Abstract
Background
The double-tract reconstruction (DTR) could be a preferable option in avoiding the postoperative esophageal reflux and anastomotic stenosis during totally laparoscopic proximal gastrectomy (TLPG). An optimal procedure to achieve the DTR in TLPG remains to be established.
Methods
During March 2018 to April 2019, 15 consecutive patients with gastric cancer in the upper third of the stomach underwent intracorporeal DTR after TLPG at our hospital. The intracorporeal esophagojejunostomy (E-J), gastrojejunostomy (G-J) and jejunojejunostomy (J-J) were, respectively, performed using circular staplers by the Self-Pulling and Holding Purse-String Suture Technique, Intraluminal Poke Technique and U-shaped Parallel Purse-string Suture Technique (Technical Tie-Up). Demographic and clinicopathologic characteristics, perioperative details and postoperative outcomes were analyzed.
Results
The mean operating time was 216.1 ± 18.2 min. Total time for three anastomoses was 49.8 ± 6.1 min, and the time for E-J, G-J, J-J was 22.4 ± 5.0 min, 13 (range 11–16) min, 14.2 ± 2.8 min, respectively. The median proximal and distal resection margins were 2.5 (range 2–4) cm and 6 (range 5–7) cm, respectively, which were all tumor-free in 15 patients. No major complications and mortality occurred. During the median follow-up period of 14 months (range 7 to 20.5 months), there were no postoperative anastomosis-related complications observed, such as anastomotic bleeding, leakage or stenosis. No patients complained the symptoms indicating esophageal reflux and remnant gastritis.
Conclusions
Predominant classic circular-stapled double-tract reconstruction is safe, feasible and time-saving in TLPG by the technical tie-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The incidence of cancer in the upper third of the stomach has been steadily increasing over the last half century [1, 2]. For these cases of proximal gastric cancer, both laparoscopic total gastrectomy (LTG) and laparoscopic proximal gastrectomy (LPG) are the current surgical approaches, while the LPG provides a series of advantages such as more food intake volume and better postoperative nutrition status [3, 4].
As for the digestive reconstruction after LPG, the double-tract reconstruction (DTR) could be a preferable option considering its more priority in avoiding the postoperative esophageal reflux and anastomotic stenosis than esophagogastrostomy (EG) [5,6,7,8]. Some studies suggested the incidences of reflux esophagitis for EG and DTR were (range 9.1–35.3%) vs (range 0–25%) [7, 8]. However, the completion of intracorporeal DTR with three anastomoses in totally laparoscopic proximal gastrectomy (TLPG) is apparently difficult for its quite time-consuming and technically demanding procedure. The wide applications of linear staplers or hand-sewing manners would face huge challenges due to their own inherent disadvantages and limitations, such as the closure of the irregular or large common openings and the higher requirement for laparoscopic suture skill, although several recent studies reported the procedures of DTR in TLPG using the both [9,10,11,12]. Therefore, an optimal technique to achieve the DTR in TLPG remains to be established.
Herein, we introduce the safe, feasible and time-saving integrated procedures to intracorporeally achieve the three anastomoses of DTR in TLPG using only circular staplers. In this study, we, respectively, performed the intracorporeal esophagojejunostomy (E-J), gastrojejunostomy (G-J) and jejunojejunostomy (J-J) using circular staplers within a mean of 49.8 ± 6.1 min by the Self-Pulling and Holding Purse-String Suture Technique, Intraluminal Poke Technique and U-shaped Parallel Purse-string Suture Technique (technical tie-up), which all were previously reported by our team [13,14,15]. The technical tie-up could create the complete three circular-stapled anastomoses and produce more comfort to surgeons because of its safety and time-saving instead of tiredness or fear of anastomotic leakage and stenosis than using others. To the best of our knowledge, this is the first report that all the three anastomoses of DTR in TLPG were completed by the pure classic circular-stapled approaches with their own obvious advantages. The surgical process and preliminary outcomes are shown in the present study.
Methods
Patients and techniques
In our study, 15 consecutive patients with gastric cancer in the upper third of the stomach underwent intracorporeal DTR after TLPG from March 2018 to April 2019 at our hospital. The intracorporeal E-J, G-J and J-J anastomosis of the DTR were all achieved with the circular-stapled manners in all patients. Patients selection criteria included (1) histologically confirmed gastric adenocarcinoma, and lesion invasion within submucosal layer with no suspected positive LN and no distant metastasis by preoperative endoscopy, endoscopic ultrasonography and computed tomography; (2) tumor located in the upper third of the stomach with tumor diameter no larger than 4 cm; (3) no contraindication for laparoscopic surgery. The type of operation was selected based on the patient’s individual decision after being informed of the advantages and disadvantages of each method, and the written informed consent was obtained from all patients.
