Abstract
Background
The SAGES University Colorectal Masters Program is a structured educational curriculum that is designed to aid practicing surgeons develop and maintain knowledge and technical skills for laparoscopic colorectal surgery. The Colorectal Pathway is based on three anchoring procedures (laparoscopic right colectomy, laparoscopic left and sigmoid colectomy for uncomplicated and complex disease, and intracorporeal anastomosis for minimally invasive right colectomy) corresponding to three levels of performance (competency, proficiency and mastery). This manuscript presents focused summaries of the top 10 seminal articles selected for laparoscopic left and sigmoid colectomy for complex benign and malignant disease.
Methods
A systematic literature search of Web of Science for the most cited articles on the topic of laparoscopic complex left/sigmoid colectomy yielded 30 citations. These articles were reviewed and ranked by the SAGES Colorectal Task Force and invited subject experts according to their citation index. The top 10 ranked articles were then reviewed and summarized, with emphasis on relevance and impact in the field, study findings, strength and limitations and conclusions.
Results
The top 10 seminal articles selected for the laparoscopic left/sigmoid colectomy for complex disease anchoring procedure include advanced procedures such as minimally invasive splenic flexure mobilization techniques, laparoscopic surgery for complicated and/or diverticulitis, splenic flexure tumors, complete mesocolic excision, and other techniques (e.g., Deloyers or colonic transposition in cases with limited colonic reach after extended left-sided resection).
Conclusions
The SAGES Colorectal Masters Program top 10 seminal articles selected for laparoscopic left and sigmoid colectomy for complex benign and malignant disease anchoring procedure are presented. These procedures were the most essential in the armamentarium of practicing surgeons that perform minimally invasive surgery for complex left and sigmoid colon pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The practice of surgery is a lifelong learning process. The rapid introduction of new surgical techniques and technologies have made it necessary for trainees and practicing surgeons alike to learn and incorporate these innovations into clinical care. However, it may be difficult for graduating trainees and surgeons already in practice to develop new skills in the absence of additional formal graduate/fellowship training. In recognition of this need, SAGES formed the SAGES University MASTERS Program: A Structured Curriculum for Deliberate, Lifelong Learning [1]. This educational curriculum incorporates a didactic component with educational materials and guidelines endorsed by SAGES, as well as a peer coaching model to facilitate the development and maintenance of surgical skills. The SAGES Masters Program consists of 8 educational pathways: acute care, bariatric biliary, colorectal, flexible endoscopy, foregut, hernia and robotic surgery. Each pathway is further subdivided into 3 levels of performance: competency, proficiency, and mastery.
The SAGES Masters Program in Colorectal Surgery includes 3 anchoring procedures: (1) laparoscopic right colectomy[2], laparoscopic left and sigmoid colectomy for uncomplicated and complex disease, and intracorporeal anastomosis for minimally invasive right colectomy. The educational content will be organized along 3 levels of performance (competency, proficiency, and mastery) to facilitate assessment of the learner’s fund of knowledge, clinical management and decision-making skills, and technical skills. The laparoscopic left and sigmoid colectomy anchoring procedure is split into uncomplicated and complex diseases. This manuscript presents the Top 10 articles relevant to the clinical practice of laparoscopic left and sigmoid colectomy for complex benign and malignant disease. These include advanced procedures such as minimally invasive splenic flexure mobilization techniques, laparoscopic surgery for complicated and/or diverticulitis, complete mesocolic excision, and other techniques (e.g., Deloyers or colonic transposition in cases with limited colonic reach after extended left-sided resection). These procedures were considered to be the most essential in the armamentarium of practicing surgeons that perform minimally invasive surgery for complex left and sigmoid colon pathology.
Methods
The SAGES Masters Program used standardized methodology to identify seminal articles for each anchoring pathway [3]. In this method, a systematic literature review was performed by the SAGES librarian and the top 30 articles relevant to each anchoring procedures were ranked by the chairs of the SAGES Colorectal Task Force based on clinical impact (citation index), multimedia content, relatively recent publication date, quality of study design and scientific content as assessed. This search was initially performed in April 2018 and updated in June 2022. A web-based survey was then sent to all members of the Colorectal Task Force as well as additional subject experts to request additional recommendations for seminal articles and rank the top 10 articles that were selected for each anchoring procedure. Experts were asked to rank articles from most to least pertinent to performance of the given anchoring procedure. A total of 28 responses were obtained and a consensus was reached with the top 10 most pertinent articles in each of the SAGES Masters Colorectal pathway anchoring procedures (Table 1). In some instances, 2 articles were combined as one of the top 10 item, especially if the educational was deemed complimentary such as a study on clinical outcomes, combined with a video demonstration of a given surgical technique. The Colorectal Task Force members were divided into three workgroups, each assigned to a given anchoring procedure: (1) laparoscopic right colectomy; (2) laparoscopic left and sigmoid colectomy for uncomplicated and complex disease; and (3) intracorporeal anastomosis for minimally invasive right colectomy subcommittees. Each task force member was assigned in-depth review of one of the Top 10 articles in that pathway. The reviews of the Top 10 articles for laparoscopic left and sigmoid colectomy for complex pathology are presented here.
