Abstract
Background
Incisional hernia (IH) is a common complication after colorectal surgery. However, the risk factors for incisional hernia after laparoscopic colorectal surgery (LCRS) have not been fully elucidated. This retrospective study analyzed the incidence rate of IH and evaluated the risk factors for IH after LCRS.
Methods
This was a retrospective multi-institution study of 423 colorectal cancer patients conducted between September 2012 and December 2014 in Yokohama Clinical Oncology Group. The diagnosis of IH was based on computed tomography and physical examination findings. The patient-, tumor-, and surgery-related variables were examined by univariate and multivariate analyses.
Results
A total of 423 patients were analyzed. The median follow-up period was 48.4 months. IH was observed in 36 patients (8.5%). The 1-year incidence of IH was 5.2%, and the 4-year incidence was 8.5%. A multivariate analysis showed that preoperative umbilical hernia (odds ratio [OR] 5.71; 95% confidence interval [CI] 2.02–16.10; p = 0.001) and a visceral fat area (VFA) ≥ 100 cm2 (OR 2.74; 95% CI 1.08–6.96; p = 0.035) were independent risk factors of IH after LCRS.
Conclusions
The risk factors of IH after LCRS were preoperative umbilical hernia and VFA ≥ 100 cm2. In the case with an umbilical hernia or VFA ≥ 100 performing LCRS, it should likely NOT have a peri-umbilical extraction site and should be considered for an alternate site like a low transverse or Pfannenstiel incision.
Clinical Trials Registration: The trial was registered with the UMIN Clinical Trials Registry, number 000038707.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Incisional hernia (IH) is one of the most common complications following abdominal surgery. IH is often asymptomatic and rarely causes occlusion and strangulation; however, more than one-third of patients have symptoms of pain or discomfort at the hernia site and suffer limitations of activity, resulting in a poor quality of life.
There have been some reports regarding the risk factors of IH after open surgery for colorectal cancer [1,2,3,4]. Patient factors, such as obesity, sex, and age; surgical factors, such as suture technique, wound infection, and wound length; and biological factors, such as smoking habit and defects of collagen and enzymes, have been reported as risk factors for IH.
Laparoscopic surgery is an accepted treatment modality for colon cancer, and laparoscopic surgery for colon cancer has become a viable alternative strategy to open surgery [5,6,7,8,9]. However, few studies have explored the risk factors for IH after laparoscopic colorectal surgery (LCRS). Thus far, the gender, body mass index (BMI), presence of surgical site infection (SSI) after surgery, visceral fat obesity and specimen extraction site have been reported as risk factors of IH after limiting LCRS [10,11,12,13,14,15,16].
It was recently reported that the visceral fat volume was a risk factor for IH after colorectal surgery [11, 17]. Although the BMI is a useful indicator of obesity, it does not always reflect the degree of obesity in the visceral cavity, as the distribution of adipose tissue differs markedly among individuals. We previously found that visceral obesity was a superior predictive factor for an increased risk of postoperative complications after laparoscopic colectomy compared with the BMI [18].
The present study analyzed the incidence rate of IH and evaluated the risk factors for IH after LCRS.
Materials and methods
The study protocol was approved by the Ethical Advisory Committee of Yokohama City University Graduate School of Medicine and the institutional review board of each participating hospital before the study was initiated. The study was registered with the Japanese Clinical Trials Registry as UMIN000038707 (https://www.umin.ac.jp/ctr/index.htm). Due to the retrospective nature of the study, written informed consent was not obtained. We used opt-out to disclose the study information.
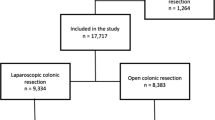
From September 2012 to December 2014, 566 consecutive patients with a preoperative diagnosis of colon or rectal cancer underwent LCRS with lymph node dissection at 2 institutions of Yokohama City University Medical Center and Yokohama City University Graduate School of Medicine in Yokohama Clinical Oncology Group. Of these, 423 patients were retrospectively investigated. The exclusion criteria of this study were cases with emergency surgery, conversion to open surgery, abdominoperineal resection, intersphincteric resection wherein the specimen was extracted via a perineal wound or the anus, other abdominal operations during the follow-up period, and missing data concerning the preoperative visceral fat area (VFA).