Operative procedures
Patients were placed in the supine position with the two legs split under general anesthesia. Pneumoperitoneum was established at about 10–12 mmHg, and five percutaneous ports were placed on the umbilicus and the bilateral upper abdominal regions (Fig. 1). Subsequently, abdominal cavity exploration, D1+ lymphadenectomy (the dissections of No.1, No.2, No.3a, No.4sa, No.4sb, No.7, No.8a, No.9, and No.11p) based on the Japanese guidelines for proximal gastric cancer were carried out under laparoscopy [16]. A 2.5 cm abdominal incision on the left middle clavicular line was made for putting into anvils, specimen extraction and circular staplers introduction (Fig. 1). Two 25 mm anvils (DST Series, EEA; Medtronic, Minneapolis, MN) secured with a 2-0 suture loop of approximately 3–5 cm (Braided Nylon, Surgilon; Medtronic Minneapolis, MN) at its central rod, were pushed into the abdominal cavity through the abdominal incision for their following placement at the esophagus and stomach after the stomach was fully divided.
Trocar placement for TLPG with double-tract reconstruction. (A) Camera port for laparoscopy; (B) main manipulation port for the surgeon; (C–E) assisted ports; (F) abdominal incision approximately 2.5 cm on the left middle clavicular line for the specimen extraction, putting into anvil and circular stapler introduction
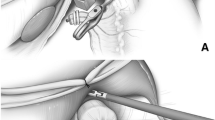
For double-tract reconstruction, G-J and E-J were first performed, respectively. At first, the distal esophageal wall was sub-totally transected in approximately 90% circumference from the left side using the electrocautery, remaining approximately 10% circumference uncut at the right side. Using the Self-pulling and Holding Purse-String Suture Technique [15], the laparoscopic hand-sewn purse-string suture and anvil placement were completed (Fig. 2A). Next, using the Intraluminal Poke Technique (Fig. 2B) [14], the other 25 mm anvil secured with a suture loop was introduced into the stomach through an anterior gastrotomy approximately 2.5 cm on the middle-upper stomach. The laparoscopic needle holder which carried the suture loop and anvil was advanced to the tentative anastomosis position of the greater curvature of approximately 1/2 stomach, and pushed out by its head to generate a small opening for pulling out the central rod of the anvil after electrocautery was applied at the protruding gastric wall. Approximately half stomach was divided using another one following the cutting of one endoscopic linear stapler (Endo-GIA; Medtronic, Minneapolis, MN) close to the root of the suture loop attached to the anvil and pulling out the central rod of the anvil. The specimen was extracted by one plastic protection bag through the abdominal incision. The jejunum was divided about 25 cm distal to the Treitz ligament. A 25 mm circular stapler was put into the abdominal cavity through the abdominal incision. The circular stapler lubricated by paraffin oil was inserted into jejunum through the jejunal end with the traction of three graspers from the assistant and surgeon (left hand), and then pushed it to the tentative anastomosis position in forward direction by against count pressure of one grasper that the surgeon applied on the jejunum and the two graspers from the assistant. The constant opposite traction was applied on the jejunal end by the left hand of surgeon to properly keep the jejunum on the circular stapler from slipping off without the fixation. Subsequently, the central rod of the circular stapler was pierced out the jejunal wall to connect with anvil at the distal half stomach (Fig. 2C). The G-J anastomosis was completed in an anti-colic manner after the circular stapler was fired. Afterward, another 25 mm circular stapler was inserted into the distal jejunal lumen about 5 cm from the distal jejunal for the formation of E-J (Fig. 2D). An end-to-side E-J anastomosis was obtained after the shaft of the circular stapler was coupled with the anvil along the proximal esophageal stump and fired. The distal limb of the jejunal stumps was closed by an endoscopic linear stapler. Finally, the last 25 mm anvil secured with a 2-0 suture loop was pushed into abdomen through the abdominal incision for the creation of J-J as the last anastomosis of DTR in TLPG. The purse-string suture was placed along the distal intestine approximately 20 cm distal to the G-J anastomosis by four forehand seromuscular stitches of two unidirectional parallel suturing along the jejunum using the U-shaped Parallel Purse-String Suture Technique (Fig. 2E) [13], and then the 25 mm anvil was placed in position at the intestine segment. A 25 mm circular stapler was inserted into the proximal jejunal lumen about 5 cm, then a completed side-to-side J-J was created after coupling and firing of the circular stapler (Fig. 2F). The proximal jejunal end was closed using an endoscopic linear stapler, and the mesenteric defect was closed by laparoscopic hand-sewn manner. Afterward, the complete DTR after TLPG was formed (Fig. 3).
