Abstract
Background
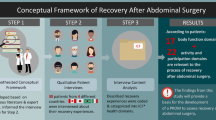
We initiated a research program to develop a novel patient-reported outcome measure (PROM) to assess postoperative recovery from the perspective of abdominal surgery patients. In light of FDA recommendations, the first stage of our program aimed to, based on previous literature and expert input, develop a hypothesized conceptual framework portraying the health domains that are potentially relevant to the process of recovery after abdominal surgery.
Methods
This study was conducted in three phases: (1) systematic review to identify PROMs with measurement properties appraised in the context of recovery after abdominal surgery, (2) content analysis to categorize the health domains covered by the PROMs according to the ICF, and (3) two-round Delphi study to gain expert input regarding which of these health domains are relevant to the process of recovery. Participants were experts in perioperative care identified through two major surgical societies (35 invited).
Results
The systematic review identified 19 PROMs covering 66 ICF domains. 23 experts (66%) participated in the Delphi process. After Round 2, experts agreed that 22 health domains (8 body functions, 14 activities and participation) are potentially relevant to the process of recovery after abdominal surgery. These domains were organized into a diagram, representing our hypothesized conceptual framework.
Conclusions
This hypothesized conceptual framework is an important first step in our research program and will be further refined based on in-depth qualitative interviews with patients. The sound methodological approach used to derive this framework may be valuable for studies aimed to develop PROMs according to FDA standards.
Visual Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
As with any major operation, patients undergoing abdominal surgery invariably experience a rapid health decline postoperatively, which is followed by a gradual return towards preoperative health [1]. Clinical manifestations of this decline include symptoms (e.g., postoperative pain and fatigue) and changes in functional status and psychological well-being. Length of postoperative recovery, defined as the time to return to preoperative health or ‘normal,’ varies depending on patient characteristics, extent of surgery and occurrence of postoperative complications [2,3,4]. Older patients, for example, may take 3–6 months to recover from a major abdominal operation and some never return to baseline functioning [3]. Prolonged or incomplete postoperative recovery not only increases healthcare costs but is also associated with substantial burden to patients and caregivers (e.g., time away from work, leisure, family and social activities) [5].
In line with the principles of patient-centered value-based care [6], there is growing interest in using patient-reported outcomes (PROs; reports of health coming directly from the patient without interpretation by others) to measure surgical recovery. Recent literature advocates that patient-reported outcome measures (PROMs) should be a key component of research to support patient-centered decision making and inform quality improvement initiatives [1, 7, 8]. If collected routinely in surgical practice, PROMs can also be a useful tool to guide clinician–patient communication about recovery expectations like the time to return to normal activities [9] and to promote self-management (e.g., empower patients to track their own recovery trajectory and identify complications) [10]. However, a recent systematic review of PROMs that have been used in this context found that they were not developed according to optimal scientific standards and have little evidence supporting their measurement properties [11]. To bridge this knowledge gap, we initiated a research program to develop a conceptually relevant and psychometrically sound PROM to measure recovery after abdominal surgery.
The field of PROMs has evolved in recent years after the US Department of Health and Human Services Food and Drug Administration (FDA) [12] published specific standards for regulatory approvals based on PRO data. The document emphasizes that PROMs should have strong evidence of ‘content validity’ (i.e., the extent to which the PROM reflects all aspects of the construct it is trying to measure) supported by a process involving (1) the development of a hypothesized conceptual framework based on literature review and expert opinion and (2) qualitative interviews with patients based on the domains identified, with subsequent adjustment of the conceptual framework as needed. The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) also supports the need to develop a hypothesized conceptual framework to outline the initial PROM structure and, most importantly, inform the subsequent stages of PRO development involving patient interviews [13, 14].
In this study, we developed a hypothesized conceptual framework portraying the health domains that, according to previous literature and expert opinion, are potentially relevant to the process of recovery after abdominal surgery. In line with FDA and ISOPOR guidelines, this is an essential step within the first phase of development of a novel PROM to measure postoperative recovery from the perspective of patients undergoing abdominal surgery.
Methods
The process of PROM development guiding our entire research program is outlined in Fig. 1. Development of the hypothesized conceptual framework was conducted in three steps: (1) systematic literature review to identify PROMs used in the context of recovery after abdominal surgery, (2) content analysis to categorize the health domains covered by the PROMs identified, and (3) Delphi study to gain expert input regarding which of these health domains are relevant to the process of recovery after abdominal surgery. Steps 1 and 2 were informed by preliminary data from a systematic review and content analysis conducted by our group and published elsewhere [11].
