Abstract
Introduction
Achalasia is a debilitating primary esophageal motility disorder. Heller myotomy (HM) is a first-line therapy for the treatment of achalasia patients who have failed other modalities. Other indications for HM include diverticulum, diffuse esophageal spasm, and esophageal strictures. However, long-term outcomes of HM are unclear. This study aims to assess incidence of reintervention, either endoscopically or through minimally invasive or resectional procedures, in patients who underwent HM in New York State.
Methods
The Statewide Planning and Research Cooperative System (SPARCS) administrative longitudinal database identified 1817 adult patients who underwent HM between 2000 and 2008 for achalasia, esophageal diverticulum, diffuse esophageal spasm, and esophageal strictures, based on ICD-9 and CPT codes. Through the use of unique identifiers, patients requiring reintervention were tracked up to 2016 (for at least 8 years follow-up). Primary outcome was incidence of subsequent procedures following HM. Secondary outcomes were time to reintervention and risk factors for reintervention.
Results
Of the 1817 patients who underwent HM, 320 (17.6%) required subsequent intervention. Of the 320 patients, 234 (73.1%) underwent endoscopic reinterventions, 54 (16.9%) underwent minimally invasive procedures, and 32 (10%) underwent resectional procedures as their initial revisional intervention. Of the 234 patients who underwent endoscopic reintervention as their initial revisional procedure, only 40 (16.8%) required subsequent surgical procedures. Over a mean follow-up of 7.0 years, the mean time to a subsequent procedure was 4.3 ± 3.74 years. Reintervention rates after 10 years following HM for achalasia, diverticulum ,and other indication were 24.4%, 12.6%, and 37%, respectively.
Conclusion
The majority of HM reinterventions were managed solely by endoscopic procedures (60.6%). Heller myotomy remains an excellent procedure to prevent surgical reintervention for achalasia and diverticulum.
Graphic Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achalasia is a rare (incidence 1.6/100,000) esophageal motility disorder that is progressive and incurable [1]. Treatment focuses on symptom palliation and include pharmacological, endoscopic, and surgical interventions. Endoscopic options include botulinum toxin injection, pneumatic dilatation, and peroral endoscopic myotomy (POEM) [2]. Botulinum toxin injections have been shown to be effective, but the effect diminishes at 6 months [3]. POEM is a relatively newer endoscopic treatment modality, and short-term outcomes have shown it to be very effective [4]. Clinical guidelines from the American College of Gastroenterology recommend pneumatic dilatation or Heller myotomy (HM) as first-line therapy in patients with low surgical risk [5]. One systematic review concluded that HM provided better symptomatic relief when compared to endoscopic modalities [6]. Symptomatic improvement has been shown in 89% of patients at 3-year follow-up, and 75% at 15-year follow-up [6, 7].
Despite the established efficacy of HM, data demonstrating the long-term efficacy and reintervention after HM are limited. At a single institution, 20% of 248 patients required subsequent interventions after HM at a median follow-up of 3 years [8]. One population-based study of employed Americans demonstrated that 9.5% of 871 patients required a reintervention in the first year after HM [9]. Furthermore, HM has been extended to treat other conditions including diffuse esophageal spasm, esophageal diverticulum, and esophageal stricture [10,11,12,13,14]. However, there is a paucity of multi-institutional, long-term data demonstrating the long-term efficacy of HM for non-achalasia disorders.
The purpose of this study is to evaluate the incidence of reintervention and reoperation after HM for different indications in New York State over a 15-year period. In addition, we sought to identify risk factors for reinterventions and reoperations.
Methods
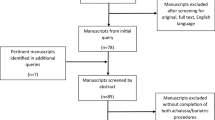
The New York Statewide Planning and Research Cooperative System (SPARCS) administrative database was used to identify patients who underwent HM between January 1, 2000 and December 31, 2008. SPARCS is a longitudinal, all payer data reporting system that documents patient-level detail including demographics, diagnoses, and treatments for every hospital or surgery center encounter in the state of New York [15]. Each patient is assigned a unique identifier and can be followed across time and institution. Through the use of ICD-9 and CPT diagnostic and procedural codes, all patient undergoing HM for specific diagnostic codes were extracted. The extracted records were stratified by indication for procedure (achalasia, diverticulum and other) through primary diagnosis codes (530.0, 530.6, and 530.3, 530.5, 553.3). Patients were tracked for a minimum of 8 years (2000–2016) post procedure to assess for reintervention or reoperation. Reintervention and reoperation were categorized as endoscopic (pneumatic dilation, botox injections), minimally invasive (reoperative myotomy, fundoplication, hiatal hernia repair), and resectional (esophagogastrostomy, esophagoenterostomy, esophagocolostomy, esophagogastrectomy, esophagectomy). Exclusion criteria included: age < 8, missing identifiers, duplicated records, and patients who underwent HM with a primary diagnosis other than achalasia, diverticulum, esophageal dyskinesia/spasm, esophageal stenosis, and hiatal and paraesophageal hernia. The study was reviewed by the Institutional Review Board and deemed exempt. The need for written informed consent was exempt.
