Abstract
Background
The use of ultrasonography to assist needle placement during transverse abdominal plane (TAP) technique has provided direct visualization of surround anatomical musculature and facial planes. However, the increased girth in patients undergoing bariatric surgery is challenging to visualize via ultrasonography which may lead to poor postoperative analgesia.
Objective
The aim of the study is to investigate whether the addition of postoperative laparoscopic-guided TAP block as part of a multimodal analgesic regimen within the ERAS protocol compared to no block provides better postoperative analgesia in patients undergoing one-anastomosis gastric bypass surgery.
Patients and methods
A prospective clinical trial was performed. Patients were randomized into two groups: patients undergoing postoperative laparoscopic-guided TAP (TAP-lap) and patients not receiving TAP-lap (Control). Multimodal analgesia included preoperative port-site infiltration with Bupivacaine 0.25% in both groups and systemic Acetaminophen. Pain quantification as measured by visual analogic scale (VAS) was assessed at 6 and 24 h after surgery, and 24-h postoperative opioid consumption.
Results
One hundred and forty patients were included, 70 in each group. The mean operation time was 78.5 ± 14.4 min in TAP-lap and 75.9 ± 15.6 min in Control (NS). The mean postoperative pain, as measured by VAS, 6 h after surgery was 23.1 ± 11.3 mm in TAP-lap and 41.8 ± 16.2 mm in Control (p = 0.001).
24 h after surgery was 16.6 ± 11.4 mm in TAP-lap and 35.4 ± 12.7 mm in Control (p = 0.001).
Morphine rescues were necessary in 14.2% in Control and 2.8% in TAP-lap (p = 0.035).
Conclusion
Laparoscopic-guided TAP block as part of a multimodal analgesia regimen can reduce postoperative pain and opioid consumption, without increasing operative time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bariatric surgery, usually performed laparoscopically, is an effective procedure to reduce and maintain weight loss in morbidly obese patients [1]. Despite the laparoscopic approach has significantly reduced the postoperative pain, it is still present. Thus, an adequate management of postoperative pain remains a challenge, as it is closely related with a decrease in the quality of life in the immediate postoperative period [2]. Several multimodal analgesia schemes, as part of Enhanced Recovery After Surgery (ERAS) programs, have been proposed, aiming to reduce postoperative pain, reduce postoperative opioid consumption, and shorten hospital stay [3,4,5,6]. Multimodal analgesia involves the use of opioids, local anesthetics, and non-steroidal anti-inflammatory drugs, all with different pharmacological actions in order to maximize analgesic efficacy, while reducing the risk and severity of adverse events, mostly associated with systemic opioids administration [7]. During laparoscopic surgery, it is common for the surgeon to infiltrate the laparoscopic ports with local anesthetics. We previously demonstrated that the association of port-site infiltration to intravenous analgesia improved the pain control [8].
The transversus abdominal plane block is a regional anesthesia technique that consists of placing local anesthetic into the fascial planes between the transversus abdominis muscles providing analgesia to the anterior-lateral abdominal wall [9, 10]. TAP blocks are routinely performed for pain control after laparoscopic surgery at many institutions [11]. The provided analgesic effect reduces the risk of postoperative cardiopulmonary complications, which are more prone to appear on morbidly obese subjects [12, 13]. The ultrasound guidance allows a greater precision of needle placement in the desired tissue plane [14]. However, the increased girth in patients undergoing bariatric surgery is challenging to visualize via ultrasonography, which may lead to poor postoperative analgesia [15, 16].
Morbidly obese patients particularly benefit from opioid-sparing analgesia. Therefore, the application of loco-regional techniques, such as TAP block, must be maximized. Our group developed the technique of laparoscopic-guided TAP block in patients undergoing Roux-en-Y gastric bypass (RYGB), and observed a greater analgesic effect of laparoscopic-guided TAP than port-site infiltration [17].
The aim of this study was to determine if postoperative laparoscopic-guided TAP block adds analgesic effect to preoperative port-site infiltration, as part of a multimodal analgesia scheme within an ERAS program, in patients undergoing One-Anastomosis gastric bypass (OAGB).
