Abstract
Purpose
Incisional hernia at the extraction site (ESIH) is a common complication after laparoscopic colorectal resections. The aim of this study was to evaluate the prevalence and potential risk factors for ESIH in a large cohort study having standardized technique.
Methods
A cross-sectional study was performed including all patients who underwent elective laparoscopic right or extended right colectomy for cancer from November 2006 to October 2013 using a standard technique. All patients have been followed up for a minimum of 1 year with abdominal CT scan.
Results
A total of 292 patients were included with a median follow-up of 42 months. Twenty patients (6.8 %) developed ESIH. Obesity (odds ratio (OR) = 3.76, 95 % confidence interval (CI) 1.39–10.15; p = 0.009) and incision length (OR 2.86, 95 % CI 1.077–7.60; p = 0.035) significantly predisposed to the development of ESIH.
Conclusion
This study identified that the risk of ESIH is significant after colonic resections and there are several risk factors responsible for the development of ESIH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic resection is now the standard surgical treatment for colon cancer [1, 2]. For cancer of the right colon, this comprises right or extended right hemicolectomy according to the location of the tumor [3, 4]. Mostly, the specimen is removed via an extraction site wound in the abdominal wall.
Incisional hernia at the extraction site (ESIH) appears to be one of the most frequent complications after laparoscopic colorectal resection with an incidence of 5–20 % in published series [5–7].
An understanding of risk factors for ESIH would provide a useful basis for consenting patients before operation and for designing interventions to prevent this complication. Published series have been mostly heterogeneous with regard to pathology, operation performed, or duration of follow-up, making it difficult to draw firm conclusions [8, 9].
The aim of this study was to analyze the risk factors and prevalence of ESIH on CT scan at a minimum follow-up of 1 year in a cohort of patients, all of whom have undergone laparoscopic resection for right-sided colon cancer.
Methods
A retrospective analysis was undertaken of patients data collected prospectively on our colorectal surgery database from November 2006 to October 2013. This is a cross-sectional study of patients who underwent elective laparoscopic right or extended right colectomy for cancer in the study period.
Inclusion and exclusion criteria
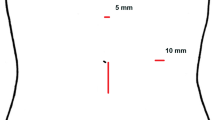
All consecutive patients with cancer in the right colon (cecum, ascending colon, hepatic flexure, and transverse colon) who underwent elective laparoscopic right hemicolectomy or extended right hemicolectomy during an 8-year study period were included in the analysis. Patients underwent standard CT staging of the chest, abdomen, and pelvis preoperatively and again at a minimum 1 year postoperatively using a multislice CT scanner (Siemens™) with a slice of 3 mm. Operative data were recorded on a proforma, which included the location and length of the extraction site wound. All CT scans were reported by a consultant radiologist and reviewed for evidence of ESIH (Fig. 1). Exclusion criteria were as follows: conversion to laparotomy, surgical reintervention through a laparotomy, natural orifice extraction of specimen, follow-up less than 1 year, and/or without a follow-up abdominal CT scan. No single-incision surgical procedure (SILS) was included in the study.
Surgical technique and postoperative management
All cancer resections were performed by experienced laparoscopic consultant surgeons or by higher surgical trainees under direct supervision using a standardized technique which we have previously published [10]. Laparoscopic mesocolic excision was performed in all cases adhering to oncological principles of cancer resection. No bowel preparation was used. Port placement for right colonic resections included the use of four trocars (two 12 mm and two 5 mm). Primary vascular ligation was followed by medial to lateral dissection and then division of colon with clear margins. The location of the extraction site wound was decided by the surgeon, and in all cases, we used a wound protector. Fascial closure used a running suture of loop “0” PDS in one or two layers, for midline incision or other sites, respectively. The 12-mm port site was also closed with an interrupted absorbable suture. The skin was closed with an absorbable subcuticular suture. Patient-controlled analgesia (PCA) or local blocks were the preferred option for pain relief, although epidural analgesia was used in a minority. Postoperatively, patients were managed in an enhanced recovery program.