Patient demographics, indication for HM, comorbidities, and complications at the primary procedure were identified as potential risk factors for reintervention or reoperation. Indication for HM is defined as the primary diagnosis coded for the hospital record encounter for the index procedure. Frequency of reinterventions or reoperation was stratified by indication for HM. Primary outcome was incidence of subsequent esophageal procedures following HM. Secondary outcomes were time to reintervention and risk factors for reintervention.
Chi-square tests with exact P-values based on Monte Carlo simulation were utilized to examine the marginal association between categorical variables and patients’ indication for HM (achalasia vs diverticulum vs other), as well as between types of reintervention/reoperation. Wilcoxon rank sum tests (for variables with 2 levels) and Kruskal–Wallis tests (for variables with > = 3 levels) were used to compare unadjusted marginal differences in follow-up time among different primary diagnosis groups, as well as the difference in time to reinterventions by reintervention types and patients’ primary diagnosis. Cumulative incidences of reinterventions/reoperation (any type of reintervention, endoscopic procedure, minimally invasive procedure, resectional procedure) at a specific time point with death as a competing risk event were estimated using cuminc() function, cmprsk package in R. Univariate proportional sub-distribution hazards models (Fine-Gray models) were utilized to examine the marginal association between categorical variables and the incidence of reinterventions/reoperation. Indication for HM and other factors related to each outcome that were significant (p-value < 0.05) based on univariate analysis were further considered in multivariable Fine-Gray models. Forward selection was implemented based on p-values in the analysis of the risk for resectional procedure because of low number of patients with such outcomes[16]. In Fine-Gray models, a hazards ratio (HR) > 1 indicated higher risk to have reintervention, while an HR < 1 indicated lower risk. Statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and significance level was set at 0.05.
Results
A total of 1817 patients underwent HM between 2000 and 2008. Of these, the primary indication for HM was achalasia in 1549 (85.25%) patients, diverticulum in 213 (11.72%) patients, and others in 53 (3.03%) patients. Patient demographics, comorbidities, clinical information, and 30-day complications stratified by indication for HM are shown in Table 1. Patients who underwent HM for diverticulum had the highest median age than those who underwent HM for achalasia or other indications (73 vs 49 vs 64, p < 0.0001). Other significant differences amongst the three groups were insurance type, geographic region in NYS where the surgery was performed and average length of hospital stay. Patients who underwent HM for diverticulum or other conditions were more likely to have comorbidities as compared to achalasia (72.3% vs 61.81% vs 47.06%, p < 0.001). Furthermore, patients who underwent HM for diverticulum or other conditions were more likely to have complications as compared to achalasia (20.19% vs 23.64% vs 11.88%, p < 0.0001).
Among the 1817 HM patients, 320 (17.6%) required a subsequent intervention. Of those requiring a subsequent intervention, 279 (87.19%) were achalasia patients, 22 (6.87%) were diverticulum patients, and 19 (5.94%) were other patients.
In the achalasia reintervention cohort (N = 279), 207 (74.2%) underwent endoscopic reintervention, 45 (16.1%) underwent minimally invasive procedures, and 27 (9.7%) underwent resectional procedures as their initial revisional intervention. Of the 207 patients who underwent endoscopic reintervention as their initial revisional procedure, 170 (81.3%) were managed solely by endoscopic interventions and 37 (17.7%) required subsequent surgical (minimally invasive or resectional) procedures. In the diverticulum reintervention cohort (N = 22), 14 (63.6%) underwent endoscopic reintervention, 5 (22.7%) underwent minimally invasive procedures and 3 (13.6%) underwent resectional procedures as their initial revisional intervention. In the other indications reintervention cohort (N = 19), 13 (68.4%) underwent endoscopic reinterventions, 4 (21.1%) underwent minimally invasive procedures, and 2 (10.5%) underwent resectional procedures as their initial revisional intervention. This is shown in Table 2. Overall, 194 of the 320 patients (60.6%) who required reinterventions after HM, underwent endoscopic therapies alone.
