Abstract
Introduction
Laparoscopic resection of diverticular disease is typically offered to selected patients. We present the outcomes of laparoscopic colectomy in consecutive patients suffering from either simple diverticulitis (SD) or complicated diverticulitis (CD).
Purpose
To examine the outcomes of laparoscopic sigmoid colectomy for complicated diverticulitis.
Methods
Between December 2001 and May 2013, all patients with diverticulitis requiring elective operation were offered laparoscopic sigmoid colectomy as the initial approach. All cases were managed at a large tertiary care center on the colorectal surgery service. Preoperative, intraoperative, and postoperative variables were prospectively entered into the colorectal surgery service database (CRSD) and analyzed retrospectively.
Results
Of the 576 patients in the CRSD, 139 (24.1 %) had CD. The overall conversion rate was 12.8 % (n = 74). The average BMI was 29.8 kg/m2. The conversion rate for CD was 12.2 %. The return of bowel function time was delayed in the CD group when compared to the SD group (3.1 vs 3.8 days, p = 0.04). The hospital length of stay (HLOS) was similar between the groups (5.1 vs 5.8 days, p = 0.08). The overall anastomotic leak rate was 2.1 % (n = 12). Patients undergoing laparoscopic resection for SD had a postoperative complication rate of 10.0 % (n = 38), whereas those with CD had a postoperative morbidity rate of 19.6 % (n = 24). CD patients who had conversion to an open procedure had an even higher rate of postoperative complications (29.4 %, n = 5, p = 0.35). On non-parsimonious multivariate adjustment, only CD (RR 1.96, 95 % CI 1.11–3.46, p = 0.02) was found to be an independent risk factor for the development of postoperative complications.
Conclusions
Complicated diverticulitis did not affect the conversion rate to an open procedure. However, patients with CD are prone to postoperative complications. The laparoscopic approach to sigmoid colectomy is safe and preferable in experienced hands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diverticular disease is a common condition that will affect approximately 50 % of Americans by the age of 60 years and nearly all by the age of 80 years [1–3]. Elective surgery for diverticulitis is technically challenging, irrespective of whether a laparoscopic approach is chosen. Until the early 1990s, sigmoid colectomy was exclusively performed utilizing a midline laparotomy. With the introduction of laparoscopic cholecystectomy in 1987, the era of minimally invasive gastrointestinal surgery emerged; however, diverticulitis was thought to be a relative contraindication [2, 4–6].
Guidelines from the American Society of Colon and Rectal Surgeons recommend the laparoscopic approach to elective colectomy when the expertise is available [2]. This recommendation is based on multiple trials that have demonstrated several advantages of laparoscopic colectomy over the open approach. These include decreased operative blood loss, less pain, shorter time to return of bowel function (ROBF), shorter hospital length of stay (HLOS), and improved quality of life [7–9].
However, the surgical literature does not uniformly support the laparoscopic approach to complicated diverticular disease [10, 11]. Therefore, patients with complicated diverticulitis (CD) were historically deemed unsuitable for laparoscopic resection and have been excluded from numerous studies that evaluated the effectiveness of the minimally invasive approach [12–14].
Methods
A retrospective review was performed between December 2001 and May 2013, during which consecutive patients with diverticulitis requiring elective surgery were offered laparoscopic sigmoid colectomy as the initial approach. There were no exclusion criteria. All cases were managed at Albany Medical Center, a large tertiary care center on the colorectal surgery service. Data points of all patients undergoing elective sigmoid resection for diverticular disease by any of the four colorectal surgeons were collected into the colorectal surgery service database (CRSD). Patient data included age, gender, body mass index (BMI), previous abdominal operations, indication for sigmoid resection (recurrent diverticulitis, abscess, fistula, stricture, and immunocompromised state), American Society of Anesthesiology (ASA) class, number of previous diverticulitis attacks, and number of attacks requiring hospitalization. A diverticular attack in these patients with diverticulitis was defined as either a physician-documented or self-reported episode of left lower quadrant abdominal pain and tenderness, with or without fever and leukocytosis. CD included those episodes associated with contained perforation, abscess, fistula, obstruction, or stricture.