The following data were collected: age, sex, BMI, American Society of Anesthesiologists score (ASA), Eastern Cooperative Oncology Group performance status (ECOG PS), Prognostic Nutritional Index (PNI), smoking history, comorbid diseases (e.g., hypertension, diabetes mellitus, cardiac disease), history of preoperative umbilical hernia, VFA, subcutaneous fat area (SFA), location of primary tumor, preoperative TNM stage according to the 7th edition of the Union for International Cancer Control classification, neoadjuvant treatment including chemo and/or radiation therapy, preoperative bowel preparation, operation time, intraoperative amount of blood loss, length of umbilical incision, intraoperative blood transfusions, intraoperative hypotension requiring use of pressor and postoperative complications over grade I according to the Clavien–Dindo classification, such as SSI, anastomotic leakage, and small bowel obstruction.
The BMI, VFA, and SFA in particular were analyzed as primary measurements of obesity to compare the incidence rate of IH of the groups with and without IH. The VFA and SFA were measured by importing cross-sectional CT imaging data into the SYNAPSE VINCENT system (FUJIFILM, Tokyo, Japan) at the level of umbilicus by independent medical staff preoperatively. In Japan, the BMI cut-off value defining obese and non-obese is 25 kg/m2, and the VFA cut-off value defining obese and non-obese is 100 cm2 by the Japan Society for the Study of Obesity [19, 20]. However, there is no standardized established cut-off value for SFA, so receiver operating characteristic (ROC) curves were constructed to compare these measurements with IH as the classifier. A cut-off value of 150 cm2 was calculated by the ROC curve.
Procedure
Total six surgeons participated in this study. LCRS was performed using five ports: a 12-mm port in the umbilical region; three 5-mm ports in the upper-right, upper-left, and lower-left quadrants; and a 12-mm port in the lower-right quadrant. A 12-mm umbilical trocar was used as a camera port for a rigid scope.
In both arms, the skin incision was performed with a scalpel, and the subcutaneous fat and linea alba were dissected by electrical cautery. Central vascular ligation and colon or rectum mobilization were performed laparoscopically. The specimen was extracted through the umbilical port, which was extended according to the size of the specimen. During specimen extraction, wound protection was achieved using a dual-ring drape device. Wound closure of the umbilical incision was done with interrupted sutures using 1-Vicryl® for the fascia layer and 4–0 PDS® subcuticular sutures for the skin. Prophylactic intraoperative wound irrigation with 1000 ml of saline was routinely performed before skin closure. The prophylactic antibiotic regimens were performed as follows: flomoxef sodium was injected intravenously within 30 min before the skin incision. In patients who underwent operations lasting longer than 3 h, flomoxef sodium was injected intravenously every 3 h.
The diagnosis of IH
The incidence of incisional hernia was monitored for more than 3 years after the operation. After hospital discharge, patients were followed at the hospital as an outpatient every 3 months by a physical examination and every 6 months by computed tomography (CT). The diagnosis of IH was based on physical examination or CT findings (Fig. 1). IH was diagnosed based on the discontinuity of the abdominal fascia at the umbilical surgical site. Parastomal hernia and port site hernia were not included in this study. The duration until the detection of IH was calculated from the date of surgery to the earliest date of IH presence on CT.