Over a mean follow-up of 7.0 years (range 0 to 16.9 years), the average time to any reintervention or reoperation was longest in the achalasia group compared to diverticulum and others (4.5 years vs 2.9 years vs 3.3 years, p = 0.0284). No statistical difference amongst the 3 indications was seen when looking at time to each subgroup of procedure as shown in Table 3.
The cumulative incidence curves for any subsequent procedures among all HM patients stratified by procedure type and indication for HM are shown in Figs. 1 and 2. The reintervention or reoperation rates for achalasia patients at 1 years, 5 years, 10 years, and 15 years are 5.7%, 13.6%, 24.4%, and 31.4%.
Supplemental Table A describes the risk factors associated with having any type of subsequent procedure after adjusting for possible confounding factors. Indication for HM was significantly related to subsequent reintervention (p = 0.0005). Patient with diagnosis other than achalasia and diverticulum were more likely to have any subsequent procedure (HR 20.12 95% CI 1.223–3.308), while patients with diverticulum were less likely to have any subsequent procedure (HR 0.538 95% CI 0.343–0.845). There was no statistical significant relationship between hospital volume of Heller myotomy (low volume = ≤ 6 cases, high volume = > 6 cases annually) and need for subsequent procedure. Patients with comorbidities such as renal failure (HR 2.573 95% CI 1.076–6.156, p = 0.0337) and depression (HR 1.739 95% CI 1.044–2.897, p = 0.0336) and complications such as abscess formation (HR 25.562 95% CI 3.054–213.962, p = 0.0028) and enteritis (HR 5.803 95% CI 4.829–6.974, p = < 0.001) were more likely to have subsequent procedures. See Supplemental Table B for risk factors associated with subsequent endoscopic, minimally invasive, and resectional procedures. (Supplemental Table B).
Discussion
Although HM has long been established as the procedure of choice for treatment of severe achalasia [17], the long-term rates of reintervention and reoperation have been unclear. Previous studies suggest that such rates range from 4.9% to 29.4% [8, 9, 18,19,20]. However, these studies are specific to achalasia patients over a shorter follow-up period with a smaller cohort. To our knowledge, this is the largest study in identifying rates and risk factors for HM reintervention/reoperation across different interventions. Importantly, because of the population-based approach, the potential for loss to follow-up is limited.
The present study suggests that the 10 year rates of reintervention/reoperation are highest when HM is performed for other indications compared to achalasia and diverticulum (37% vs 24.3% vs 12.6%, respectively). The other indications include esophageal spasms, esophageal strictures, paraesophageal hernia, and hiatal hernia. HM has been used to treat esophagogastric junction outflow obstruction and diffuse esophageal spasms (DES) after failure of medical therapy [10, 21, 22]. Leconte et al. reported failure to improve DES symptoms in 25% of patients following myotomy in a small study with 3 year follow-up.[23]. Myotomy may not be successful in the treatment of DES as it is hypothesized to decrease the intensity of the contractions but not the frequency [21]. Treatment of esophageal stricture with myotomy has only been successful and demonstrated in small case series [13, 14]. All 3 patients in one study [13] and 2 patients in a second study [14] demonstrated success with myotomy with a median follow-up of 10 years and 5 years, respectively.
The results of this study show a lower reintervention or reoperation rate over 15 years for diverticulum patients compared to achalasia patients (16.8% vs 31.4%). However, the baseline demographics and comorbidities are markedly different between the two patient populations. Patients who underwent HM for diverticulum are older (median age 73 vs 49) and more likely to have comorbidities (congestive heart failure, valvular disease, pulmonary disease, hypertension) compared to the achalasia group. Age and comorbidities are independent prognostic factors for postoperative complications and increased risk of mortality following elective surgery [24, 25]. Surgical management of patients is heavily influenced by patient’s age and frailty score [26]. In this study, physicians may have advised against subsequent procedures in diverticulum patients. However, the results of our study are consistent with a previous study in which esophageal diverticulum is a favorable patient characteristic for laparoscopic HM [27].
