Abstract
Background
The efficacy of ultrasound-guided transversus abdominis plane (USG-TAP) block as a part of multimodal analgesia was evaluated in morbidly obese patients undergoing laparoscopic bariatric surgery.
Methods
We studied 100 patients with body mass index >35 kg/m2. They were randomly allocated to study (USG-TAP) and control groups. Pain scores at rest and on movement at various time points up to 24 postoperative hours were compared. Other parameters evaluated were patients requiring Tramazac hydrochloride (TMZ) as rescue analgesic, sedation score, time to ambulate, any adverse events, and patient satisfaction.
Results
The median visual analogue scale pain score of the study (USG-TAP) group was consistently lower at 1, 3, 6, 12, and 24 h at rest and on movement, in the postoperative period. Number of patients requiring TMZ required in the first, third, and sixth hour was significantly lower in the USG-TAP group. The prolonged sedative effect of the TMZ affected the time to ambulate. Patients in the control group remained more sedated. Four patients in the control group required BIPAP support postoperatively; no adverse event was observed. Time to ambulate was 6.3 ± 1.8 h in USG-TAP and 8 ± 1.8 h in control groups; P < 0.001. Patient satisfaction scores were significantly higher in the USG-TAP group; P < 0.001.
Conclusions
Our study demonstrates that the USG-TAP as part of multimodal analgesic technique in morbidly obese patients undergoing laparoscopic gastric bypass reduces opioid requirement, improves pain score, decreases sedation, promotes early ambulation, and has greater patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and Introduction
The pathophysiology of obesity, typical comorbidities and the high prevalence of obstructive sleep apnea among obese patients make safe analgesic management difficult. In particular, pain control after bariatric surgery is a major challenge. General anesthesia in morbidly obese (MO) is associated with multiple risks, which can be further aggravated with sedation, immobilization, and hypoventilation from administration of narcotic analgesics in the postoperative period [1–5]. Moreover, due to association with moderate to severe sleep apnea, usage of sedative analgesia may have adverse outcome. Pain management remains key aspect in the perioperative anesthetic care and single most important determinant of patient safety. The MO patients can benefit from a technique that can produce analgesia effects without significant adverse effects on the respiratory function and ambulation.
Multimodal postoperative pain management strategies have been effectively used after weight loss surgeries (WLS) [6–8]. Opioid-sparing multimodal analgesia has been further validated for WLS patients and should become a standard of care to overcome the adverse effects of opioids and the complications associated with delayed ambulation [7–9].
Transversus abdominis plane (TAP) block, a locoregional nerve block, has emerged as a promising approach for provision of postoperative pain relief after abdominal incision [10–13] and the results of published studies show a remarkable reduction in postoperative opioid requirement in patients receiving TAP block.
We wished to study the analgesic potential of TAP block which produces dermatosensory block of the lower six thoracic and upper lumbar abdominal afferents [3, 5, 14], in this vulnerable group of patients. In our literature search, we did not come across any study, which has evaluated the possible benefits of this block in this patient population.
Regional and locoregional anesthetic techniques in the morbidly obese however have their limitations due to poorly defined landmarks leading to technical difficulties. Recently, ultrasound guidance (USG) has established its place as a technique to facilitate safe and accurate placement of local anesthetic, when technical difficulties are anticipated with anatomic landmark-based approaches [15, 16], leading to improved success rate of nerve blocks in obese patients.
We hypothesized that use of ultrasound-guided TAP (USG-TAP) block as a part of multimodal analgesia will minimize postoperative opioid requirement, expedite ambulation, and minimize adverse events in morbidly obese patients undergoing laparoscopic gastric bypass under general anesthesia. The primary outcome was requirement of Tramazac hydrochloride in first 24 h after surgery and the secondary outcomes were visual analogue scale (VAS) score (Richmond Agitation Sedation Scale; Table 1), time to ambulate, and any adverse events.
Patients and Methods
With approval of Institutional Ethics Committee of Max Super Speciality Hospital (a unit of DDF), New Delhi, a total of 100 patients with BMI >35 kg/m2, either sex, age more than 18 years, and scheduled for laparoscopic gastric bypass were recruited to undergo this randomized prospective double blind study. The study was registered with CTRI (CTRI 2011/12/002267).