Statistical analyses
All statistical analyses were performed with the JMP® 12 software program (SAS Institute Inc., Cary, NC, USA). Quantitative data are expressed as the median and range. Comparisons between two groups were made using the Mann–Whitney U test, χ2 test, and Fisher’s exact test, and p-values of less than 0.05 were considered statistically significant. The patient survival analysis was preformed using Kaplan–Meier survival curves with log-rank statistics. Variables with p-values of less than 0.05 in the univariate analysis were included in the multivariate analysis. The multivariate analysis was performed using the Cox proportional hazards methods. The results of the Cox model analysis were reported using odds ratios (ORs) and 95% confidence intervals (CIs). Kaplan–Meier curves were used to study the time to the development of IH and were stratified by the surgical approach.
Results
The incidence of IH in the study population is shown in Fig. 2. The median follow-up period was 48.4 months, and the incidence was 5.2% at 12 months, 7.8% at 24 months, 8.0% at 36 months, and 8.5% at 48 months (Fig. 2). In this study, among the patients who had IH, about 90% of cases occurred within 2 years. And how to detect postoperative IH were almost surveillance CT (97%) (Table 1).
The characteristics of the groups with and without IH are shown in Table 1. A total of 423 patients underwent laparoscopic colorectal surgery. There were no significant differences in the age, sex, ASA, ECOG PS, PNI, smoking history, presence of co-morbid disease, tumor location whether colon or rectum, primary tumor stage, neoadjuvant treatment, preoperative bowel preparation, operation time, intraoperative amount of blood loss, intraoperative blood transfusions, intraoperative hypotension requiring use of pressor, incision length at umbilical site, or postoperative complication rate between the groups. However, the BMI in the IH group was significantly higher than in the no-IH group (IH 24.8 vs. no-IH 22.4, p < 0.001). Furthermore, the rate of having preoperative umbilical hernia in the IH group was higher than in the no-IH group (IH 22.2% vs. no-IH 3.1%, p < 0.001), the VFA in the IH group was larger than in the no-IH group (IH 140 cm2 vs. 98.2 cm2, p < 0.001), and the SFA in the IH group was also larger than in the no-IH group (TC 163.1 cm2 vs. no-IH 112.2 cm2, p < 0.001).
The results of a univariate analysis of the groups with and without IH are shown in Table 2. The rate of BMI ≥ 25 in the IH group was significantly higher than in the no-IH group (p = 0.002). And the rate of BMI ≥ 30 in the IH group was also significantly higher than in the no-IH group (p = 0.006). Furthermore, the rate of a preoperative umbilical hernia was higher in the IH group than in the no-IH group (p < 0.001), the rate of VFA ≥ 100 cm2 and SFA ≥ 150 cm2 was higher in the IH group than in the no-IH group (p < 0.001 and p = 0.002, respectively), and the rate of the incision length at the umbilical site ≥ 60 mm was higher in the IH group than in the no-IH group (p = 0.034).
A multivariate analysis using the BMI cut-off of 25 showed that preoperative umbilical hernia (OR 5.71; 95% CI 2.02–16.10; p = 0.001) and VFA ≥ 100 cm2 (OR 2.74; 95% CI 1.08–6.96; p = 0.035) were independent risk factors of IH after LCRS (Table 3). And in multivariate analysis using the BMI cut-off of 30, the independent risk factors of IH were preoperative umbilical hernia (OR 5.00; 95% CI 2.05–10.9; p = 0.001) and VFA ≥ 100 cm2 (OR 2.62; 95% CI 1.13–6.81; p = 0.023) (Table 4).
Discussion
The incidence rate after LCRS was previously reported to range from 3.4 to 17.0% [10, 11, 13, 15, 21,22,23,24,25,26]. Most previous studies were retrospective in nature, like the present study, and our rate of IH was similar to that in those previous studies. In addition, almost all cases of IH occurred within 2 years in this study, Yamamoto et al. reported a similar cumulative incidence rate curve for IH [11]. A nationwide cohort study in Denmark also reported that IH after LCRS was observed early during follow-up [23].