The top 10 seminal articles were then reviewed by members of the Colorectal Task Force right colon subcommittee, summaries were compiled and presented here with emphasis on: 1. Why is this a top 10 article? 2. What is unique about this paper? 3. Why is it important to read this paper before you do the relevant procedure? 4. What has been the impact of this paper in the field? 5. What are the study findings? 6. What are the strengths and limitations of paper, and 7. What are the conclusions of this article?
Results
The citation indices for the top 10 articles selected for the Colorectal Pathway complex laparoscopic left/sigmoid colectomy anchoring procedure ranged from 0.0 to 17.8 on Google Scholar, 0.0 to 12.8 on Web of Science, and Altemetric attention scores in the 25th to 94th percentiles (Table 1). Articles in the top 10 list included procedure descriptions and video vignettes of splenic flexure mobilization techniques, colon lengthening procedures such as Deloyers, complete mesocolic excision, as well as assessments of clinical outcomes for minimally invasive approaches to diverticular disease, inflammatory bowel disease, and splenic flexure tumor. They are presented here in order of reviewer’s ranks, with the 1st being the highest rank.
Dumont et al. (2013) options and outcome for reconstruction after extended left hemicolectomy [4]
An extended left hemicolectomy is defined resection of at least the splenic flexure, descending colon, and sigmoid. It may be required in the setting of synchronous left-sided lesions or prior sigmoidectomy. After an extended left hemicolectomy, there is often limited mobility of the ascending colon stump, making a tension-free colorectal anastomosis difficult. In this setting, knowledge of additional salvage techniques, such as a right colon transposition or complete intestinal derotation, may be useful to avoid a total colectomy with ileorectal anastomosis, an ileostomy, or a Hartman’s procedure. This paper was included as one of the Top 10 Articles because it is one of the very few publications that provide technical details and outcomes of these salvage techniques performed to achieve greater colonic reach after open extended left hemicolectomy.
The key operative steps of a right colon transposition involved a 180° rotation in the sagittal plane around the ileocolic pedicle axis after full mobilization of the ascending colon and hepatic flexure. Complete intestinal derotation consists in full mobilization of the ascending colon and hepatic flexure, as well as the base of the small bowel mesentery, followed by a 180° rotation around the superior mesenteric artery axis. Once completed, the right colon is on the left side, and the small bowel is on the right side, similar to a malrotation. Illustrations of both strategies are provided in the article.
The objective of this study was to compare operative and postoperative outcomes after right colon transposition (RCT) or complete intestinal derotation (CID) in patients undergoing open extended left hemicolectomy for colorectal cancer. The authors defined an extended left hemicolectomy as resection of the splenic flexure, descending colon, and sigmoid. A retrospective review of all extended left hemicolectomies that required one of these mobilization techniques over a 10-year period at a single institution was performed. The main outcomes were anastomotic complications (defined a stricture, leak, or inability to create an anastomosis) and overall morbidity.
There was a total of 39 patients that were included in the study, of which 29 underwent RCT (or Deloyers procedure) and 10 CID. Patient characteristics were comparable. The middle colic pedicle was ligated or later required ligation for increased reach in 50% of the CID group and 87% of the RCT group. In one RCT patient, total colectomy with ileorectal anastomosis was required due to ischemia of the remaining colon. The overall incidence of anastomotic complications was 10.2% and was comparable between the RCT and CID groups. There were only three anastomotic leaks overall, with one occurring in the RCT group and two in the CID group. There were no episodes of postoperative obstruction with mean follow-up 20 months. While this is the only available paper that compares these two techniques, it is still limited by possible selection bias and low sample size. In particular, it is not clear why one procedure was favored over the other, suggesting possible selection bias. Furthermore, the indication for surgery included patients with peritoneal carcinomatosis requiring cytoreductive surgery and heated intraperitoneal chemotherapy, which may lead to worse outcomes than patients undergoing colonic resection alone.
In summary, this paper was included in the Top 10 because it is the only paper in the literature that provides any technical description on how to perform complex salvage maneuvers after extended left hemicolectomy in which colonic reach is an issue. In the setting of extended left colectomy with a short residual transverse colon, this study compares two techniques used to achieve additional reach—colonic rotation with right colonic transposition and complete intestinal derotation. Both approaches have comparable short-term outcomes, but RCT is associated with an increased risk of having to ligate the middle colic pedicle and devascularizing additional colon.
Sciuto et al. (2016) laparoscopic deloyers procedure for tension-free anastomosis after extended left colectomy: technique and results [5] and Mishra et al. (2015) problem solving after marginal artery injury during splenic flexure mobilization a video vignette [6]
Colonic reach may be an issue after extended left hemicolectomy in that the proximal transverse colon may not be able to reach down into the pelvis without undue tension. This may occur after resection of synchronous tumors, previous sigmoid resection, or ischemia of the left colon after an interrupted marginal artery. In this setting, several salvage techniques are available, including a Deloyers procedure (i.e., right colon transposition), which involves complete mobilization of the ascending colon and hepatic flexure followed by a 180° counter-clockwise turn to create a colorectal anastomosis. Another technique, the creation of a retroileal window, often allows for preservation of the middle colic artery, which is usually ligated during a Deloyers procedure. Due to the complexity of these maneuvers, they often require conversion to open surgery. These 2 articles were combined and included in the Top 10 articles because they are amongst the few publications that provide technical details, video vignettes, and outcomes of these maneuvers performed laparoscopically. The impact of this paper may not be demonstrable by the number of citations due to the rarity of this procedure and the available literature. However, it is impactful in that it demonstrates that conversion is not absolutely necessary if a Deloyers procedure is required.