Patients and methods
A prospective randomized clinical trial of patients undergoing OAGB at an International Federation for Surgery of Obesity (IFSO) Center of Excellence was performed between December 2018 and March 2019. Inclusion criteria consisted of adult patients who were scheduled to undergo one-anastomosis gastric bypass (OAGB) procedure with either a BMI > 40 kg/m2 or > 35 kg/m2 with the presence of comorbidities associated with obesity (i.e., Type 2 Diabetes Mellitus, hypertension, dyslipidemia, sleep apnea). Patients were excluded if they were scheduled for additional surgeries (band removal, cholecystectomy, hernioplasty, or hiatal hernia treatment), history of foregut surgery, bariatric-revision surgery, history of allergy to local anesthetics, coagulopathy or anticoagulation, and those patients who refused TAP block.
The sample size calculation was based on historic data of our center of postoperative pain quantification by Visual Analogic Scale (VAS) 24 h after surgery in patients undergoing preoperative port-site infiltration with Bupivacaine 0.25% associated with postoperative intravenous analgesia (Control Group-40 mm) and an expected reduction to 25 mm in patients undergoing the combination of preoperative port-site infiltration, intravenous analgesia, and postoperative laparoscopic-guided TAP block with Bupivacaine (Experimental group). At 80% power and a significance level of p = 0.05, it was calculated that 70 patients were required in each arm of the study.
Patients were randomized using a computerized simple randomization scheme in a 1:1 ratio into two groups: patients undergoing postoperative laparoscopic-guided TAP associated to postoperative intravenous analgesia and preoperative port-site infiltration (TAP-lap Group) compared to those ones receiving only postoperative intravenous analgesia associated with preoperative port-site infiltration (Control Group) (Supplementary Material 2).
Surgical technique
The laparoscopic procedure consisted of the placement of 6 ports: right and left flank (12 mm), supraumbilical (10 mm), right and left hypochondrium, and right iliac fossa (5 mm). A 20-cm-long gastric pouch, calibrated with a 36-Fr bougie was constructed. Termino-lateral gastro-jejunal anastomosis with linear stapler (I-Drive with Tri-staple cartridges, Medtronic, USA) was performed. The holes were sutured with continuous barbed suture V-Loc 2/0 (Medtronic, USA). The total bowel length was determined; the biliopancreatic limb length represented 60% of the total bowel length and the common limb 40%. Mesenteric defects were not closed in any of the cases. The integrity of the anastomoses and staple lines were checked with intraoperative methylene blue dye.
Analgesic technique
Preoperative port-site infiltration was performed by the surgeon with 10 ml of Bupivacaine 0.25%, applying 1.5 ml under the aponeurotic layer in each port.
Intravenous analgesia included acetaminophen 1 g/6 h.
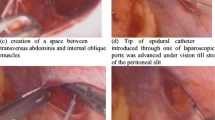
Bupivacaine 0.25% 30 ml was used for TAP-lap. The drug was injected into the plane between the internal oblique and the transversus abdominis muscles, as previously reported [13]. Local anesthetic injection was placed at the dermatome level, just lateral to the port insertion sites (Fig. 1). The local anesthetic was injected sequentially with 5 mL of bupivacaine 0.25% into the fascial plane between the internal oblique and the transversus abdominis muscles at each of the three corresponding port sites on the right and left side for a total volume of 30 ml. At each port site, the laparoscopic guidance consists in the insertion of the needle until the tip protrudes on the peritoneal layer. Then the needle is retracted 3 mm into the abdominal wall, which is the estimated thickness of the preperitoneal space and the transversus abdominis muscle, so that the anesthetic drug is injected into the space between the internal oblique muscle and the transversus abdominis muscle, forming a bulge protruding on to the peritoneum (Fig. 2).
Patients who reported postoperative pain greater than a VAS score of 50 mm received subcutaneous morphine 5 mg until discharged from the hospital.
Prophylaxis of nauseas and vomiting (PONV)
The prophylaxis regimen used was according to the Spanish National Enhanced Recovery After Surgery (ERAS) protocol for bariatric surgery [18], and specifically following the Apfel scale [19]. Given that most patients were women (females are more prone to present PONV, following Apfel scale criteria), without history of smoking at the time of surgery (stop of tobacco habit was mandatory at least 8 weeks prior to surgery), and undergoing a surgery involving the stomach, all the patients were considered as high-risk patients for postoperative nausea or vomiting (PONV).