Operative variables included intraoperative Hinchey class, estimated blood loss (EBL), operative time, and complications. Intraoperative Hinchey classification included stages 1–4. Stage 1 was the presence of pericolic or mesenteric abscess; stage 2 was a walled-off pelvic abscess; stage 3 was generalized purulent peritonitis; and stage 4 was generalized fecal peritonitis [15].
Our operative technique entailed selective takedown of the splenic flexure, mandatory identification of the left ureter, exteriorization through a 4-cm infraumbilical midline incision, intracorporeal end-to-end anastomosis, followed by a pneumatic air leak test. The use of hand ports and larger incisions was considered conversion to an open procedure.
Postoperative variables evaluated included time to ROBF, HLOS, morbidity, and mortality. ROBF was defined as the postoperative day when patients were able to tolerate a diet or reported passage of flatus. Postoperative ileus was defined as the intolerance of oral intake or the absence of flatus by the seventh postoperative day. Postoperative morbidity included superficial surgical site infection (SSI), deep incisional SSI, organ space SSI, anastomotic leak, incisional hernia, Clostridium difficile infection, and ileus.
Statistical analysis was performed by STATA, version 11.1. Bivariate and multivariate logistic regression was used to assess for independent risk factors for postoperative complications.
Results
During the 12-year study period, 576 patients required elective sigmoid colectomy for diverticulitis, and all were approached laparoscopically. No patients were excluded. The mean age of the patients was 55.7 years (range 23–90 years), and 47.0 % were male (n = 263). The average ASA class was 2.2 (range 1–4). The average BMI was 29.8 (range 17.6–62.1). The mean follow-up time was 12 months (range 3–36 months), and during this period there were no episodes of recurrence and no deaths (Table 1).
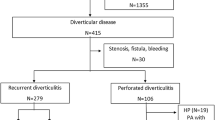
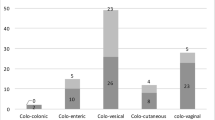
The most common indication for operative intervention was recurrent diverticulitis (n = 437, 75.9 %), followed by fistula (n = 63, 10.9 %), abscess (n = 48, 8.3 %), stricture (n = 21, 3.6 %), perforated diverticulitis (n = 4, 0.7 %), and immunocompromised state (n = 3, 0.5 %). The rate of CD was 24.1 % (n = 139). The average number of diverticulitis attacks prior to operative intervention was 3.1 (range 1–12) with approximately one attack requiring hospitalization (range 0–7). A total of 311 patients had undergone previous abdominal operations, most commonly appendectomy (n = 50), cholecystectomy (n = 28), small bowel resection (n = 26), total abdominal hysterectomy (n = 25), and cadaveric renal transplant (n = 3). A total of 442 (76.7 %) patients had an intraoperative Hinchey score of 1, whereas 123 (21.4 %) had an intraoperative Hinchey score of 2, and 11 (1.9 %) had an intraoperative Hinchey score of 3 (Fig. 1). For 138 patients, a second procedure was performed concurrently with the sigmoid colon resection (Fig. 2).
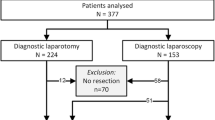
The overall conversion rate from laparoscopic to open sigmoid resection was 12.8 % (n = 74) (Fig. 3). The conversion rate was 13.0 % (n = 57) for simple diverticulitis (SD) and 12.2 % (n = 17) for CD (Table 2).
With regard to anastomotic integrity, the leak rates for overall, SD, and CD were 2.1 % (n = 12), 2.3 % (n = 10), and 1.4 % (n = 2), respectively (Table 3). Furthermore, patients with complicated diverticular disease who underwent successful laparoscopic resection had an anastomotic leak rate of 1.6 %.