The operative steps of the Deloyers procedure include complete mobilization of the ascending colon and hepatic flexure. The middle colic is often ligated during this maneuver to increase length. The small bowel mesentery is similarly mobilized to the root of the mesentery. Once the mobilization is completed, the ascending colon is rotated 180° counter-clockwise and a tension-free colorectal end-to-end anastomosis is created. A video of a laparoscopic Deloyers was included in the paper by Sciuto et al. to increase the understanding of the 180° counter-clockwise rotation [6]. In the article by Mishra et al., creation of retroileal window with passage of the terminal ileum and the transverse colon through the defect to reach the pelvis in a tension-free manner is demonstrated in a video vignette [7].
The objective of the study of Sciuto et al. was to describe the perioperative outcomes of laparoscopic Deloyers procedure after laparoscopic extended left hemicolectomy. A retrospective case series of ten patients who underwent a laparoscopic Deloyers procedure was performed.
Five patients required this procedure for synchronous tumors while the other five had either ischemia or a history of an anastomotic stricture. This procedure requires transection of the right and middle colic arteries, complete mobilization of the right colon and hepatic flexure, and 180° counter-clockwise rotation of the colon so that the terminal ileum lies anterior to the mesentery in the right upper quadrant. Nine cases (90%) could be completed laparoscopically. Conversion was required in 1 case due to extensive adhesions. The mean operative time was 189 min and there was 1 anastomotic leak. At 6 months postoperatively patients were having 2–3 bowel movements per day without incontinence. However, there is limited ability to generate other conclusions due to the small sample size.
In summary, these 2 articles were included in the top 10 because they demonstrate the feasibility of laparoscopic approaches to manage some of the most dreaded complications of extended left colectomy and low anterior resection, namely when colonic reach cannot be achieved and/or when injury to the marginal artery results in an ischemic conduit. These articles represent the largest published case series of laparoscopic Deloyers and describe the technique of retroileoal window, respectively. The articles demonstrate that both techniques can be performed laparoscopically with acceptable postoperative and functional outcomes, and should be considered in order to avoid a total colectomy or fecal diversion.
Benseler et al. (2012) different approaches for complete mobilization of the splenic flexure during laparoscopic rectal cancer resection [7] and Dapri et al. (2017) the three approaches to the colonic splenic flexure mobilization—a video vignette [8]
Laparoscopic splenic flexure mobilization is often required during rectal resection to ensure adequate colonic length for a tension-free anastomosis, especially for low anastomoses. It is critical for surgeons performing minimally invasive left-sided colectomies to be familiar with the different approaches to splenic flexure mobilization in the event of technical difficulties or altered anatomy that may impair one approach. These 2 articles were combined and included in the Top 10 articles because they provide operative technical details including illustrations, video vignettes [4], and clinical outcomes [3] for three different approaches to splenic flexure mobilization: anterior, lateral, and medial mobilization.
With the anterior approach, the dissection is started by dividing the gastrocolic ligament and entering into the lesser sac. The division of the greater omentum is then continued distally along the transverse colon until the splenic flexure is completed mobilized. With the medial approach, the dissection is begun by entering the plane between the colonic mesentery and the retroperitoneum below the IMV at the base of the pancreas. The mesocolon is separated off the anterior surface of the mesentery and the lesser sac is entered. The greater omentum is dissected off the transverse colon laterally. Finally, with the lateral approach, the white line of Toldt is incised first, and the dissection continues along Gerota’s fascia, and the greater omentum is dissected off laterally as well. Videos of these three approaches to splenic flexure mobilization are provided [4].
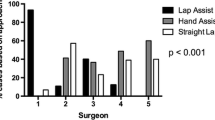
The objective of the paper by Benseler et al. was to compare perioperative outcomes of three different approaches to laparoscopic splenic flexure mobilization during laparoscopic low anterior resection. A retrospective review of 303 patients who underwent laparoscopic splenic flexure mobilization during rectal cancer resection at a single center and by 6 surgeons from 1998 to 2010 was performed [3]. The study population was divided into three groups based on the approach to splenic flexure mobilization. The main study outcomes were intraoperative and postoperative complications.
Most of the study population underwent lateral mobilization (214 patients) over medial (41 patients) and anterior approaches (48 patients). Patient characteristics were comparable. There were significantly more intraoperative complications and conversions in the lateral group. Radial nerve palsies were also more common in the lateral and medial approaches, which the authors suggest was a result of the prolonged Trendelenburg and right lateral positioning during these approaches. Postoperative complications and length of stay were similar in favor of the medial and anterior approaches. A secondary analysis of a single surgeon demonstrated that many of the intraoperative complications in the lateral approach occurred early in the learning curve. The results of this study may be limited by the fact that an important proportion of the intraoperative complications in the lateral approach occurred early in the learning curve of a single surgeon. The authors also state that their surgical approach to splenic flexure mobilization evolved over the study period in favor of the anterior approach, further suggesting an important learning curve effect.