Study variables
The principal endpoint was the presence or absence of an incisional hernia at the extraction site (ESIH) on CT scan at a minimum of 1 year after surgery. The following variables were analyzed: age, gender, BMI, American Society of Anesthesiologists (ASA) grade, operative data (including technique and operative time, length and site of extraction incision), and postoperative complications. Pathological characteristics of the specimen were included in the study. Tumors were staged according to the seventh edition of the TNM staging system [11].
Statistical analysis
All results and variables were logged on a specially designed database. Continuous variables are presented as mean ± standard deviation, ranges, and categorical variables as absolute numbers or percentages. Chi-square tests were used to compare differences in categorical variables (Fisher’s exact tests were used as needed), and Student’s t tests were used for continuous variables. Univariate analysis and multivariate logistic regression analysis were performed to identify independent predictive factors for the development of ESIH. Adjusted odds ratios (ORs) were calculated using logistic regression. Variables achieving statistical significance in the univariate analysis were considered for multivariate analysis. ORs with 95 % confidence intervals (CIs) are presented for each studied variable. Differences were considered to be significant at the 5 % level. All p values reported were two sided. Statistical analyses were performed using SPSS version 20.0 (SPSS™, Inc., Chicago, IL, USA).
Results
From November 2006 to August 2014, we performed 352 laparoscopic right or extended right hemicolectomies. Figure 2 provides the flow chart of all patients included in this series. After several exclusions, the data of 292 patients were included in the final analysis.
There were 127 males (43.5 %) and 165 females (56.5 %), with a mean age of 73.3 ± 10.46 years and a mean BMI of 26.2 ± 4.74 kg/m2. Overall, 35.9 % of patients had previous abdominal surgery and 32.8 % an ASA grade greater than III.
During a median follow-up of 42 months (range 12–96), 20 patients (6.8 %) developed ESIH. Table 1 shows the characteristics of patients who developed ESIH versus those who did not. There were no significant differences between groups in the characteristics of tumor, surgical technique, or postoperative data. The rate of ESIH appeared to be significantly greater in those with a higher BMI (p = 0.004) or a longer extraction site wound (p = 0.023). There was also a greater prevalence of ESIH in patients with a periumbilical midline extraction site (9.1 %) compared with other sites (3.4 %), but this did not reach statistical significance (p = 0.062) (Table 1).
On multivariate analysis, a BMI >30 (odds ratio [OR] = 3.76, 95 % confidence interval (CI) 1.39–10.15; p = 0.009) and an incision length more than 5 cm (OR 2.86, 95 % CI 1.077–7.60; p = 0.035) were significant independent predictors of ESIH (Table 2).
Of the 20 patients with ESIH, 6 of them underwent surgical repair because of symptoms or cosmetic concerns. The remaining 14 are awaiting surgery, or surgery is not warranted for several reasons (i.e., comorbidities).
Discussion
We report that approximately 7 % of patients developed an extraction site incisional hernia after standardized laparoscopic resection for right-sided colon cancer as evidenced by CT scan at a year or more postoperatively.
The strength of this study is that it is the largest analysis of incisional hernia in a homogenous series of patients who had a laparoscopic procedure for a right-sided colon cancer with a standardized technique. A limitation is that although the data was collected prospectively, this is a retrospective analysis and some confounders were not studied as diabetes mellitus or smoking habit.
There is some controversy regarding the most appropriate method of detecting ESIH. The yield of incisional hernias on CT is perhaps double the clinical rate of detection [7]. However, while many hernias detected on CT may never become clinically significant, CT is more accurate than clinical examination in detecting the presence or absence of a hernia and is therefore more valuable in the research setting. However, the cross-sectional design based on yearly CT scan hampered identification of the specific time after surgery at which hernia occurred.