Schematic illustration of the Technical Tie-Up. A The purse-string suture at the esophagus stump is completed for the anvil placement using the Self-Pulling and Holding Purse-String Suture Technique. T, tumor. B Anvil placement at the great curvature of approximately 1/2 stomach using the Intraluminal Poke Technique. The laparoscopic needle holder holding the suture loop secured at the central rod of the anvil is poked out and the electrocautery is applied at the protruding gastric wall to generate a small opening. T tumor. C Schematic illustration of the circular-stapled gastrojejunostomy. The 25 mm circular stapler is put into the distal jejunal lumen about 20 cm from the distal jejunal end for being coupled with the anvil at stomach. D Schematic illustration of the circular-stapled esophagojejunostomy. The 25 mm circular stapler is inserted into the distal jejunal lumen about 5 cm from the distal jejunal end to be connected to the anvil along the esophageal stump. E The purse-string suture at the jejunum is completed for the anvil placement using the U-Shaped Parallel Purse-String Suture Technique. F Schematic illustration of circular-stapled jejunojejunostomy. The 25 mm circular stapler is inserted into 5 cm of the proximal jejunal lumen to be coupled with the anvil along the distal jejunum
Postoperative management
For all patients, a water-soluble contrast media study was applied for evaluations of anastomoses on postoperative day 3. After their first bowel movement, 15 patients were given liquid diet, and soft diet was given if there’s no any anastomosis-related complication observed. All these patients were uneventfully discharged with a median of 7 (range 6–10) days after operation.
Results
Patient clinicopathological characteristics and operative results are shown in Table 1. The mean operating time was 216.1 ± 18.2 min. Total time for three anastomoses was 49.8 ± 6.1 min, and the time for E-J, G-J, J-J was 22.4 ± 5.0 min, 13 (range 11–16) min, 14.2 ± 2.8 min, respectively (the time for each of esophagojejunostomy and jejunojejunostomy was the total required time of the purse-string suture, anvil placement, the coupling with the anvil and firing of the circular stapler. The time for gastrojejunostomy was the total required time of the Intraluminal Poke procedure, the coupling and firing of the circular stapler). The average estimated blood loss was 177.3 ± 78.4 mL. The median proximal and distal resection margins were 2.5 (range 2–4) cm and 6 (range 5–7) cm from the tumor, which were all tumor-free in 15 patients. No patients underwent conversion to other intracorporeal anastomosis techniques or open surgery. There were 4 postoperative complications and morbidities including atelectasis (n = 2), pleural effusion (n = 1), and pulmonary infection (n = 1). All the four patients recovered after conservative treatment. No surgical site infection occurred. There was no mortality. During the median follow-up period of 14 months (range 7 to 20.5 months), there were no instances of postoperative anastomosis-related complications, such as anastomotic bleeding, leakage or stenosis. No patients complained the symptoms indicating esophageal reflux and remnant gastritis. There were no any sign of reflux esophagitis and remnant gastritis for five patients underwent an endoscopic evaluation after surgery.
Discussion
In this article, we have described the technical tie-up (Self-Pulling and Holding Purse-String Suture Technique, Intraluminal Poke Technique, U-shaped Parallel Purse-String Suture Technique) for intracorporeal DTR in TLPG, during which the E-J, G-J and J-J of the DTR were all completed with pure circular staplers. Within our 15 cases in this study, the total time for the three anastomoses was 49.8 ± 6.1 min, and the time for E-J, G-J, J-J was 22.4 ± 5.0 min, 13 (range 11–16) min, 14.2 ± 2.8 min, respectively, and no anastomosis-related complications occurred. The technical tie-up could be safe, feasible and time-saving, and provided reasonable complication incidence and satisfactory outcomes.
Since the first performance in 1995 [17], the LPG has been increasingly performed for gastric cancer cases located at the upper third portion of stomach. In fact, TLPG has been being considered to be less invasive and more function-preserving than LPG or totally laparoscopic total gastrectomy (TLTG) since the physiological function of the distal part of the stomach is preserved to reduce postoperative weight loss or decrease the incidence of gastric symptoms and nutritional deficiencies [3, 18, 19]. Given the great priority in avoiding the incidence of esophageal reflux and anastomotic stenosis [5, 20], the DTR could be a better choice in TLPG.