In summary, these two papers were included in the Top 10 because they provide another excellent technical resource for three approaches to laparoscopic splenic flexure mobilization. Based on the results of these studies, the medial and anterior approaches to splenic flexure mobilization should be preferred over the lateral approach. However, surgeons should be familiar with all three approaches in cases where one technique may not be feasible due to difficult anatomy or other technical factors.
Degiuli et al. (2020) segmental colonic resection is a safe and effective treatment option for colon cancer of the splenic flexure: a nationwide retrospective study of the Italian society of surgical oncology-colorectal cancer network collaborative group [9]
The optimal surgical procedure for tumors located at the splenic flexure has been a longstanding source of controversy. The options include an extended right/subtotal colectomy, segmental splenic flexure resection, or an extended left colectomy. Proponents of the extended procedures (either right/subtotal or left) argue that it is technically easier and there is a greater lymph node harvest leading to better oncologic outcomes, whereas proponents of the segmental splenic flexure resection argue that a segmental resection preserves colonic length and function and is associated with adequate nodal harvest and equivalent oncologic outcomes. This paper was included as one of the Top 10 Articles in the updated search because it describes the short- and long-term outcomes for extended versus segmental resections for tumors located at the splenic flexure, as well as outcomes for minimally invasive approach to these tumors.
The objective of this study was to determine if there were any differences in postoperative and oncologic outcomes associated with segmental splenic flexure resection versus extended resections. A cohort study of patients with non-metastatic colon cancer of the splenic flexure from 31 Italian centers performing colorectal surgery between 2006 and 2016 was performed. The splenic flexure was defined as the portion of bowel located from the distal third of the transverse colon to the proximal third of the left colon and divided into two groups: segmental resection of the splenic flexure versus extended resection (either right or left). The procedure choice was at the surgeons’ discretion. Main outcomes included 30-day postoperative outcomes, and oncologic outcomes including overall and progression-free survival.
A total of 1304 patients were included in this study, with 791 (61%) undergoing segmental splenic flexure resection and 513 (39%) undergoing extended resection. Patient and tumor characteristics were well-balanced between the groups, except for higher age and comorbidity index in the segmental resection group. A minimally invasive approach was performed in 58% overall, with a conversion rate of 7%. A higher proportion in the segmental resection group underwent minimally invasive resection (62% vs. 57%). There were no differences in 30-day clinical outcomes, including total complications, anastomotic leak, length of stay, readmissions, and reoperations. In terms of pathologic outcomes, mean resected bowel length was higher in the extended resection arm, although both groups had more than 25% with a distal resection margin < 5 cm. Total lymph node yield was higher in the extended arm (20.1 vs. 16.7 nodes), although the number of positive nodes were similar, as well as the T and N stages. Median follow-up length was 48 months and 46 months for the segmental and extended resection groups, respectively, with no difference in 5-year overall (84% vs 83%) or progression-free (85% vs. 84%) survival. On multiple regression analysis, segmental vs. extended resection was not significantly associated with either overall or progression-free survival. However, the reasons for choosing segmental versus extended resections were not reported, and certain hospitals had low volume. These limitations could have been partly overcome through matching and a hierarchical regression analysis considering variabilities between hospitals.
In summary, this paper was included in the Top 10 because it is the largest study comparing segmental versus extended resection for splenic flexure cancers that is highly generalizable due to the multicenter cohort design. It demonstrated that segmental splenic flexure resection was associated with similar postoperative, pathologic, and oncologic outcomes compared to extended resections, as well as the feasibility of a minimally invasive approach to these tumors.
Bhakta et al. (2016) laparoscopic sigmoid colectomy for complicated diverticulitis is safe: review of 576 consecutive colectomies [10]
Laparoscopic surgery may be difficult in patients with complicated diverticulitis, especially in the context of multiple prior attacks, previous abscess, and fistulas to adjacent organs. Without the full tactile feedback of open surgery, altered planes and fibrosis may render laparoscopic colectomy more difficult and therefore increase the probability of conversion to open surgery. This paper was included as one of the Top 10 Articles because it demonstrates that laparoscopic sigmoid resection for complicated diverticulitis is feasible and safe.
The objective of this study was to compare the 30-day perioperative outcomes of elective laparoscopic sigmoid resection for simple and complicated diverticular disease. A diverticular attack was defined as a physician-documented or self-reported episode of left lower quadrant pain and tenderness, with or without leukocytosis and fever. Complicated diverticular disease was defined as episodes of diverticulitis associated with prior perforation, abscess, fistula, obstruction, or stricture. The authors performed a retrospective review of consecutive patients undergoing elective laparoscopic sigmoid resection for diverticulitis over a 12-year period at a single tertiary center. The main outcome measures of this study were postoperative time to return of bowel function, length of hospital stay, morbidity and mortality.