Across the spectrum of laparoscopic colon resections, ESIH is recognized as one of the most common complications [5]. The incidence of this clinical condition ranges from 5 to 20 % of patients in some series [7, 12]. Apart from our series, the largest published experience included 1057 cases [13]. However, that was a retrospective series, including open and laparoscopic procedures. In their results from 137 laparoscopic right colonic resections followed up, 15.9 % developed incisional hernia (including port site hernia) and specifically 5.1 % on the midline incision for the laparoscopic right colectomies. The present study in patients undergoing right-sided colonic resection for bowel cancer reports ESIH in 6.8 %.
Previous studies have reported a range of factors associated with ESIH. Sadava et al. [8], in a series of patients operated for cancer and benign diseases, found BMI and surgical site infection to be significant predictors of ESIH. Compared with standard laparoscopic surgery, single-incision technique (SILS) has been reported to increase the risk of ESIH [9]. Interestingly, in a recent study, in a series of 193 patients operated for colorectal cancer with open or laparoscopic techniques, visceral obesity measured by CT scan rather than BMI was a significant predictor of incisional hernia [12].
One of the most controversial issues is whether there is any benefit in using a midline incision vs. other sites for specimen extraction after colonic resection. Lim et al. [14] compared midline and transverse incisions in 147 left sided laparoscopic procedures (sigmoid and rectal cancer resections). They did not find any differences between clinical complications (transumbilical incision 2/92 vs. left transverse incision 0/55, p = 0.810). Williams et al. [15] demonstrated, in a prospective series of 15 patients, the benefit of using a transverse right incision and preservation of rectus abdominis muscle. There is no control arm, but in their experience, none of the patients in a 24-month follow-up developed any incisional hernia. However, Singh et al. [16] in 2008 reporting on 208 laparoscopic colonic resections observed a 7.8 % ESIH rate for midline extraction wound versus 0 % for other extraction sites. In our experience, the rate of ESIH was higher in the group of patients with midline incision, but the difference did not reach statistical significance. It is important to note that our study included a relatively homogeneous group of patients undergoing a standardized operation. The only real variables introduced by the surgeon were the location of extraction site and length of the wound.
Non-controlled trials have proposed intracorporeal anastomosis in laparoscopìc right colectomy to diminish the size of the extraction site incision and potentially reduce the rate of abdominal wall complications [17–20]. However, it is usually the specimen size rather than the extracorporeal anastomosis that determines the length of the extraction wound (except for NOTES). Finally, use of prophylactic mesh has been suggested to prevent incisional hernia in patients at risk [21]. The scientific evidence is scarce, but recently, a RCT has published its benefits in colorectal surgery when an open procedure was carried out [22]. We are not aware of any published data on use of prophylactic mesh in laparoscopic colorectal surgery except in the prevention of port site incisional hernias in laparoscopic cholecystectomy [23].
Patients undergoing laparoscopic colon resection need to be informed that although their surgery is planned as a minimally invasive procedure with associated benefits, nonetheless, an extraction site through the abdominal wall is usually required and this is associated with a significant risk of hernia which may require further surgery in due course. This risk is especially high in patients who are overweight, and they need to be so advised.
Regarding surgical technique, the risk of ESIH may be reduced by using extraction sites away from the umbilicus (possibly NOTES) and by keeping the extraction wound short.
In conclusion, increased BMI, longer extraction wound length and possibly periumbilical extraction site all increase the risk of ESIH after standardized laparoscopic right hemicolectomy for cancer.