Thus, all the patients received pharmacologic prophylaxis with triple therapy, including Dexamethasone during the anesthetic induction, and Droperidol and Ondansetron at the end of the surgery.
Variables
Primary outcome of this study was pain quantification as measured by Visual Analogic Scale (VAS), ranging from 0 mm (absence of pain) to 100 mm (unbearable pain) at 24 h after surgery. Secondary outcomes include pain quantification at 6 h after surgery, surgical duration, opioid consumption during the first 24 h, PONV, complications, and hospital stay. Pain quantification during the first 24 h was evaluated by a nurse blinded to the treatment applied.
Statistics
Statistical analysis was performed with the statistical software SPSS 22.0 for Windows. Quantitative variables that followed a normal distribution were defined by the mean and standard deviation. For non-Gaussian variables, the median and range were used. Qualitative variables were defined by number and percentage of cases.
Comparison of variables was performed with Student t test (Mann–Whitney test in non-Gaussian variables). Comparison of qualitative variables was performed with the Chi-square test; in those cases with fewer than five observations in the cell the Fisher exact probability method was used. p < 0.05 was regarded as significant. An intent-to-treat analysis was performed.
The study was approved by the local ethics committee and informed consent was obtained from all the patients.
Results
A total of one hundred and forty obese patients were included in the study; no patients were excluded. The two groups were comparable with respect to age, gender, comorbidities, weight, and BMI (Table 1).
Mean operation time was 78.5 ± 14 min in TAP-lap Group and 75.9 ± 12.6 min in Control Group (Non-significant—NS). Postoperative complications appeared in 1 patient in each group (1.4%): one abdominal wall hematoma in the right iliac fossa, adjacent to the placement of the 5-mm port in TAP-lap Group, and one subcutaneous emphysema secondary to the pneumoperitoneum in the Control Group. Both complications were conservatively managed and recovered uneventfully. There was no mortality or readmission in any of the groups.
When analyzing the postoperative pain, patients presenting complications were not excluded, as this is an intention-to-treat analysis. The mean postoperative pain, as measured by VAS, 6 h after surgery was 23.1 ± 11.3 mm in TAP-lap Group and 41.8 ± 16.2 mm in Control Group (p = 0.001). 24 h after surgery, postoperative pain was 16.6 ± 11.4 mm in TAP-lap Group and 35.4 ± 12.7 mm in Control Group (p = 0.001).
Morphine rescues were necessary in 2 patients (2.8%) in TAP-lap Group and in 10 patients (14.2%) in the Control Group (OR 4.47, CI 95% (1.7–11.2); p = 0.035). All the patients with morphine rescue needs required only a single administration of 5 mg subcutaneous morphine chloride during the first 24 h postoperatively. Later morphine rescues were not necessary in any cases. During hospital stay, PONV appeared in 1 patient (1.4%) in TAP-lap Group and 8 patients (11.4%) in Control Group (OR 4.27, CI 95% (1.8–10.6); p = 0.039). All the patients with PONV received morphine rescues. Median hospital stay was 1 day (range 1–2 days) in both groups (NS). Hospital discharge during the first 24 h in 95.7% of the patients in TAP-lap Group and in 87.1% of the cases in Control Group (p = 0.07).
Discussion
Port-site infiltration with local anesthetic drugs is a usual procedure employed for multimodal analgesia. However, its analgesic efficacy remains unclear. Several series report excellent postoperative analgesia [20, 21], whereas other studies could not demonstrate this efficacy [22]. A previous study of our group showed that port-site infiltration with Bupivacaine achieved similar analgesic efficacy than epidural analgesia in patients undergoing bariatric surgery [8].
Moncada et al. reported that the port-site infiltration achieves a significant pain reduction only during the first 4 postoperative hours, but no longer. They performed preoperative infiltration with bupivacaine, which is a drug with a half-life significantly shorter than the time frame examined [23]. Actually, there is a great controversy about the optimal time of infiltration with local anesthetic drugs. Some groups defend the preoperative application in order to reduce unpleasant sensations and autonomic reactions to injury, as nociceptors are activated by inflammation and injury, giving rise to painful and non-painful sensations that influence feeding and illness behavior [24, 25]. Local anesthetics have shown to present an anti-inflammatory effect, which modulates the immune response to surgical intervention [24, 25]. However, other authors defend a postoperative infiltration to prolong the duration of the anesthetic after surgery [26, 27]. Moon et al. have solved this dilemma, using liposomal bupivacaine, a long-acting local anesthetic with half-life of 96 h. They performed a TAP block preoperatively and observed a significant reduction of postoperative morphine needs during all the hospital stay [28]. However, liposomal bupivacaine is expensive and not available at all institutions and further studies should confirm the initial results obtained.