A total of 576 elective laparoscopic sigmoid resection performed by 4 surgeons were included in the study with 139 (24%) undergoing resection for complicated diverticulitis. The overall conversion rate was 12.8% (including conversion to a hand-assisted approach), with no difference between the simple and complicated diverticulitis patients. Postoperative morbidity was significantly higher in the complicated group which was mostly accounted for by a higher incidence of ileus (8.6% vs. 3.2%), with no difference in anastomotic leak or infectious complications. On multivariate analysis, body mass index (BMI) > 35, EBL > 100 ml and complicated diverticulitis were independent risk factors for postoperative morbidity. Overall length of stay was 5.4 days with no differences between the groups. This paper may be limited by the fact that there were fewer patients in the complicated diverticulitis group, thus limiting the generalizability of the findings to all patients with complicated diverticulitis. Moreover, the definition of recurrent diverticulitis, which was the most common indication for elective resection, included either a physician-documented or self-reported episode of left lower quadrant abdominal pain and tenderness, thus raising the possibility of selection bias.
In summary, this paper was included in the Top 10 because it is the largest consecutive series evaluating outcomes of elective laparoscopic sigmoid colectomy for complicated diverticulitis. This study demonstrated that when performed by experienced surgeons, elective laparoscopic sigmoid resection for complicated diverticulitis was associated with low rates of conversion, anastomotic leaks and infectious complications relative to simple diverticulitis.
Mino et al. (2015) preoperative risk factors and radiographic findings predictive of laparoscopic conversion to open procedures in Crohn’s disease [11]
Laparoscopy is accepted as the standard surgical approach for inflammatory bowel disease and particularly Crohn’s disease (CD). However, conversion to open surgery is common in these complex cases. There are data to suggest that patients who undergo conversion to open surgery have worse perioperative outcomes. Identification of risk factors for conversion may allow surgeons to avoid the potential morbidity and added costs associated with conversion and better select patients who would most benefit from an open approach upfront. This paper was included as one of the Top 10 Articles because it one of the few studies that provide additional risk stratification for patients undergoing laparoscopic surgery for CD.
The objective of this paper was to identify risk factors for conversion to open surgery based on preoperative imaging in patients undergoing planned laparoscopic surgery for CD. A retrospective review of all patients who underwent planned laparoscopic resection for Crohn’s disease over a ten-year period by 13 surgeons at a single high-volume referral center was performed. Patients were included if they had preoperative CT or MRI enterography within three months of surgery. Patients who underwent conversion to open surgery were matched on a 1:3 ratio to patients that had a successful laparoscopic resection based on surgeon, number of previous abdominal surgeries, age, and BMI. Preoperative imaging was reviewed blindly by two independent specialized radiologists. Independent risk factors were identified using multiple logistic regression.
The main indication for surgery was failure of medical management or fistula, with surgical procedures consistent in ileocolic resection (59%), fistula repair, sigmoidectomy, total colectomy and small bowel resection. The overall conversion rate was 14.4%, and 27 patients who were converted to open surgery were matched to 81 patients with successful laparoscopic resection. After adjusting for confounding variables, the presence of an enteroenteric fistula, enterocutaneous fistula in the pelvis, and a pelvic abscess were independent predictors of conversion to open surgery. While this study originates from a high-volume and experienced IBD center, the results are limited by the relatively small sample sizes, as well as heterogeneity in the patient population and surgeons. In addition, conversions were not correlated with clinical outcomes in this study.
In summary, this paper was included in the Top 10 as it provides additional risk stratification for conversion in Crohn’s patients undergoing complex laparoscopic resections, based on preoperative CT and MRI enterography. It serves as a valuable guide for surgeons to better select patients for an open vs. laparoscopic approach in the management of complex Crohn’s pathology, or at least avoid the potential added morbidity and costs associated with unplanned, delayed or reactive conversions.
Kim et al. (2016) complete mesocolic excision and central vascular ligation for colon cancer: principle, anatomy, surgical technique, and outcomes [12]
Complete mesocolic excision (CME) incorporates many of the same principles of total mesorectal excision to colon cancer surgery. The goal of CME is to remove the entire colon and mesocolon intact to minimize tumor spillage and residual tumor in apical lymph nodes to improve oncologic outcomes. The essential elements of CME include sharp dissection along the embryologic planes, central vascular ligation of the feeding pedicle, and adequate resection margins. It is essential for surgeons who wish to adopt this technique to understand the underlying principles and technique of CME. This paper was included in the Top 10 because it provides an exhaustive review of the available evidence that support the basis of CME and its outcomes, as well as the applied anatomy and technical details to perform this demanding operation.
This paper is a narrative review of the oncologic backgrounds, essential components, applied anatomy, laparoscopic technique, short-term, and oncologic outcomes of CME. The plane of mesocolic excision should follow the avascular embryologic planes separating the mesocolon and retroperitoneum along Toldt’s fascia to ensure a smooth surface and avoid any defects. The feeding vascular pedicle should be ligated at its base to maximize lymph node yield and resect the apical nodes, which may harbor skip metastases in 2% of patients. The authors advocate for a tumor-specific CME, whereby for distal transverse and splenic flexure tumors, extended left hemicolectomy with central ligation of the middle colic and left colic pedicles should be performed. Descending colon tumors should undergo left hemicolectomy with central ligation of the left branch of the middle colic and left colic artery with preservation of the root of the inferior mesenteric artery (although it is recommended to clear the apical lymph nodes). A medial to lateral is recommended in the review to facilitate identification of the vascular pedicle origin. This paper provides intraoperative photographs of the expected result of dissection (for example, the anterolateral aspect of the superior mesenteric vein should be completely skeletonized to remove all lymphatic-containing mesentery for a right hemicolectomy). Bowel length margins are recommended to be at least 10 cm in either direction to further maximize lymphatic harvest.