Currently, to achieve the DTR in TLPG, various techniques such as linear-stapled and laparoscopic hand-sewn techniques have been proposed. As for the linear-stapled techniques, they still present some deficiencies of their own [9, 10, 20]. On one hand, no matter of the E-J, G-J or J-J, the common incision was unavoidable if the linear stapler was applied, and sometimes it may be skill-demanding and time-consuming to close an irregular or a large common incision adequately by linear- stapled or hand-sewn manner. On the other hand, the linear-stapled procedure always necessitates sufficient length of esophagus, and the E-J would be created in chest cavity or mediastinum where the negative intrathoracic pressure may increase esophageal reflux; even more, it would be more troublesome and dangerous once there's anastomotic leakage in the mediastinum. Some surgeons also tried applying laparoscopic hand-sewn techniques to perform some anastomoses of DTR in TLPG. As one of the most conventional laparoscopic surgical technique, the laparoscopic hand-sewn technique has some advantages like saving the cost of the surgery and making the operation not restricted by the available surgical instruments [21]. However, even for the surgeons with advanced laparoscopic suturing skill, it should not be the first choice to finish the three anastomoses of DTR in TLPG by laparoscopic hand-sewn manner because of the long operation time. Furthermore, although circular-stapled anastomosis is the popular and time-tested procedure to accomplish digestive reconstruction in conventional open gastrectomy, it has been never reported that all the intracorporeal E-J, G-J and J-J of the DTR were performed using circular staplers during TLPG. It may attribute to the difficulties of the performance of intracorporeal purse-string suture and anvil placement along esophagus, stomach and intestine under laparoscopy. Therefore, the safe, feasible and time-saving procedures of intracorporeal purse-string suture and anvil placement along these organs can be crucial to apply the classic circular stapler to the DTR during TLPG.
To address the problems, we introduced the integrated applications of our reported three unique techniques (the technical tie-up) in predominant circular-stapled anastomoses of DTR in TLPG. During this approach, three anvil placements along esophagus, stomach and intestine were successively obtained by the Self-Pulling and Holding Purse-String Suture Technique, Intraluminal Poke Technique and U-shaped Parallel Purse-String Suture Technique. As a result, the E-J, G-J and J-J of DTR in TLPG were created in safety, feasibility and time-saving using pure circular staplers.
These procedures are of many advantages in the following several aspects. First, it is the first report about performing all the three anastomoses of the DTR in TLPG using the pure classic circular-stapled anastomoses as open surgery. Second, it is the integrated and ingenious applications of the three unique techniques concerning predominant circular-stapled anastomoses during TLPG to make sufficient use of their advantages, such as the prevention of esophageal shortening or retracting into the mediastinum and great mobility, free purse-string suture at stomach and the simplest paralleled purse-string suture along intestine in safety and time-saving. Third, the three classic circular-stapled anastomoses were completely and finally formed without any opening left after each coupling and firing of circular stapler, which is so familiar to our surgeons. Fourth, the time-saving procedures with the complete three circular-stapled anastomoses by the technical tie-up would produce more comfort to the surgeons instead of tiredness or fear of anastomotic leakage and stenosis using others, which is different from the comfort of patients who underwent totally laparoscopic gastrectomy because of the smaller incision, less pain, and earlier ambulation, etc. Fifth, the classic circular-stapled E-J could especially lower the height of anastomosis or decrease the risk of fatal anastomotic leakage in mediastinum than linear-stapled E-J of DTR in TLPG. Sixth, the procedures could drive the DTR in TLPG wider application for patients with gastric cancer in the upper third of the stomach by surgeons with basic laparoscopic skills because of these own merits.
However, the surgical limitation using the procedure is the proximal gastric cancer with invasion to the intra-abdominal esophagus of no more than 1 cm. Moreover, some limitations of our study are the amount of the small cases and no comparative data with other intracorporeal double-tract reconstruction methods. Therefore, it is further required for long-term follow-up data to confirm the long-term nutritional, functional and oncological outcomes, and comparative studies with other intracorporeal anastomosing methods to assess which is better among them.