In prior studies that investigated the timing to reinterventions, patients had the highest risk in the first 12 months after HM [8, 28,29,30,31]. One study of 248 patients who underwent HM for achalasia showed reinterventions occurred in 12% and 28% of the patients at 1 year and 5 years, respectively [8]. A vast majority (82%) of their reinterventions were endoscopic. Our study demonstrated lower rates of reintervention at 5.7% and 13.6% at 1 year and 5 years, respectively. The majority of our reinterventions were endoscopic, which is consistent with prior studies [8, 32].
Other studies have identified longer duration of symptoms, male patients and low lower esophageal sphincter pressures preoperatively as risk factors for HM failure [33,34,35]. We identified comorbidities in renal failure and depression and complications of abscess and enteritis as independent risk factors for any type of reintervention/reoperation. These risk factors can help with patient expectations and optimize postoperative surveillance. Further research is needed to validate these risk factors.
There are several limitations of this study. First, this is a retrospective study using an administrative database. Since this data are extracted from a single state, our findings cannot be generalizable to other geographic areas. Patients who received subsequent procedures at other states are not included in the current analysis. Clinical information is not provided and thus patient history, symptom severity and prior treatments cannot be analyzed. In addition, we are unable to identify technical factors contributing to the need for reintervention. There is the potential of miscoding diagnosis and procedure codes. Furthermore, there are currently no ICD-9, ICD-10 or CPT codes for POEM. We were unable to include POEM as an reintervention, although the number of PEOM procedures performed prior to 2016 is likely limited. We calculated success of HM based on freedom from reintervention or reoperation, rather than symptoms.
Conclusion
HM is an effective treatment for achalasia and esophageal diverticulum with long-term success rates of 68.6% and 83.2% at 15 years. The majority of reinterventions after HM were managed endoscopically (60.6%). Given the rate of reinterventions, it is imperative to set patient’s expectations when planning for HM and to maintain long-term surveillance postoperatively.
References
O’Neill OM, Johnston BT, Coleman HG (2013) Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 19:5806–5812
Leyden JE, Moss AC, MacMathuna P (2014) Endoscopic pneumatic dilation versus botulinum toxin injection in the management of primary achalasia. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005046.pub3
Martinek J, Siroky M, Plottova Z, Bures J, Hep A, Spicak J (2003) Treatment of patients with achalasia with botulinum toxin: a multicenter prospective cohort study. Dis Esophagus 16:204–209
Kroch DA, Grimm IS (2018) POEM for Achalasia. Am Surg 84:489–495
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1249 (quiz 1250)
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstatter M, Lin F, Ciovica R (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–57
Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henriquez A (2006) Very late results of esophagomyotomy for patients with achalasia: clinical, endoscopic, histologic, manometric, and acid reflux studies in 67 patients for a mean follow-up of 190 months. Ann Surg 243:196–203
Raja S, Schraufnagel DP, Blackstone EH, Murthy SC, Thota PN, Thuita L, Lopez R, Gabbard SL, Ray MN, Wadhwa N, Sanaka MR, Zanoni A, Rice TW (2019) Reintervention after Heller myotomy for achalasia: is it inevitable? Ann Thorac Surg 107:860–867
Ehlers AP, Oelschlager BK, Pellegrini CA, Wright AS, Saunders MD, Flum DR, He H, Farjah F (2017) Achalasia treatment, outcomes, utilization, and costs: a population-based study from the United States. J Am Coll Surg 225:380–386
Schlottmann F, Shaheen NJ, Madanick RD, Patti MG (2017) The role of Heller myotomy and POEM for nonachalasia motility disorders. Dis Esophagus 30:1–5
Oelschlager BK (2007) Surgical options for treatment of esophageal motility disorders. Gastroenterol Hepatol (N Y) 3:687–689
Andreoll NA, Lope LR, Malafai O (2014) Heller’s myotomy: a hundred years of success! Arq Bras Cir Dig 27:1–2
Kawahara H, Imura K, Yagi M, Kubota A (2001) Clinical characteristics of congenital esophageal stenosis distal to associated esophageal atresia. Surgery 129:29–38