Short- and long-term outcomes were also reviewed. CME was generally associated with increased operative time compared to non-CME surgery, but no difference in overall perioperative complications. Comparing laparoscopic and open CME, the authors reported that laparoscopic CME was associated with increased operative duration and the rate of conversion during laparoscopic CME ranged from 1.9 to 10.4%. However, there were no differences in overall morbidity, but may be associated with quicker return of bowel function and shorter length of stay. The oncologic outcomes of CME in this review were reported favorable with improved disease-free and overall survival. Laparoscopic CME may also have oncologic benefits over open CME. However, the review of the short- and long-term outcomes are not comprehensive and do not report the biases inherent to the included studies.
In summary, this paper was included in the Top 10 Articles because it provides a comprehensive overview of the rationale, anatomic, oncologic and surgical principles of CME, with detailed illustrations of operative details and technical steps during laparoscopic CME. This manuscript serves as an essential guide for surgeons to master the principles and techniques of CME prior to implementation.
Merkel et al. (2016) prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision [13]
Complete mesocolic excision (CME) describes the principles of surgery along the embryologic planes and high vascular ligation for colon cancer. It applies many of the same principles of total mesorectal excision to colon cancer resection. However, it is considered very technically demanding, and as such this procedure has not been widely adopted outside of few specialty centers. There is controversy surrounding its oncologic benefits that must balanced with the increased risk of intraoperative organ and vascular injury associated with CME. This paper was included in the Top 10 Articles because it provided long-term outcomes of CME from 1978 to 2014, which reflect early and late learning curves. It is an important manuscript to read prior to implementing (or not) CME and understand the potential technical risks vs. oncologic benefits of this complex procedure.
The objective of this study was to determine the effect of CME on surgical and oncologic outcomes in patients undergoing colon cancer resection for non-metastatic disease. The authors performed a review of all patients undergoing non-metastatic colon cancer resection from 1978 to 2014. The study group was divided into five time periods: pre-CME (1978–1984), CME development (1985–1994), CME implementation (1995–2002), and two mature CME periods (2003–2009 and 2009–2014), including a total of 2019 consecutive patients. The main outcome measures were locoregional and distant recurrence, as well as overall survival.
There was an overall decrease in the incidence of locoregional recurrence (from 6.7% to 2.1%) and distant metastases (18.9% to 13.3%) over the study period. However, operative morbidity also increased (17.2% to 21.3%) but mortality remained stable. The effect of CME on survival outcomes was less pronounced in stage I–II and was mainly seen for stage III. However, adjuvant systemic therapy was only introduced in 1995, and increased from 0% in the first study period to 79% in the 2009–2014. This is one of the few papers that have provided long-term comparison of the oncologic outcomes of CME and non-CME surgery. However, there are several important limitations. While the long study period is a strength, it also is an important weakness in that there were many changes over time, especially in systemic therapy regimens, as well as other technologies such as imaging techniques that may have allowed for more accurate staging. There is also the possibility of stage migration with the implementation of CME due to the increased lymph node harvest.
In summary, this paper was included in the Top 10 because it is one of the few papers that have provided long-term comparison of the oncologic outcomes of CME and non-CME surgery. These results suggest that CME for colon cancer confers a survival benefit for patients with colon cancer. This effect is especially pronounced for stage III, but this may be biased by the advent of systemic therapy. CME surgery can be considered for patients with more advanced stages of colon cancer.
Vennix et al. (2016) acute laparoscopic and open sigmoidectomy for perforated diverticulitis: a propensity score-matched cohort [14] and Di Saverio et al. (2016) pushing the envelope: laparoscopy and primary anastomosis are technically feasible in stable patients with Hinchey IV perforated acute diverticulitis and gross faeculent peritonitis [15]
Perforated diverticulitis has been traditionally managed surgically with an open approach. There are few high-quality studies comparing laparoscopic and open sigmoid resection for perforated diverticulitis. The study by Vennix et al. demonstrates that laparoscopic Hartmann’s or sigmoid resection with primary anastomosis may be performed with lower morbidity than through the traditional open approach, thus providing clinicians with an evidence-based approach for selecting minimally invasive approaches in the management of perforated diverticulitis.
These 2 articles were combined and included in the Top 10 articles because one provides outcomes from a contemporary propensity matched cohort study of patients with perforated diverticulitis undergoing laparoscopic vs. open sigmoid resection, while the other provides a detailed video description of the technical steps of laparoscopic sigmoid resection for perforated and feculent peritonitis [10].
The main objective of the paper by Vennix et al. was to compare 30-day perioperative outcomes and direct medical costs of laparoscopic and open sigmoid resection for perforated diverticulitis. The cohort study analyzed 307 consecutive patients from 28 Dutch hospitals who were not enrolled in the concurrent laparoscopic lavage LADIES trial, and instead underwent laparoscopic (LS) or open sigmoidectomy (OS) for perforated diverticulitis with procedures consisting in Hartmann’s procedures or sigmoid resection with primary anastomosis. A video demonstration by Di Saverio demonstrates the technical steps of laparoscopic sigmoid resection for perforated diverticulitis demonstrates surgical steps including laparoscopic mobilization of the diseased sigmoid colon with preservation of the left colic artery, followed by exteriorization and resection through a Pfannenstiel incision, followed by end-to-end stapled anastomosis [10].