References
Zerey M, Hawver LM, Awad Z, Stefanidis D, Richardson W, Fanelli RD (2013) SAGES evidence-based guidelines for the laparoscopic resection of curable colon and rectal cancer. Surg Endosc 27:1–10
Lujan HJ, Plasencia G, Jacobs M, Viamonte M 3rd, Hartmann RF (2002) Long-term survival after laparoscopic colon resection for cancer: complete five-year follow-up. Dis Colon rectum 45:491–501
Lin KM, Ota DM (2000) Laparoscopic colectomy for cancer: an oncologic feasible option. Surg Oncol 9:127–134
Feng B, Sun J, Ling TL, et al. (2012) Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 26:3669–3675
Borie F, Bigourdan JM, Pissas MH, Ripoche J, Millat B (2014) The best surgical approach for left colectomy: a comparative study between transverse laparotomy, midline laparotomy and laparoscopy. J Gastrointest Surg 18:1010–1016
Llaguna OH, Avgerinos DV, Lugo JZ, et al. (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg:265–269
Claes K, Beckers R, Heindryckx E, et al. (2014) Retrospective observational study on the incidence of incisional hernias after colorectal carcinoma resection with follow-up CT scan. Hernia 18:797–802
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc 28:3421–3424
Sangster W, Kulaylat AN, Stewart DB, Schubart JR, Koltun WA, Messaris E (2015) Hernia incidence following single-site vs standard laparoscopic colorectal surgery. Color Dis 17:250–256
Hemandas A, Flashman KG, Farrow J, O’Leary DP, Parvaiz A (2011) Modular training in laparoscopic colorectal surgery maximizes training opportunities without clinical compromise. World J Surg 35:409–414
Sobin LH, Gospodarowicz MK, Wittekind Ch. Eds. TNM classification of malignant tumours, 7th ed. Wiley-Blackwell, Oxford 2009.310 pages.
Aquina CT, Rickles AS, Probst CP, et al. (2015) Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon rectum 58:220–227
Mishra A, Keeler BD, Maxwell-Armstrong C, Simpson JA, Acheson AG (2014) The influence of laparoscopy on incisional hernia rates: a retrospective analysis of 1057 colorectal cancer resections. Color Dis 16:815–821
Lim SW, Huh JW, Kim YJ, Kim HR (2013) Vertical transumbilical incision versus left lower transverse incision for specimen retrieval during laparoscopic colorectal surgery. Technol Coloproctol 17:59–65
Williams GL, Beaton C, Codd R, Stephenson BM (2012) Avoiding extraction site herniation after laparoscopic right colectomy. Technol Coloproctol 16:385–388
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
Mufty H, Hillewaere S, Appeltans B, Houben B (2012) Single-incision right hemicolectomy for malignancy: a feasible technique with standard laparoscopic instrumentation. Color Dis 14:e764–e770
Carnuccio P, Jimeno J, Parés D (2014) Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Technol Coloproctol 18:5–12
Milone M, Elmore U, Di Salvo E, et al. (2015) Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29:2314–2320
Raftopoulos I, Courcoulas AP, Blumberg D (2006) Should completely intracorporeal anastomosis be considered in obese patients who undergo laparoscopic colectomy for benign or malignant disease of the colon? Surgery 140:675–682
Hidalgo MP, Ferrero EH, Ortiz MA, Castillo JM, Hidalgo AG (2011) Incisional hernia in patients at risk: can it be prevented? Hernia 15:371–375
Garcia-Urena MA, Lopez-Monclus J, Hernando LA, et al. (2015) Randomized controlled trial of the use of a large-pore polypropylene mesh to prevent incisional hernia in colorectal surgery. Ann Surg 261:876–881
Armananzas L, Ruiz-Tovar J, Arroyo A, et al. (2014) Prophylactic mesh vs suture in the closure of the umbilical trocar site after laparoscopic cholecystectomy in high-risk patients for incisional hernia. A randomized clinical trial. J Am Coll Surg 218:960–968
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Parés, D., Shamali, A., Stefan, S. et al. Predictive factors for extraction site hernia after laparoscopic right colectomy. Int J Colorectal Dis 31, 1323–1328 (2016). https://doi.org/10.1007/s00384-016-2610-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2610-x