Step 1. Systematic literature review
PROMs previously appraised in the literature were identified using preliminary data from a systematic review assessing the measurement properties of existing PROMs used in the context of recovery after abdominal surgery [11]. To inform the development of this hypothesized conceptual framework, we analyzed PROMs identified from a literature search carried out from the 9th to 14th of October 2014 (in the previously published work, the search was updated in August 2016 [11]). Data extraction focused on the specific items (questions) included in each PROM. PROMs were excluded from the analysis if specific items could not be retrieved from the literature or internet search engines, or by contacting the authors. Further details about the search strategies, selection criteria, and data extraction methods have been reported elsewhere [11].
Step 2. Content analysis of the PROMs
To categorize the domains of health covered by each PROM identified in the literature, individual items included in each measure were linked to the World Health Organization’s International Classification of Functioning, Disability and Health (ICF) [15], which provides a common language for describing health and health-related states. In the present study, PRO items were linked to the ICF up to the two-level classification [16]. For example, a symptom such as abdominal pain, which is part of the body functions (B) chapter, is classified under ‘sensory functions and pain’ (B2; first-level classification) and ‘sensation of pain’ (B280; second-level classification). Further details about our process of ICF mapping have been previously reported [11]. At the end of this process, we compiled a list of ICF health domains covered by the PROMs identified.
Step 3. Delphi study
To finalize our hypothesized conceptual framework of recovery after abdominal surgery, we conducted a web-based Delphi study to gather expert input regarding the relevance of each health domain identified in the literature. The Delphi technique is a method of systematically surveying a group of experts to reach consensus opinion on a specific topic. It involves the anonymous completion of a series of questionnaires interspersed with summary and feedback derived from previous responses [17, 18]. We followed current recommendations for conducting and reporting Delphi studies in health research [19]. The Delphi study was approved by the McGill University Ethics Review Board (study # A03-E13-16B).
Panel nomination and recruitment
A multidisciplinary panel of clinicians with expertise in perioperative care and strategies to enhance recovery after abdominal surgery were invited to participate in this study. Potential participants were identified though major surgical organizations in North America (members of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) SMART Enhanced Recovery task force; n = 15) and Europe (board members, executive committee, and committee officers of the Enhanced Recovery After Surgery (ERAS) Society; n = 10). An invitation letter was sent via e-mail providing a brief outline of the project, its objectives, expected number of rounds and anticipated time commitment. As the study was conducted in English, ability to communicate in English was a prerequisite for participation. A positive response to the invitation letter served as informed consent.
Delphi process
The Delphi study was conducted in two rounds and surveys were responded to electronically via secure web-based survey software (QuestionPro, Survey Analytics LLC; Seattle, WA). Prior to each round, surveys were pilot tested among surgeons at our institution; changes in structure and word clarity were made in response to their feedback. At each round, a web link to the survey was distributed via e-mail and experts were given two weeks to respond. A reminder to complete the survey was sent at 1 week. An interval of 1 week between rounds was used to summarize the data and develop the next survey.
Round 1
Members of the expert panel were presented a list of all health domains covered by the PROMs identified in the systematic review, including the specific definition of each domain according to the ICF. They were asked to, based on their clinical experience and knowledge from previous literature, use a 4-point Likert scale (strongly disagree; disagree; agree; strongly agree) to rate their agreement as to whether each specific health domain is relevant to the process of recovery after abdominal surgery. A space was also provided for experts to present arguments and literature citations in support of their opinion or to suggest new domains to be added. As we were only interested in factors associated with functional recovery (i.e., ICF domains corresponding to body function, activity, and participation), domains related to environmental factors (e.g., satisfaction with care, support from health professionals) were not included in the survey.
Round 2
The summary of responses obtained in Round 1 (distribution of Likert scale scores and percentage agreement with each health domain), expert comments, and literature citations were incorporated into a second survey. During this round, experts were given the opportunity to view the group results and change their own ratings in light of their colleagues’ responses and arguments.
Data analyses
Distribution of Likert scale scores in Rounds 1 and 2 were extracted from the summary reports generated by the survey software (QuestionPro, Survey Analytics LLC; Seattle, WA). Domains of health rated as agree or strongly agree by ≥ 75% of the experts after Round 2 were deemed relevant to the process of recovery. These health domains were then organized into a structured diagram, representing our hypothesized conceptual framework of recovery after abdominal surgery.