Among the cohort of 307 patients, 117 were matched 2:1 using propensity score for age, gender, CRP level, Hinchey classification, surgeon, and prior laparotomy. Hartmann’s procedures having been performed in 66% of both groups. Postoperative morbidity (66% vs. 44%) and length of hospital stay were significantly higher in the OS vs. LS group, although there was no significant difference in the incidence of severe complications (Clavien IIIb and above). This resulted in lower overall costs in the laparoscopic cohort and a higher rate of stoma reversal in the laparoscopic Hartmann’s group. While the study cohorts were well-balanced based on propensity score matching, the paper may still be limited by the small sample size, selection biases inherent in the decision to perform a Hartmann’s procedure, and exclusion of patients from matching who may have had more severe comorbidities.
In summary, these studies were included in the Top 10 Articles because Vennix et al. performed a methodologically rigorous study comparing matched cohorts of patients who underwent laparoscopic and open sigmoidectomy for perforated diverticulitis. Di Saverio et al. video vignette illustrates the surgical steps of laparoscopic sigmoid resection with primary anastomosis for perforated purulent diverticulitis. These two articles demonstrate that laparoscopic sigmoidectomy in the emergency setting for patients with perforated diverticulitis can be associated with lower morbidity, shorter length of stay, and higher rates of stoma reversal when performed by experienced surgeons and when compared to an open approach.
Feinberg et al. (2017) oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis [16]
Laparoscopy has traditionally been contra-indicated in patients with T4 colon cancers due to the possibility of en-bloc multivisceral resection, which can be technically challenging laparoscopically. There are concerns about the oncologic adequacy of laparoscopic en-bloc resection of adjacent organs for T4 tumors, and several consensus statements have recommended against it. This paper was included in the Top 10 articles because it provides a methodologically rigorous meta-analysis of all published data evaluating the feasibility and oncologic safety of laparoscopic resection in selected patients with T4 tumors. The analysis was further refined by implementing a matching algorithm to create balanced study cohorts.
The objective of this study was to perform a systematic review of all studies comparing laparoscopic and open resection for T4 colon cancer. An individual patient data systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses of Individual Patient Data (PRISMA-IPD) and was registered in the PROSPERO database. Only studies that were provided individual patient data for laparoscopic and open resection of T4 tumors or for which aggregate data were available, were included. The main outcomes were overall survival, disease-free survival, and resection margins. The Methodological Index for Non-Randomized Studies (MINORS) instrument was used for quality assessment.
There was a total of 5 studies that met the inclusion criteria and provided individual patient or aggregate data, of which all were observational data, for a total of 1268 patients (675 laparoscopic, 593 open). The methodologic quality of these studies was high. Matching was performed using the individual patient data to create balanced cohorts. There were no differences in overall survival, disease-free survival, and resection margins between laparoscopic and open groups. The pooled conversion rate was 18.6%, and open resection was associated with a significantly higher lymph node harvest. However, these results are limited by the fact that all included studies were observational and prone to selection bias. In particular, the inclusion criteria of T4 was based on pathologic assessment rather than on preoperative clinical imaging. As a result, patients with obvious extensive multivisceral invasion may not been offered laparoscopy a priori.
In summary, this paper was included in the Top 10 Articles because it provides evidence to support the use of laparoscopy in selected patients with T4 tumors. Oncologic outcomes were similar between the open and laparoscopic groups, but there was a relatively high rate of conversion. In experienced hands, laparoscopy should not be absolutely contraindicated in the surgical management of T4 colon cancer.
Conclusions
The Top 10 articles reviewed in this manuscript were ranked as the most impactful with respect to clinically relevant content for implementation of laparoscopic left and sigmoid colectomy for complex disease with splenic flexure takedown for complex pathology, one of the 3 anchoring procedures of the SAGES Masters program in colorectal surgery. Outcomes from retrospective comparative and matched cohort studies as well as meta-analyses were reviewed alongside articles demonstrating various surgical techniques of laparoscopic splenic flexure mobilization, right colon transposition and complete intestinal derotation to achieve adequate colonic length, tension-free and viable colorectal anastomoses following extended left colectomy and LAR, and approaches to splenic flexure cancers. The evidence in support and/or against the use of laparoscopy in complicated and perforated diverticulitis, complex IBD, and locally advanced colon cancer laparoscopically, was reviewed and complemented with illustrations and video vignettes on the surgical techniques employed. Finally, several articles reviewed of the surgical principles and techniques of CME, a technique that has become increasingly advocated as associated with superior oncologic outcomes following cancer resections. The content pooled from these 10 publications should serve as a prerequisite towards achieving mastery in laparoscopic surgery for left and sigmoid colon complex pathology.