The risk factors of developing IH can be divided into two categories: patient-related and operation-related. Regarding patient-related risk factors, previous reports have mentioned obesity—e.g., high values for the BMI, SFA, and VFA—as well as male gender and older age as risk factors for IH [11, 13, 15,16,17, 21, 23, 27, 28]. Among these values, the BMI has been used to reflect obesity because it is easy to measure. However, the BMI does not reflect true body fat, as a high BMI indicates not only visceral fat obesity but also subcutaneous fat obesity. Other measurements of obesity include the waist circumference, SFA, VFA, and total fat area (i.e., the sub of the SFA and VFA), although few reports have mentioned these factors as risk factors for developing IH. In this study, the VFA was independent risk factor of IH but the SFA and BMI were not independent risk factors in the multivariate analysis. The BMI cut-off was lower than that of U.S. and western countries, this may be one reason why the BMI was not associated with increased risk factor for IH in the multivariable analysis. Christopher et al. and Yamamoto et al. showed that visceral obesity was a strongly significant risk factor for IH after colorectal surgery [11, 17], but only one report analyzed the VFA as a risk factor for IH after LCRS. The association between obesity and IH has been attributed to increased abdominal wall tension [29], and A meta-analysis reported that VFA of Japanese obesity was larger than other countries [30], so VFA may be a better factor reflecting the intraabdominal pressure than other factors. Our results indicated that a high degree of visceral fat obesity is strongly associated with the development of IH. However, the cut-off value of VFA has not been standardized, so further studies are needed.
Operation-related risk factors include SSI, length of incision, and location of specimen extraction. In our report, SSI was not a significant risk factor associated with developing IH; however, some reports have described an association between SSI and IH [23, 31]. Our study included only cases of laparoscopic surgery, so the length of the incision was shorter than that with open surgery, and the SSI rate was relatively lower than in previous reports. Yamamoto et al., whose data included only laparoscopic surgery, just like this study, also did not find SSI to be a significant risk factor of IH.
The rate of an incision length over 60 mm was significantly greater in the IH group than in the no-IH group according to a univariate analysis; however, this factor was not found to be an independent risk factor for developing IH according to the multivariate analysis. Davit et al. reported that an incision length over 5 cm was a significant independent risk factor for developing IH [13]. The extraction incision site in this report included not only the midline site but also other sites, in contrast to that previous study. An open technique for colorectal surgery was reported to be a risk factor for IH compared to a laparoscopic technique [24]. Further studies are needed to determine the cut-off value for the incision length.
The extraction site is another important risk factor for IH. However, all cases in the present study used a midline incision to extract the specimen, and a randomized trial in patients after LCRS showed that a transverse specimen extraction incision had a lower incidence of IH than midline specimen extraction incision (but worse cosmesis) [12]. Another large-scale retrospective cohort study concerning LCRS showed that a Pfannenstiel incision was the best extraction site in terms of reducing the risk of IH and that midline incisions should be avoided when possible [32].
For further consideration regarding the operative risk factors, the suture technique and suture materials are very important factor. Continuous sutures were associated with a decreased rate of IH compared to interrupted sutures [26], and small tissue bites of 5 mm every 5 mm was also associated with a decreased rate of IH compared to large tissue bites of 10 mm every 10 mm [33]. Another report showed that the rate of developing IH in patients with a ratio of suture length to wound length ≥ 4 was less than that in patients with a ratio of < 4, indicating that tight suturing was not more effective than loose suturing in terms of preventing IH development [34]. Regarding suture materials, one meta-analysis showed that closure with continuous rapidly absorbable sutures was associated with a significantly greater risk of IH than closure by continuous slowly absorbable sutures or non-absorbable sutures [35]. In the current era, continuous loose suturing with small bites using slowly absorbable materials is typically performed for wound closing. However, in this study, the suture technique used to close abdominal wounds was a simple interrupted suturing technique using an absorbable braided suture material (1-Vicryl®). We changed the suture technique and material from 2017, so further investigation is needed in the point of these factors in the future.
One advantage of this study is its multicenter setting, which may have reduced some bias. In addition, the number of cases in this study was larger than that in most other single reports involving LCRS. Our median follow-up period (48.4 months) was also longer than in most other reports. IH formation is time-dependent, so the follow-up period is important.