Randomization followed a computer-generated allocation schedule (R version 2.12), using allocation concealment to prevent prior knowledge of treatment assignment. Numbers were assigned in strict chronological sequence and study participants were entered in sequence. Each study patient was allocated a unique randomization number on successful completion of screening, to be assigned to either control (no TAP, NT) or intervention group (ropivacaine TAP, RT). The randomization code was sent to the investigator (or designee) who decided the treatments according to the randomization code.
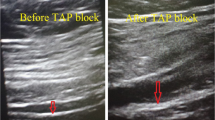
To minimize bias and confounders, the decision to accept or reject a patient was made using inclusion and exclusion criteria. Informed consent was obtained from participants prior to obtaining the randomization code. Independent anesthesiologists assessed the eligibility of the patient and obtained the randomization number and allocation of treatment type. The codes were revealed to the researchers once the recruitment, data collection, and analysis were completed. At the end of surgery after closure of ports, with the patient placed supine, a 15° tilt was achieved away from the side in which the block had to be performed. An assistant pulled the abdomen away towards the opposite side (Figs. 1 and 2).
The patients of group RT received bilateral TAP block using 20 ml of 0.375 % ropivacaine whereas patients of group NT received 20 ml of normal saline, on each side. The anesthesiologist drawing the drugs for TAP block was not be involved in the study. The patients, their anesthesiologists, and the staff providing postoperative care were blinded to group allocation. The block was performed using Sonosite M-Turbo machine, with linear array probe L38 (5–10 MHz).
Based on the preliminary data, we compared the usage of Tramazac hydrochloride (TMZ) in the group NT (0.52) and the same for group RT (0.20). We calculated that at least 45 subjects per group were required to achieve a power of 90 at 1 % level of significance. However to account for any losses, 100 patients were enrolled in the study.
Statistical Analysis
All data collected during the study was included in the data listings. Descriptive statistical methods were used to summarize the data from this study, with hypothesis testing performed for the outcome variable. The term “descriptive statistics” refers to number of subjects (n); mean, median, standard deviation (SD), minimum, and maximum for continuous data and frequencies; and percentages for categorical data.
Normally distributed data were presented as mean and standard deviation; non-normally distributed data as medians quartiles (interquartile range). Demographic data were analyzed using Student’s t test or Mann–Whitney U test as appropriate. Categorical data were analyzed using chi-square analysis or Fisher’s exact test where applicable.
All statistical testing was be two-sided and performed using a significance (alpha) level of 0.05. All statistical analyses were conducted with the STATA System, version 9.0.
Results
A total of 100 patients completed the study. All patients completed the study and there were no protocol violations. The patient characteristics and duration of anesthesia did not differ between the study (RT) and control (NT) groups.
The groups were comparable concerning age, weight, height, BMI, surgical methods, and operation time (Table 2). The application of USG-TAP block significantly reduced the total requirement of TMZ in the first 24 h of postoperative period, in the study group (Table 3). This was the maximum in the first and third postoperative hour.
Number of patients requiring TMZ required in the first, third, and sixth hour was found to be significantly more in the control group (Table 3). Even though the requirement at the sixth postoperative hour was lesser than the preceding hours, the prolonged sedative effect of the TMZ affected the time to ambulate. The mean TMZ required in 24 h postoperatively in the NT group was 48 mg and in the RT group was 9 mg; P = 0.000.
Postoperatively, the median VAS pain score of the study (RT) block group was consistently lower in the PACU at 1, 3, 6, 12, and 24 h at rest and on movement. In all patients, VAS remained less than 4 at the end of first postoperative day. This was associated with statistically significant intergroup difference in the sedation score in the first six postoperative hour (Tables 4 and 5).
Four patients in the control group required BIPAP support at the third hour in the PACU (Table 3). However, no adverse event related to the surgical procedure or the USG-TAP block was observed in any patient.
Time to ambulate was 6.3 ± 1.8 h in USG-TAP and 8 ± 1.8 h in the control groups; P < 0.001. We also assessed patient satisfaction scores at the end of first post-op day which was significantly more in the study group, P < 0.001, although this finding had no clinical relevance (Table 6).