The overall postoperative complication rate was 14.2 % (n = 82), with a 12.1 % (n = 53) complication rate for SD and 20.9 % (n = 29) for CD. This included all patients regardless of laparoscopic completion or conversion to an open procedure. The rates of postoperative complications for completed laparoscopic colectomies were 10.0 % for SD and 19.7 % for CD (p = 0.005). Patients completing laparoscopic resection for CD had a postoperative morbidity rate of 19.7 % (n = 24), as opposed to 29.4 % in CD patients requiring conversion (n = 5, p = 0.35) (Table 3). Postoperative infection rates were similar between SD and CD and included superficial incisional SSI (3.9 vs 6.5 %), organ or space SSI (2.1 vs 3.6 %), and Clostridium difficile infection (2.9 vs 2.9 %). The rate of incisional hernia was also similar (1.6 vs 2.9 %). However, the rate of ileus was significantly higher in the CD group (3.2 vs 8.6 %, p = 0.007) (Table 4).
The ROBF time was delayed in the CD group when compared to the SD group (3.1 vs 3.8 days, p = 0.04). The HLOS was similar between the groups (5.1 vs 5.8 days, p = 0.08) (Table 4).
Patients with a BMI of 35 or more had a complication rate of 23.0 % (n = 23) compared with a complication rate of 12.4 % (n = 59) for patients with a BMI <35 (p = 0.006). The average operative time for patients with a BMI of 35 or more was 141.6 min compared with 129.5 min for patients with a BMI <35 (p < 0.2).
On multivariate adjustment, in the non-parsimonious model, when the contributions of risk factors that were found to be significant on the bivariate analysis were accounted for, only CD was found to be a significant risk factor for the development of postoperative complications (RR 1.96, 95 % CI 1.11–3.46, p = 0.02). In the parsimonious model, CD (RR 2.07, 95 % CI 1.33–3.22, p = 0.001), conversion to an open procedure (RR 2.21, 95 % CI 1.41–3.44, p = 0.0001), BMI ≥ 35 (RR 2.10, 95 % CI 1.28–3.46, p = 0.0.004), and EBL greater than 100 mL (RR 1.06, 95 % CI 1.01–1.11, p = 0.02) were found to be independent risk factors for the development of complications.
Discussion
In this study, we showed that the rate of conversion to an open procedure was independent of the complexity of diverticulitis (13.0 % SD vs 12.2 % CD). However, patients with CD as well as those undergoing conversion experienced increased rates of postoperative complications. To our knowledge, this is the largest series of consecutive cases demonstrating laparoscopic sigmoid colectomy for CD to be safe with low conversion rates, low leak rates, and without disease recurrence and mortality.
Numerous studies have proven the feasibility of the laparoscopic approach to SD [8, 10, 13]. However, practice guidelines have been reluctant to recommend laparoscopy as the gold standard for CD [14, 15]. The concern is that the primary reason to undergo conversion, is the inflammatory processes due to diverticular abscess, fistula, and stricture. Finding similar conversion rates between SD and CD contributes to the evidence supporting the laparoscopic approach to all cases of diverticulitis requiring surgical intervention.
The higher rate of morbidity in the CD group reported in the literature and in our study is a reflection of the complex nature of the disease process [16, 17]. Patients with CD were 1.7 times more likely than patients with SD to develop a postoperative complication. The authors hypothesized that this effect was not dependent on the type of procedure (e.g., laparoscopic or laparoscopic converted to open) but rather the disease process itself. To verify this, statistical analysis controlled for the operative approach. A subgroup analysis of our CD cohort showed no statistically significant difference in the complication rates whether the operation was completed laparoscopically or not (19.7 % laparoscopic vs 29.4 % laparoscopic converted to open, p = 0.35). It should be noted that when laparoscopic resection is successful, patients benefit from the advantages of minimally invasive surgery, making it worthwhile to attempt laparoscopy [18].
Statistical analysis identified BMI greater than 35, EBL greater than 100 mL, and CD as independent risk factors for the development of postoperative complications. Interestingly, prior abdominal surgery, number of diverticular attacks, and intraoperative Hinchey classification did not play significant roles in the development of postoperative complications in this patient population [6, 8]. Therefore, these traditional risk factors for conversion should not be seen as contraindications to the laparoscopic approach.
It is important to acknowledge that a longer duration of ileus was found in the CD group. We attributed this to the longer operative time required, as well as the increased EBL, associated with these cases. This longer duration of ileus corresponds to the increased length of ROBF that was seen in the CD group, a finding that correlates with prior studies linking increased operative times to increased duration of ROBF [19–22].