In our Control Group, only with preoperative port-site infiltration, the postoperative pain assessment revealed a mild pain relief, with mean VAS measurements of 41.8 mm at 6 h after surgery and 35.4 mm at 24 h, and requiring a morphine rescue in 14.2% of the patients. Considering that the half-life of Bupivacaine is 8 h, even the pain determination 6 h after surgery showed a loss of analgesic effect.
Andersen et al. [29] conducted a systematic review on different analgesic treatment options in laparoscopic gastric bypass surgery. They conclude that port-site infiltration and TAP block are effective analgesic methods, but there are no studies comparing both approaches. Many anesthesiologists defend TAP block as superior to port-site infiltration and prefer to carry out a TAP block, once they decide to perform an ultrasound-guided infiltration. In order to reduce the difficulties in the identification of the transversus abdominis plane when performing ultrasound-guided TAP blocks in bariatric patients, we developed the laparoscopic guidance [17]. The laparoscopic TAP block technique provides direct visualization of the target area. However, it is not as precise as ultrasonography delineating the interfacial planes and surrounding musculature. Therefore, we suggest using ultrasonographic confirmation of local anesthetic spread, at least during the learning curve.
In the present study, we aimed to evaluate the addition of postoperative laparoscopic TAP block to preoperative port-site infiltration with isolated preoperative port-site infiltration, and observed a significantly better pain relief and lower morphine rescue needs in the TAP-lap Group. In our opinion, a synergistic effect of the multimodal regimen probably accounts for the success of the postoperative analgesia seen in our study. The port infiltration with local anesthetic reduces the pain generation, whereas the laparoscopic TAP block prolongs the analgesic effect.
A limitation for the external validation of this technique is that the TAP-lap was performed by trained surgeons in this approach. In our previous study evaluating the initial implementation of this procedure in RYGB [17], the first ten cases of TAP-lap block were validated with ultrasonographic confirmation of the anesthetic infiltration in the correct plane, considering it as the learning curve. Anyway, further prospective randomized studies should be conducted to confirm a similar efficacy in laparoscopic-guided and ultrasound-guided TAP block.
Conclusion
Laparoscopic-guided TAP block, associated to preoperative port-site infiltration, as part of a multimodal analgesia scheme, can reduce postoperative pain and opioid rescue needs, without increasing operative time.
References
Bray GA (2004) Medical consequences of obesity. J Clin Endocrinol Metab 89:2583–2589
Wu CL, Naqibuddin M, Rowlingson AJ et al (2003) The effect of pain on health-related quality of life in immediate postoperative period. Anesth Analg 97:1078–1085
Aronsohn J, Orner G, Palleschi G, Gerasimov M (2019) Opioid-free total intravenous anesthesia with ketamine as part of an enhanced recovery protocol for bariatric surgery patients with sleep disordered breathing. J Clin Anesth 52:65–66
Aktimur R, Kirkil C, Yildirim K, Kutluer N (2018) Enhanced recovery after surgery (ERAS) in one-anastomosis gastric bypass surgery: a matched-cohort study. Surg Obes Relat Dis 14:1850–1856
Lam J, Suzuki T, Bernstein D et al (2019) An ERAS protocol for bariatric surgery: is it safe to discharge on post-operative day 1? Surg Endosc 33:580–586
De Oliveira GS, Jr (2018) Optimal analgesic regimen for bariatric surgery: no opioid is rarely the option. J Clin Anesth 51:123–124
American Society of Anesthesiologists Task Force on Acute Pain Management (2012) Practice guidelines for acute pain management in the postoperative setting: an updated report by the American Society of Anesthesiologists Task Force on acute pain management. Anesthesiology 116:248–273.