However, this study has several limitations. First, this was a retrospective study, as opposed to a prospective design. Patients in this study were not followed prospectively to identify an IH. Second, our sample size was still relatively small, so larger studies are required. Third, the VFA and SFA measurement required the application. So, it may be limited to be able to measure these variables. Fourth, the BMI cut-off in Japan was lower than that of western countries. The number of BMI > 30 in Japan was less than in western countries, so further number are required to get to know whether BMI > 30 or 35 is independent risk factor of IH or not. Fifth, while we used the receiver operating characteristic curves to establish cut-off values for the VFA and SFA, no standardized cut-off values exist for the VFA and SFA. Sixth, the suture technique and materials were not current trend, so further investigation is needed in the point of these factors.
In conclusion, the incidence of IH was 8.5% at 4 years after LCRS, among the patients who had IH, about 90% of cases occurred within 2 years and about 97% of cases were detected by surveillance CT. After LCRS, we need for long term follow-up of at least 2 years to assess development of IH by surveillance CT. And this study established that a history of preoperative umbilical hernia and VFA ≥ 100 cm2 were significantly independent risk factors for IH after LCRS. In the case with an umbilical hernia or VFA ≥ 100 performing LCRS, it should likely NOT have a peri-umbilical extraction site and should be considered for an alternate site like a low transverse or Pfannenstiel incision.
References
Hoer J, Lawong G, Klinge U, Schumpelick V (2002) Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg 73:474–480
Mingoli A, Puggioni A, Sgarzini G, Luciani G, Corzani F, Ciccarone F, Baldassarre E, Modini C (1999) Incidence of incisional hernia following emergency abdominal surgery. Ital J Gastroenterol Hepatol 31:449–453
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Regnard JF, Hay JM, Rea S, Fingerhut A, Flamant Y, Maillard JN (1988) Ventral incisional hernias: incidence, date of recurrence, localization and risk factors. Ital J Surg Sci 18:259–265
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Clinical Outcomes of Surgical Therapy Study G, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, Group UMCT (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, Ito M, Saito S, Fujii S, Konishi F, Saida Y, Hasegawa H, Akagi T, Sugihara K, Yamaguchi T, Masaki T, Fukunaga Y, Murata K, Okajima M, Moriya Y, Shimada Y (2017) Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol 2:261–268
Benlice C, Stocchi L, Costedio MM, Gorgun E, Kessler H (2016) Impact of the specific extraction-site location on the risk of incisional hernia after laparoscopic colorectal resection. Dis Colon Rectum 59:743–750
Yamamoto M, Takakura Y, Ikeda S, Itamoto T, Urushihara T, Egi H (2018) Visceral obesity is a significant risk factor for incisional hernia after laparoscopic colorectal surgery: a single-center review. Asian J Endosc Surg 11:373–377
Lee L, Mata J, Droeser RA, Kaneva P, Liberman S, Charlebois P, Stein B, Fried GM, Feldman LS (2018) Incisional hernia after midline versus transverse specimen extraction incision: a randomized trial in patients undergoing laparoscopic colectomy. Ann Surg 268:41–47
Pares D, Shamali A, Stefan S, Flashman K, O'Leary D, Conti J, Senapati A, Parvaiz A, Khan J (2016) Predictive factors for extraction site hernia after laparoscopic right colectomy. Int J Colorectal Dis 31:1323–1328
Soderback H, Gunnarsson U, Hellman P, Sandblom G (2018) Incisional hernia after surgery for colorectal cancer: a population-based register study. Int J Colorectal Dis 33:1411–1417
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc 28:3421–3424