Based on this data, we conclude that experienced surgeons should attempt laparoscopic colectomy on all patients, with acceptable operative time, complications, and conversions.
References
Corman ML (2005) Colon and rectal surgery, 5th edn. Lippincott Williams & Wilkins, Philadelphia
Feingold D, Steele SR, Lee S et al (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57(3):284–294
Parks TG (1969) Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J 4(5684):639–642
Bartus CM, Lipof T, Sarwar CM et al (2005) Colovesical fistula: not a contraindication to elective laparoscopic colectomy. Dis Colon Rectum 48(2):233–236
Scheidbach H, Schneider C, Rose J et al (2004) Laparoscopic approach to treatment of sigmoid diverticulitis: changes in the spectrum of indications and results of a prospective, multicenter study on 1,545 patients. Dis Colon Rectum 47(11):1883–1888
Bouillot JL, Berthou JC, Champault G et al (2002) Elective laparoscopic colonic resection for diverticular disease: results of a multicenter study in 179 patients. Surg Endosc 16(9):1320–1323
Senagore AJ, Stulberg JJ, Byrnes J, Delaney CP (2009) A national comparison of laparoscopic vs. open colectomy using the National Surgical Quality Improvement Project data. Dis Colon Rectum 52(2):183–186
Carbajo MA, Martin del Olmo JC, Blanco JI et al (1999) Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc 13(3):250–252
Kuhry E, Saetnan E, Graeslie H, Gaupset R (2007) Laparoscopic surgery for colorectal cancer. Tidsskrift for den Norske laegeforening:tidsskrift for praktisk medicin, ny raekke. 127(22):2946–2949
Hassan I, Cima RR, Larson DW et al (2007) The impact of uncomplicated and complicated diverticulitis on laparoscopic surgery conversion rates and patient outcomes. Surg Endosc 21(10):1690–1694
Gervaz P, Pikarsky A, Utech M et al (2001) Converted laparoscopic colorectal surgery. Surg Endosc 15(8):827–832
Faynsod M, Stamos MJ, Arnell T, Borden C, Udani S, Vargas H (2000) A case–control study of laparoscopic versus open sigmoid colectomy for diverticulitis. Am Surg 66(9):841–843
Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD (1997) Laparoscopic surgery for diverticulitis. Surg Endosc 11(3):264–267
Collins D, Winter DC (2014) Laparoscopy in diverticular disease: controversies. Best Pract Res Clin Gastroenterol 28(1):175–182
Kockerling F, Schneider C, Reymond MA et al (1999) Laparoscopic resection of sigmoid diverticulitis. Results of a multicenter study. Laparoscopic Colorectal Surgery Study Group. Surg Endosc 13(6):567–571
Chapman J, Davies M, Wolff B et al (2005) Complicated diverticulitis: is it time to rethink the rules? Ann Surg 242(4):576–581; discussion 581-573
Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE (2013) Laparoscopic versus open Hartmann procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum 56(1):72–82
Liberman MA, Phillips EH, Carroll BJ, Fallas M, Rosenthal R (1996) Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc 10(1):15–18
Caputo D, Caricato M, La Vaccara V, Capolupo GT, Coppola R (2014) Conversion in mini-invasive colorectal surgery: the effect of timing on short term outcome. Int J Surg 12(8):805–809
Keller DS, Bankwitz B, Woconish D et al (2014) Predicting who will fail early discharge after laparoscopic colorectal surgery with an established enhanced recovery pathway. Surg Endosc 28(1):74–79
Blake MF, Dwivedi A, Tootla A, Tootla F, Silva YJ (2005) Laparoscopic sigmoid colectomy for chronic diverticular disease. J Soc Laparoendosc Surg 9(4):382–385
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Avinash Bhakta, Marcel Tafen, Owen Glotzer, Jonathan Canete, A. David Chismark, Brian T. Valerian, Steven C. Stain, and Edward C. Lee have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Bhakta, A., Tafen, M., Glotzer, O. et al. Laparoscopic sigmoid colectomy for complicated diverticulitis is safe: review of 576 consecutive colectomies. Surg Endosc 30, 1629–1634 (2016). https://doi.org/10.1007/s00464-015-4393-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4393-5