an additional open re-exploration., for a final stone clearance rate of 100 %. Overall morbidity was similar between groups, with the exception of wound infections, which were more frequent in OCBDE (6 % versus 0.7 % for LCBDE). Bile leak was similar in both groups (1.4 % in LCBDE patients versus 0.8 % in OCBDE patients). Blood loss (20 ± 12 ml versus 285 ± 27 ml) and length of stay were significantly less in the LCBDE group (4.2 ± 1.8 days versus 12.6 ± 4.5 days for OCBDE, p < 0.01). The conclusions of this study were that LCBDE could be performed with similar efficacy and morbidity but with a shortened length of stay compared to OCBDE.
There are several limitations of these studies including unclear preoperative selection criteria and unclear length of follow-up. In addition, the use of non-choledochoscopic methods for LCBDE in the study by Rhodes et al., and the use of various methods for closing the choledochotomy (primary closure versus T-tube versus primary closure with ampullary stent) introduce additional heterogeneity to these studies. Finally, it is unclear from the studies how experienced the ERCP operators were. The study by Rhodes has the potential for bias, as the surgeon performing the LCBDEs also performed a majority of the ERCPs, with an initial stone clearance rate of 75 %. This low rate of clearance with postoperative ERCP seems relatively low compared to clearance rates published in the literature of greater than 95 % in some large series [19].
Recommendations Based on the Data
-
1.
Patients with choledocholithiasis discovered on intraoperative cholangiography , should undergo an initial attempt at transcystic LCBDE if feasible (distal stone, stone diameter <9 mm). (Evidence quality low, weak recommendation).
-
2.
Patients with choledocholithiasis in whom transcystic LCBDE is unsuccessful, should undergo either transcholedochal exploration (laparoscopic or open , depending on surgeon experience) if the bile duct is greater than 7 mm, or postoperative ERCP if feasible (available skilled endoscopist and favorable anatomy). (Evidence quality low, weak recommendation).
A Personal View of the Data
The available data show that LCBDE compared to postoperative ERCP has comparable safety and efficacy for the management of choledocholithiasis found on intraoperative cholangiography , and on average results in a shorter hospital stay and fewer numbers of postoperative procedures. The data also show that the efficacy of LCBDE is comparable to that of OCBDE, but with decreased morbidity related to wound complications and a shorter hospital length of stay. These data are consistent with data showing the benefits of both LCBDE and OCBDE compared to ERCP performed in the preoperative setting, which have been previously well-established [2–8, 14]. Transcystic LCBDE appears to have fewer complications compared to transcholedochal LCBDE and may be the most reasonable option to attempt initially, with transcholedochal LCBE or postoperative ERCP reserved as second-line options depending on surgeon experience and access to ERCP. Although not used in the study by Rhodes et al., flexible choledochoscopy is a valuable adjunct that may increase the efficacy of transcystic LCBDE. Future studies with larger numbers of patients are needed to confirm these benefits of LCBDE versus postoperative ERCP, and would be most applicable if they limited LCBDE to a transcystic approach which is a technique that is more likely to be a adopted by surgeons compared to transcholedochal LCBDE.
Despite the evidence for its safety and efficacy, LCBDE continues to remain largely underutilized for the treatment of choledocholithiasis compared to ERCP in the United States, especially in urban settings [20, 21]. Among the many reasons for this may be that LCBDE is viewed by some surgeons as too technically challenging, time-consuming, logistically difficult, unnecessary in the setting of access to skilled endoscopists in some centers, and the fact that LCBDE currently lacks a strong training paradigm. Current training for LCBDE is largely dependent on operative experience alone, which even for experienced surgeons can be infrequent. Simulation-based LCBDE training curricula have recently been developed and may have the potential to improve training for this relatively infrequent clinical scenario [22, 23]. Such training could not only address surgeon skill but also could be applied to improve familiarity of the operating room staff with the procedure and its equipment needs, ultimately improving utilization of LCBDE in practice.
References
Tranter SE, Thompson MH. Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ann R Coll Surg Engl. 2003;85:174–7.
Hammarstrom LE, Holmin T, Stridbeck H, Ihse I. Long-term follow-up of a prospective randomized study of endoscopic versus surgical treatment of bile duct calculi in patients with gallbladder in situ. Br J Surg. 1995;82:1516–21.