Discussion
Our study demonstrates that with a slight modification in technique, successful ultrasound-guided TAP block could be performed in the morbidly obese patients. Our study also demonstrates its efficacy as part of multimodal analgesic technique in patients undergoing laparoscopic gastric bypass, with reduced opioid requirement, better pain score, decrease sedation, early ambulation, and greater patient satisfaction.
We could not find any study demonstrating its usefulness in morbidly patients undergoing laparoscopic Roux-en-Y anastomoses. The pain relief covering the most of the anterior abdominal wall has resulted in reduction of the analgesia requirements in the early postoperative period [9, 11, 16–21].
The innervation of the abdominal wall is derived from anterior divisions of spinal segmental nerves. These nerves run laterally between the transversus abdominis and internal oblique muscle layers of the abdominal wall. By introducing local anesthetics into the transversus abdominis plane through the triangle of Petit, it is possible to block the sensory nerves of the anterior abdominal wall before they pierce the musculature to innervate the abdomen.
Due to deep anatomic location of structures and nerves, the US beam travels a greater distance, leading to beam attenuation. Moreover, the image quality through fat may be poorer as the adipose tissue has a nonlinear relationship to frequency, whereas most biological tissues have linear relationship. In addition, the irregularly shaped adipose layers leads to uneven speed of sound causing phase aberration of the sound field. So that above the focus of the transducer, there is differing speeds of sound, leading to mismatch of acoustic impedance at the fat/muscle interfaces [22–24].
In obese patients, there is an increase in the number of reflective interfaces not only leading to more echoes but also decreasing the incident of sound available to penetrate deeper tissues, such as nerves, vessels, or other targeted structures. In our patients, with the modified technique, the visibility of the muscle layers could be improved by the 15° tilt away from the side in which block had to be performed. An assistant pulled the abdomen towards opposite side (Fig. 2) [25–28].
Conventionally, however, ultrasound-guided TAP block would require placement of probe laterally behind the midaxillary line between the iliac crest and the most inferior extent of the ribs and local anesthetic is deposited between these two muscle planes under direct vision. A 100-mm needle is passed anteriorly to come perpendicularly into the ultrasound beam and placed between transversus and internal oblique posterior to the midaxillary line.
Till date, complications related to USG-TAP have not been reported in this subpopulation. However, there has been a report of intrahepatic injection with the blind technique. Other complications that have been described include intraperitoneal injection, bowel hematoma, and femoral nerve palsy [29].
These patients are very prone to airway catastrophes following administration of opioids. We believe this group of patients would benefit from opioid-sparing effect of this nerve block. In the obese patient, the goal of postoperative pain management is provision of comfort, early mobilization, and improved respiratory function without causing sedation and respiratory compromise. Although several reviews covering anesthesia and analgesia for obese patients are published, these are mostly expert opinion and there is a paucity of evidence-based recommendations.
One limitation of the procedure was that a large number of assistants were required for successful performance of the block. We did not evaluate its effect on duration of hospital stay as the length of stay was expected to be affected by surgical variables as well and these were not considered for the analysis.
Conclusion
In conclusion, postoperative pain treatment with ultrasound-guided TAP block as a part of multimodal regimen in morbidly obese patients undergoing laparoscopic gastric bypass demonstrates reduction in opioid consumption, improved pain scores, reduced sedation, early ambulation, and most importantly greater patient satisfaction.
References
Araco A, Pooney SJ, Araco F, et al. The transversus abdominis plane (TAP) block for body contouring abdominoplasty with flank liposuction. Plast Reconstr Surg. 2010;125:181–2.
Araco A, Pooney SJ, Araco F, et al. Transversus abdominis plane (TAP) block reduces the analgesic requirements after abdominoplasty with flank liposuction. Ann Plast Surg. 2010;65:385–8.
Brolin RE. Gastric bypass. Surg Clin North Am. 2001;81:1077–95.
Byrne TK. Complications of surgery for obesity. Surg Clin North Am. 2001;81:1181–93.