Conclusions
In conclusion, our results suggest that the predominant classic circular-stapled double-tract reconstruction after TLPG is safe, feasible, time-saving by the technical tie-up.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Colquhoun A, Arnold M, Ferlay J, Goodman KJ, Forman D, Soerjomataram I (2015) Global patterns of cardia and non-cardia gastric cancer incidence in 2012. Gut 64:1881–1888
Mazer LM, Poultsides GA (2019) What is the best operation for proximal gastric cancer and distal esophageal cancer? Surg Clin N Am 99:457–469
Jung DH, Ahn SH, Park DJ, Kim HH (2015) Proximal gastrectomy for gastric gancer. J Gastric Cancer 15:77–86
Ichikawa D, Komatsu S, Okamoto K, Shiozaki A, Fujiwara H, Otsuji E (2013) Evaluation of symptoms related to reflux esophagitis in patients with esophagogastrostomy after proximal gastrectomy. Langenbecks Arch Surg 398:697–701
Jung DH, Lee Y, Kim DW, Park YS, Ahn SH, Park DJ, Kim HH (2017) Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg Endosc 31:3961–3969
Wang SQ, Lin S, Wang H, Yang JJ, Yu PF, Zhao QC, Li MB (2018) Reconstruction methods after radical proximal gastrectomy: a systematic review. Medicine 90(11):1–7
Nakamura M, Yamaue H (2016) Reconstruction after proximal gastrectomy for gastric cancer in the upper third of the stomach: a review of the literature published from 2000 to 2014. Surg Today 46:517–527
Hong J, Qian L, Wang YP, Wang J, Hua LC, Hao HK (2016) A novel method of delta-shaped intracorporeal double-tract reconstruction in totally laparoscopic proximal gastrectomy. Surg Endosc 30:2396–2403
Yang K, Bang HJ, Almadani ME, Dy-Abalajon DM, Kim YN, Roh KH, Lim SH, Son T, Kim HI, Noh SH, Hyung WJ (2016) Laparoscopic proximal gastrectomy with double-tract reconstruction by intracorporeal anastomosis with linear staplers. J Am Coll Surg 222:E39–E45
Aburatani T, Kojima K, Otsuki S, Murase H, Okuno K, Gokita K, Tomii C, Tanioka T, Inokuchi M (2017) Double-tract reconstruction after laparoscopic proximal gastrectomy using detachable ENDO-PSD. Surg Endosc 31:4848–4856
Lee CM, Park DW, Jung DH, Jang YJ, Kim JH, Park S, Park SH (2016) Single-port laparoscopic proximal gastrectomy with double tract reconstruction for early gastric cancer: report of a case. J Gastric Cancer 16:200–206
Du JJ, Xue HY, Zhao LZ, Hua J, Hu J, Zhang ZQ (2019) Intracorporeal circular-stapled anastomosis after totally laparoscopic gastrectomy: a novel, simplest u-shaped parallel purse-string suture technique. J Surg Oncol 120:501–507
Du JJ, Xue HY, Hua J, Zhao LZ, Zhang ZQ (2019) Intracorporeal classic circular-stapled gastrojejunostomy and jejunojejunostomy during laparoscopic distal gastrectomy: a simple, safe “intraluminal poke technique” for anvil placement. J Surg Oncol 119:464–471
Du JJ, Shuang JB, Li J, Li JP, Hua J (2014) Intracorporeal circular-stapled esophagojejunostomy after laparoscopic total gastrectomy: a novel self-pulling and holding purse-string suture technique. J Am Coll Surg 218:E67–E72
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20:1–19
Uyama I, Ogiwara H, Takahara T, Kikuchi K, Iida S (1995) Laparoscopic and minilaparotomy proximal gastrectomy and esophagogastrostomy: technique and case report. Surg Laparosc Endosc 5:487–491
Ueda Y, Shiroshita H, Etoh T, Inomata M, Shiraishi N (2017) Laparoscopic proximal gastrectomy for early gastric cancer. Surg Today 47:538–547
Kukar M, Gabriel E, Ben-David K, Hochwald SN (2018) Laparoscopic proximal gastrectomy for gastric neoplasms. J Surg Oncol 118:95–100
Ahn SH, Jung DH, Son SY, Lee CM, Park DJ, Kim HH (2014) Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer 17:562–570
So KO, Park J (2011) Totally laparoscopic total gastrectomy using intracorporeally hand-sewn esophagojejunostomy. J Gastric Cancer 11:206–211
Acknowledgments
We thank Jin Hua for her statistical analysis of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Jian Hu, Lizhi Zhao, Hongyuan Xue, Ziqiang Zhang and Jianjun Du have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, J., Zhao, L., Xue, H. et al. Predominant classic circular-stapled double-tract reconstruction after totally laparoscopic proximal gastrectomy: safe, feasible, time-saving anastomoses by technical tie-up. Surg Endosc 34, 5181–5187 (2020). https://doi.org/10.1007/s00464-020-07824-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07824-w