Kapoor R, Kaushik SP, Saraswat VA, Choudhuri G, Sikora SS, Saxena R, Kapoor VK. Prospective randomized trial comparing endoscopic sphincterotomy followed by surgery with surgery alone in good risk patients with choledocholithiasis. HPB Surg World J Hepatic Pancreat Biliary Surg. 1996;9:145–8.
Neoptolemos JP, Carr-Locke DL, Fossard DP. Prospective randomised study of preoperative endoscopic sphincterotomy versus surgery alone for common bile duct stones. Br Med J (Clin Res Ed). 1987;294:470–4.
Stain SC, Cohen H, Tsuishoysha M, Donovan AJ. Choledocholithiasis. Endoscopic sphincterotomy or common bile duct exploration. Ann Surg. 1991;213:627–33; discussion 633–624.
Stiegmann GV, Goff JS, Mansour A, Pearlman N, Reveille RM, Norton L. Precholecystectomy endoscopic cholangiography and stone removal is not superior to cholecystectomy, cholangiography, and common duct exploration. Am J Surg. 1992;163:227–30.
Suc B, Escat J, Cherqui D, Fourtanier G, Hay JM, Fingerhut A, Millat B. Surgery vs endoscopy as primary treatment in symptomatic patients with suspected common bile duct stones: a multicenter randomized trial. French Associations for Surgical Research. Arch Surg. 1998;133:702–8.
Targarona EM, Ayuso RM, Bordas JM, Ros E, Pros I, Martinez J, Teres J, Trias M. Randomised trial of endoscopic sphincterotomy with gallbladder left in situ versus open surgery for common bileduct calculi in high-risk patients. Lancet. 1996;347:926–9.
Bansal VK, Misra MC, Garg P, Prabhu M. A prospective randomized trial comparing two-stage versus single-stage management of patients with gallstone disease and common bile duct stones. Surg Endosc. 2010;24:1986–9.
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952–7.
Koc B, Karahan S, Adas G, Tutal F, Guven H, Ozsoy A. Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: a prospective randomized study. Am J Surg. 2013;206:457–63.
Noble H, Tranter S, Chesworth T, Norton S, Thompson M. A randomized, clinical trial to compare endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy with primary laparoscopic bile duct exploration during cholecystectomy in higher risk patients with choledocholithiasis. J Laparoendosc Adv Surg Tech A. 2009;19:713–20.
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145:28–33.
Iranmanesh P, Frossard JL, Mugnier-Konrad B, Morel P, Majno P, Nguyen-Tang T, Berney T, Mentha G, Toso C. Initial cholecystectomy vs sequential common duct endoscopic assessment and subsequent cholecystectomy for suspected gallstone migration: a randomized clinical trial. JAMA. 2014;312:137–44.
Grubnik VV, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc. 2012;26:2165–71.
Nathanson LK, O’Rourke NA, Martin IJ, Fielding GA, Cowen AE, Roberts RK, Kendall BJ, Kerlin P, Devereux BM. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg. 2005;242:188–92.
Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–61.
Martin IJ, Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G. Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg. 1998;228:29–34.
Tantau M, Mercea V, Crisan D, Tantau A, Mester G, Vesa S, Sparchez Z. ERCP on a cohort of 2,986 patients with cholelitiasis: a 10-year experience of a single center. J Gastrointest Liver Dis. 2013;22:141–7.
Poulose BK, Arbogast PG, Holzman MD. National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc. 2006;20:186–90.
Poulose BK, Phillips S, Nealon W, Shelton J, Kummerow K, Penson D, Holzman MD. Choledocholithiasis management in rural America: health disparity or health opportunity? J Surg Res. 2011;170:214–9.
Santos BF, Reif TJ, Soper NJ, Nagle AP, Rooney DM, Hungness ES. Development and evaluation of a laparoscopic common bile duct exploration simulator and procedural rating scale. Surg Endosc. 2012;26:2403–15.
Teitelbaum EN, Soper NJ, Santos BF, Rooney DM, Patel P, Nagle AP, Hungness ES. A simulator-based resident curriculum for laparoscopic common bile duct exploration. Surgery. 2014;156:880–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Santos, B.F., Hungness, E.S. (2016). Management of Suspected Choledocholithiasis on Intraoperative Cholangiography. In: Millis, J., Matthews, J. (eds) Difficult Decisions in Hepatobiliary and Pancreatic Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-319-27365-5_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-27365-5_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-27363-1
Online ISBN: 978-3-319-27365-5
eBook Packages: MedicineMedicine (R0)