References
Jones DB, Stefanidis D, Korndorffer JR Jr, Dimick JB, Jacob BP, Schultz L, Scott DJ (2017) SAGES University MASTERS Program: a structured curriculum for deliberate, lifelong learning. Surg Endosc 31:3061–3071
Keller DS, Dapri G, Grucela AL, Melich G, Paquette IM, Shaffer VO, Umanskiy K, Kuhnen AH, Lipman J, McLemore EC, Whiteford M, Sylla P, Colon CCR, S, (2022) The SAGES MASTERS program presents: the 10 seminal articles for the laparoscopic right colectomy pathway. Surg Endosc 36:4639–4649
Stefanidis D, Schultz L, Bostian S, Sylla P, Pauli EM, Oleynikov D, Kurian M, Khaitan L, Cripps MW, Bachman S, Alseidi A, Brunt LM, Asbun H, Jones DB (2020) SAGES masters program: determining the seminal articles for each pathway. Surg Endosc 34:1465–1481
Dumont F, Da Re C, Goere D, Honore C, Elias D (2013) Options and outcome for reconstruction after extended left hemicolectomy. Colorectal Dis 15:747–754
Sciuto A, Grifasi C, Pirozzi F, Leon P, Pirozzi RE, Corcione F (2016) Laparoscopic Deloyers procedure for tension-free anastomosis after extended left colectomy: technique and results. Tech Coloproctol 20:865–869
Mishra A, Gosselink MP, Mortensen NJ, George BD, Cunningham C, Lindsey I, Guy R, Jones OM, Hompes R (2015) Problem solving after marginal artery injury during splenic flexure mobilization - a video vignette. Colorectal Dis 17:174–175
Benseler V, Hornung M, Iesalnieks I, von Breitenbuch P, Glockzin G, Schlitt HJ, Agha A (2012) Different approaches for complete mobilization of the splenic flexure during laparoscopic rectal cancer resection. Int J Colorectal Dis 27:1521–1529
Dapri G, Bascombe NA, Cadiere GB, Marks JH (2017) The three approaches to the colonic splenic flexure mobilization - a video vignette. Colorectal Dis 19:948–949
Degiuli M, Reddavid R, Ricceri F, Di Candido F, Ortenzi M, Elmore U, Belluco C, Rosati R, Guerrieri M, Spinelli A, and Members of the Italian Society of Surgical Oncology Colorectal Cancer Network Collaborative G (2020) Segmental colonic resection is a safe and effective treatment option for colon cancer of the splenic flexure: a nationwide retrospective study of the Italian society of surgical oncology-colorectal cancer network collaborative group. Dis Colon Rectum 63:1372–1382
Bhakta A, Tafen M, Glotzer O, Canete J, Chismark AD, Valerian BT, Stain SC, Lee EC (2016) Laparoscopic sigmoid colectomy for complicated diverticulitis is safe: review of 576 consecutive colectomies. Surg Endosc 30:1629–1634
Mino JS, Gandhi NS, Stocchi LL, Baker ME, Liu X, Remzi FH, Monteiro R, Vogel JD (2015) Preoperative risk factors and radiographic findings predictive of laparoscopic conversion to open procedures in Crohn’s disease. J Gastrointest Surg 19:1007–1014
Kim NK, Kim YW, Han YD, Cho MS, Hur H, Min BS, Lee KY (2016) Complete mesocolic excision and central vascular ligation for colon cancer: principle, anatomy, surgical technique, and outcomes. Surg Oncol 25:252–262
Merkel S, Weber K, Matzel KE, Agaimy A, Gohl J, Hohenberger W (2016) Prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision. Br J Surg 103:1220–1229
Vennix S, Lips DJ, Di Saverio S, van Wagensveld BA, Brokelman WJ, Gerhards MF, van Geloven AA, van Dieren S, Lange JF, Bemelman WA (2016) Acute laparoscopic and open sigmoidectomy for perforated diverticulitis: a propensity score-matched cohort. Surg Endosc 30:3889–3896
Di Saverio S, Vennix S, Birindelli A, Weber D, Lombardi R, Mandrioli M, Tarasconi A, Bemelman WA (2016) Pushing the envelope: laparoscopy and primary anastomosis are technically feasible in stable patients with Hinchey IV perforated acute diverticulitis and gross faeculent peritonitis. Surg Endosc 30:5656–5664
Feinberg AE, Chesney TR, Acuna SA, Sammour T, Quereshy FA (2017) Oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis. Dis Colon Rectum 60:116–125
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Dr. Lee received an investigator-initiated research grant and speaker fees from Johnson & Johnson. Dr. Young-Fadok is on the board of ERAS USA, SAGES, ISDS, and the International ERAS Society. Dr. Hedrick received a research grant from Apple and consulting fees from Ethicon. Dr. Popowich reports consulting fees from Boehringer and Bard. Dr Sylla reports consulting fees from Stryker, Ethicon, Medtronic, Olympus, RedDress, Safeheal, and GI Windows. Drs. Byrn, Cannon, Costedio, Delaney, Obokhare, and Haas report no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, L., Young-Fadok, T., Byrn, J. et al. SAGES masters program: the top 10 seminal articles for the laparoscopic left and sigmoid colectomy pathway for complex disease. Surg Endosc 37, 2538–2547 (2023). https://doi.org/10.1007/s00464-023-09965-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09965-0