Anderson KD, Acosta JM, Meyer MS, Sherman NJ (2002) Application of the principles of myotomy and strictureplasty for treatment of esophageal strictures. J Pediatr Surg 37:403–406
Chen X, Wang Y, Schoenfeld E, Saltz M, Saltz J, Wang F (2017) Spatio-temporal analysis for New York State SPARCS data. AMIA Jt Summits Transl Sci Proc 2017:483–492
Peduzzi P, Concato J, Feinstein AR, Holford TR (1995) Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 48:1503–1510
Nau P, Rattner D (2014) Laparoscopic Heller myotomy as the gold standard for treatment of achalasia. J Gastrointest Surg 18:2201–2207
Spiess AE, Kahrilas PJ (1998) Treating achalasia: from whalebone to laparoscope. JAMA 280:638–642
Jeansonne LO, White BC, Pilger KE, Shane MD, Zagorski S, Davis SS, Hunter JG, Lin E, Smith CD (2007) Ten-year follow-up of laparoscopic Heller myotomy for achalasia shows durability. Surg Endosc 21:1498–1502
Bessell JR, Lally CJ, Schloithe A, Jamieson GG, Devitt PG, Watson DI (2006) Laparoscopic cardiomyotomy for achalasia: long-term outcomes. ANZ J Surg 76:558–562
Adler DG, Romero Y (2001) Primary esophageal motility disorders. Mayo Clin Proc 76:195–200
Pereira PF, Rosa AR, Mesquita LA, Anzolch MJ, Branchi RN, Giongo AL, Paixao FC, Chedid MF, Kruel CD (2019) Esophagogastric junction outflow obstruction successfully treated with laparoscopic Heller myotomy and Dor fundoplication: first case report in the literature. World J Gastrointest Surg 11:112–116
Leconte M, Douard R, Gaudric M, Dumontier I, Chaussade S, Dousset B (2007) Functional results after extended myotomy for diffuse oesophageal spasm. Br J Surg 94:1113–1118
Oresanya LB, Lyons WL, Finlayson E (2014) Preoperative assessment of the older patient: a narrative review. JAMA 311:2110–2120
Watt J, Tricco AC, Talbot-Hamon C, Pham B, Rios P, Grudniewicz A, Wong C, Sinclair D, Straus SE (2018) Identifying older adults at risk of harm following elective surgery: a systematic review and meta-analysis. BMC Med 16:2
Farquharson SM, Gupta R, Heald RJ, Moran BJ (2001) Surgical decisions in the elderly: the importance of biological age. J R Soc Med 94:232–235
Patel DA, Lappas BM, Vaezi MF (2017) An overview of achalasia and its subtypes. Gastroenterol Hepatol (N Y) 13:411–421
Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A, Costantino M, Nicoletti L, Ancona E (2002) Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg 235:186–192
Costantini M, Zaninotto G, Guirroli E, Rizzetto C, Portale G, Ruol A, Nicoletti L, Ancona E (2005) The laparoscopic Heller-Dor operation remains an effective treatment for esophageal achalasia at a minimum 6-year follow-up. Surg Endosc 19:345–351
Kostic S, Kjellin A, Ruth M, Lonroth H, Johnsson E, Andersson M, Lundell L (2007) Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg 31:470–478
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39:713–720
Weber CE, Davis CS, Kramer HJ, Gibbs JT, Robles L, Fisichella PM (2012) Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutan Tech 22:289–296
Schuchert MJ, Luketich JD, Landreneau RJ, Kilic A, Gooding WE, Alvelo-Rivera M, Christie NA, Gilbert S, Pennathur A (2008) Minimally-invasive esophagomyotomy in 200 consecutive patients: factors influencing postoperative outcomes. Ann Thorac Surg 85:1729–1734
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanstrom LL (2005) Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg 140:827–833 (discussion 833–824)
Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, Luketich JD (2009) Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery 146:826–831 (discussion 831–823)
Acknowledgements
We acknowledge the biostatistical consultation and support from the biostatical consultation and support from the Biostatistical Consulting Core at the School of Medicine, Stony Brook University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Aurora Pryor is a speaker for Gore and Merck and she participates on a scientific advisory board for Obalon. Dr. Konstantinos Spaniolas has research support from Merck and a speaker for Gore. Dr. Andrew Brown, Dr. Jie Yang, Ms. Xiaoyue Zhang, Dr. Maria Altieri, and Dr. Kelly Ieong have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ieong, K., Brown, A., Yang, J. et al. The incidence of reintervention and reoperation following Heller myotomy across multiple indications. Surg Endosc 36, 1619–1626 (2022). https://doi.org/10.1007/s00464-021-08357-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08357-6