Ruiz-Tovar J, Muñoz JL, Gonzalez J et al (2017) Postoperative pain after laparoscopic sleeve gastrectomy: comparison of three analgesic schemes (isolated intravenous analgesia, epidural analgesia associated with intravenous analgesia and port-sites infiltration with bupivacaine associated with intravenous analgesia). Surg Endosc 31:231–236
McDonnell JG, O’Donnell BD, Farrell T et al (2007) Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med 32:399–404
El-Dawlatly AA, Turkistani A, Kettner SC et al (2009) Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth 102:763–767
Wassef M, Lee DY, Levine JL et al (2013) Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J Pain Res 6:837–841
Ahmad S, Nagle A, McCarthy RJ et al (2008) Postoperative hypoxemia in morbidly obese patients with and without obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesth Analg 107:138–143
Rosenberg-Adamsen S, Lie C, Bernhard A et al (1999) Effect of oxygen treatment on heart rate after abdominal surgery. Anaesthesiology 90:380–384
Hadzic A (2007) Textbook of regional anesthesia and acute pain management, 1st edn. McGraw-Hill, New York
Nielsen KC, Guller U, Steele SM et al (2005) Influence of obesity on surgical regional anesthesia in the ambulatory setting: an analysis of 9,038 blocks. Anaesthesiology 102:181–187
Ruiz-Tovar J, Albrecht E, Macfarlane A et al (2019) The TAP block in obese patients: pros & cons. Minerva Anestesiol. https://doi.org/10.23736/S0375-9393.19.13545-6
Ruiz-Tovar J, Garcia A, Ferrigni C et al (2018) Laparoscopic-Guided transversus abdominis plane (TAP) block as part of multimodal analgesia in laparoscopic Roux-en-Y gastric bypass within an enhanced recovery after surgery (ERAS) program: a prospective randomized clinical trial. Obes Surg 28:3374–3379
Ruiz-Tovar J, Royo P, Munoz JL et al (2016) Implementation of the Spanish National Enhanced Recovery after Surgery (ERAS) program in bariatric surgery: a pilot study. Surg Laparosc Endosc Percutan Techn 26:439–443
Apfel CC, Heidrich FM, Jukar-Rao S et al (2012) Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth 109:742–753
Lee IO, Kim SH, Kong MH et al (2001) Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. Can J Anesth 48:545–550
Jimenez Fuertes M, Costa ND (2015) Colecistectomía laparoscópica ambulatoria y control del dolor postoperatorio: presentación de una serie de 100 casos. Cir Esp 93:181–186
Tam T, Harkins G, Wegrzyniak L et al (2014) Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol 21:1015–1021
Moncada R, Martinaitis L, Landecho M et al (2016) Does preincisional infiltration with bupivacaine reduce postoperative pain in laparoscopic bariatric surgery? Obes Surg 26:282–288
Burns AJ, Pachnis V (2009) Development of the enteric nervous system: bringing together cells, signals and genes. Neurogastroenterol Motil 21:100–102
Grundy D, Al-Chaer ED, Aziz Q et al (2006) Fundamentals of neurogastroenterology: basic science. Gastroenterology 130:1391–1411
Albrecht E, Kirkham KR, Endersby RV et al (2013) Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastricbypass surgery: a prospective randomized controlled doubleblinded trial. Obes Surg 23:1309–1314
Sinha A, Jayaraman L, Punhani D (2013) Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg 23:548–553
Moon RC, Lastrapes L, Wier J et al (2019) Preoperative Transversus abdominis plane (TAP) block with liposomal bupivacaine for bariatric patients to reduce the use of opioid analgesics. Obes Surg 29:1099–1104
Andersen LP, Werner MU, Rosenberg J et al (2014) Analgesic treatment in laparoscopic gastric bypass surgery: a systematic review of randomized trials. Obes Surg 24:462–470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jaime Ruiz-Tovar, MD, PhD; Gilberto Gonzalez, MD; Andrei Sarmiento, MD; Miguel A. Carbajo, MD, PhD; Javier Ortiz-de-Solorzano, MD; Maria Jose Castro, MD, PhD; Jose Maria Jimenez, PhD; and Lorea Zubiaga, MD, PhD have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ruiz-Tovar, J., Gonzalez, G., Sarmiento, A. et al. Analgesic effect of postoperative laparoscopic-guided transversus abdominis plane (TAP) block, associated with preoperative port-site infiltration, within an enhanced recovery after surgery protocol in one-anastomosis gastric bypass: a randomized clinical trial. Surg Endosc 34, 5455–5460 (2020). https://doi.org/10.1007/s00464-019-07341-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07341-5