Samia H, Lawrence J, Nobel T, Stein S, Champagne BJ, Delaney CP (2013) Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg 205:264–267 (discussion 268)
Aquina CT, Rickles AS, Probst CP, Kelly KN, Deeb AP, Monson JR, Fleming FJ, Muscle, Adiposity Research C (2015) Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon Rectum 58:220–227
Watanabe J, Tatsumi K, Ota M, Suwa Y, Suzuki S, Watanabe A, Ishibe A, Watanabe K, Akiyama H, Ichikawa Y, Morita S, Endo I (2014) The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis 29:343–351
Examination Committee of Criteria for 'Obesity Disease' in J, Japan Society for the Study of O (2002) New criteria for 'obesity disease' in Japan. Circ J 66:987–992
Takahashi H, Mori M (2013) Characteristics and significance of criteria for obesity disease in Japan 2011. Nihon Rinsho 71:257–261
Yamada T, Okabayashi K, Hasegawa H, Tsuruta M, Abe Y, Ishida T, Matsui S, Kitagawa Y (2016) Age, preoperative subcutaneous fat area, and open laparotomy are risk factors for incisional hernia following colorectal cancer surgery. Ann Surg Oncol 23(Suppl 2):S236–241
Kinugasa T, Yoshida T, Mizobe T, Isobe T, Oka Y, Akagi Y (2015) The Impact of body mass index on perioperative outcomes after laparoscopic colorectal surgery. Kurume Med J 61:53–58
Jensen KK, Krarup PM, Scheike T, Jorgensen LN, Mynster T (2016) Incisional hernias after open versus laparoscopic surgery for colonic cancer: a nationwide cohort study. Surg Endosc 30:4469–4479
Petersson J, Koedam TW, Bonjer HJ, Andersson J, Angenete E, Bock D, Cuesta MA, Deijen CL, Furst A, Lacy AM, Rosenberg J, Haglind E, Group COcLoORIS (2018) Bowel obstruction and ventral hernia after laparoscopic versus open surgery for rectal cancer in a randomized trial (COLOR II). Ann Surg 269:53–57
Ihnat P, Tulinsky L, Jonszta T, Koscielnik P, Ihnat Rudinska L, Penka I (2018) Parastomal and incisional hernia following laparoscopic/open abdominoperineal resection: is there a real difference? Surg Endosc 33:1789–1794
Skipworth JR, Khan Y, Motson RW, Arulampalam TH, Engledow AH (2010) Incisional hernia rates following laparoscopic colorectal resection. Int J Surg 8:470–473
Bucknall TE, Cox PJ, Ellis H (1982) Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed) 284:931–933
Henriksen NA, Sorensen LT, Bay-Nielsen M, Jorgensen LN (2013) Direct and recurrent inguinal hernias are associated with ventral hernia repair: a database study. World J Surg 37:306–311
Lambert DM, Marceau S, Forse RA (2005) Intra-abdominal pressure in the morbidly obese. Obes Surg 15:1225–1232
Tanaka S, Horimai C, Katsukawa F (2003) Ethnic differences in abdominal visceral fat accumulation between Japanese, African–Americans and Cauca-sians: a meta-analysis. Acta Diabetol 40:S302–S304
Israelsson LA, Jonsson T (1996) Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 162:125–129
Lee L, Abou-Khalil M, Liberman S, Boutros M, Fried GM, Feldman LS (2017) Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: systematic review and meta-analysis. Surg Endosc 31:5083–5093
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FPH, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386:1254–1260
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Van't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J (2002) Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg 89:1350–1356
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Disclosures
Drs. Hironori Fukuoka, Jun Watanabe, Oshi Masanori, Yusuke Suwa, Shinsuke Suzuki, Hirokazu Suwa, Atsushi Ishibe, Mitsuyoshi Ota, Chikara Kunisaki and Itaru Endo have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fukuoka, H., Watanabe, J., Masanori, O. et al. The risk factors for incisional hernia after laparoscopic colorectal surgery: a multicenter retrospective study at Yokohama Clinical Oncology Group. Surg Endosc 35, 3471–3478 (2021). https://doi.org/10.1007/s00464-020-07794-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07794-z