McDonnell JG, O’Donnell BD, Tuite D, et al. The regional abdominal field infiltration (R.A.F.I.) technique: computerised and anatomical identification of a novel approach to the transversus abdominis neuro-vascular fascial plane. Anesthesiology. 2004;101:A899.
Govindarajan R, Ghosh B, Sathyamoorthy MK, et al. Efficacy of ketorolac in lieu of narcotics in the operative management of laparoscopic surgery for morbid obesity. Surg Obes Relat Dis. 2005;1:530–5.
Kamelgard JI, Kim KA, Atlas G. Combined ternovits and preventive analgesia in morbidly obese patients undergoing open gastric bypass: a pilot study. Surg Obes Relat Dis. 2005;1:12–6.
Madan AK, Ternovits CA, Speck KE, et al. Inpatient pain medication requirements after laparoscopic gastric bypass. Obes Surg. 2005;15:778–81.
McDonnell JG, O’Donnell B, Curley G, et al. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–7.
Carney J, Finnerty O, Rauf J, et al. Ipsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trial. Anesth Analg. 2010;111:998–1003.
Mukhtar K, Singh S. Transversus abdominis plane block for laparoscopic surgery. Br J Anaesth. 2009;102:143–4.
Petersen PL, Mathiesen O, Torup H, et al. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010;54:529–35.
Kuppuvelumani P, Jaradi H, Delilkan A. Abdominal nerve blockade for postoperative analgesia after caesarean section. Asia Oceania J Obstet Gynaecol. 1993;19:165–9.
Lloret Linares C, Decleves X, Oppert JM, et al. Pharmacology of morphine in obese patients: clinical implications. Clin Pharmacokinet. 2009;48:635–51.
Hayashi H, Ueyama H. Experience of ultrasound-guided popliteal sciatic nerve block and femoral nerve perineural catheter placement in a morbidly obese patient undergoing total knee arthroplasty. Masui. 2010;59:1260–2.
Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33:253–8.
French JL, McCullough J, Bachra P, et al. Transversus abdominis plane block for analgesia after caesarean section in a patient with an intracranial lesion. Int J Obstet Anesth. 2009;18:52–4.
Carney J, Mc Donnell JG, Ochana A, et al. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60.
El-Dawlatly AA, Turkistani A, Kettner SC, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7.
McDonnell JG, Curley G, Carney J, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106:186–91.
Tornero-Campello G. Transversus abdominis plane block should be compared with epidural for postoperative analgesia after abdominal surgery. Anesth Analg. 2007;105:281–2.
Saranteas T. Limitations in ultrasound imaging techniques in anesthesia: obesity and muscle atrophy? Anesth Analg. 2009;108:660–5.
Feigenbaum H. Physics and instrumentation. In: Feingenbaum H, Armstrong WF, Rayan T, editors. Feigenbaum’s echocardiography. Philadelphia: Lippincott William and Wilkins; 2005. p. 12–5.
Shmulewitz A, Teefey SA, Robinson BS. Factors affecting image quality and diagnostic efficacy in abdominal sonography: a prospective study of 140 patients. J Clin Ultrasound. 1993;21:623–30.
Browne JE, Watson AJ, Hoskins PR, et al. Investigation of the effect of subcutaneous fat on image quality performance of 2D conventional imaging and tissue harmonic. Imaging Ultrasound Med Biol. 2005;31:957–64.
Fiegler W, Felix R, Langer M, et al. Fat as a factor affecting resolution in diagnostic ultrasound: possibilities for improving picture quality. Eur J Radiol. 1985;5:304–9.
Reid SA. The transversus abdominis plane block. Anesth Analg. 2007;105:282–3.
Liu SS, Ngeow JE, Yadeau JT. Ultrasound-guided regional anesthesia and analgesia: a qualitative systematic review. Reg Anesth Pain Med. 2009;34:47–59.
Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med. 2008;33:274–5.
Conflict of Interest
The authors declare they, viz, Aparna Sinha (corresponding author), Lakshmi Jayaraman, and Dinesh Punhani have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sinha, A., Jayaraman, L. & Punhani, D. Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block After Laparoscopic Bariatric Surgery: a Double Blind, Randomized, Controlled Study. OBES SURG 23, 548–553 (2013). https://doi.org/10.1007/s11695-012-0819-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0819-5