Results
Systematic review
A total of 11,054 unique articles were identified by the search and 145 underwent full-text review. Of these, 117 were excluded. 28 studies fulfilled our selection criteria and were analyzed [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. These studies appraised a total of 19 different PROMs which are listed in Table 1. The number of items included in each PROM ranged from 5 to 40. A full description of the article screening process, details about the included studies (i.e., targeted population, sample characteristics, measurement properties assessed) and characteristics of the PROMs identified have been reported elsewhere [11].
Content analysis
A total of 66 two-level ICF domains were covered by the 19 PROMs (27 body functions, 35 activities and participation, 4 environmental factors). These domains were subsequently included in the Delphi study and are identified in the first column of Table 2. The ICF domains covered by each specific PROM have been previously reported [11]. The domains most commonly covered were ‘sensation of pain’ (n = 18), ‘energy and drive function’ (n = 15), ‘emotional functions’ (n = 12), ‘carrying out daily routine’ (n = 12), and ‘remunerative employment’ (n = 11). Several PROMs comprised items that are not classifiable by the ICF due to lack of precision (e.g., ‘how would you rate your general health?’) (n = 11). After the completion of ICF mapping, domains related to environmental factors were excluded from further analysis.
Delphi study
Of the 35 experts contacted, 23 (66%) responded to the invitation letter and participated in at least one round of the Delphi process. The rate of survey completion was 88% in Round 1 (n = 21) and 75% in Round 2 (n = 18). The expert panel comprised 20 surgeons (87%), one anesthesiologist (4%), one nurse (4%), and one physiotherapist (4%). Panel members were from four different countries (United States 61%, Canada 26%, Denmark 9%, and Spain 4%). The Round 1 survey was sent on March 10th, 2016. The Round 2 survey was sent on April 4th, 2016. Data collection for the study was completed within 6 weeks.
Table 2 shows the summary of responses obtained in Rounds 1 and 2. None of the participants suggested the inclusion of new domains between rounds. Likert scale scores distribution varied between rounds for all domains. Achievement of consensus criteria (≥ 75% agree or strongly agree) varied between rounds for three domains. The domains ‘attention functions’ and ‘respiration functions’ were only endorsed in Round 1 but not in Round 2; therefore, they were removed from the framework. The domain ‘intimate relationships’ was only endorsed and included in the framework after Round 2. None of the participants provided arguments to justify their change in opinion. At the completion of the last round, the panel agreed that 22 health domains (8 body functions, 14 activities, and participation) are relevant to the process of recovery after abdominal surgery. Figure 2 shows the hypothesized conceptual framework of recovery after abdominal surgery proposed in light of these results.
Discussion
This study outlines a hypothesized conceptual framework of recovery after abdominal surgery based on information from previous literature and expert opinion. This framework emphasizes the potential impact of abdominal surgery on body impairments, activity limitations, and participation restrictions, and based on this information, hypothesizes which health domains should be addressed in a PROM targeting the process of postoperative recovery after abdominal surgery. Our study provides an essential first step in a research program aimed to develop a novel recovery-specific PROM and will guide subsequent steps of PRO development, providing guidance for domains to address in patient interviews.
Although the development of an initial hypothesized conceptual framework is recommended by current guidelines for PRO development, these guidelines do not suggest specific methods to derive these frameworks [12,13,14]. This study provides a sound methodological approach to develop hypothesized conceptual frameworks using a systematic literature review to identify available evidence followed by a Delphi study to obtain input from experts. The Delphi method has been widely used in healthcare research as it provides several advantages over other methods to gather expert opinion (e.g., face-to-face meetings), such as allowing anonymous discussion without the influence of personal status, enabling alteration of personal views without embarrassment, and combining opinions from experts who are geographically dispersed [17,18,19]. Another strength of our study was that this hypothesized framework was built around the ICF, an international model that provides a unified, holistic and standardized language to classify and describe health and functioning [15]. Using the ICF language enables a broad understanding of our framework by clinicians and researchers from various disciplines and allows comparison with other frameworks, within and across health conditions.
Many PROMs have been developed and tested in the context of recovery after abdominal surgery. However, a recent systematic review by our group highlighted that there is limited evidence supporting their measurement properties [11]. Poor evidence of content validity was common, as few PROMs were supported by a conceptual framework of recovery. Therefore, it is unclear whether their domains and items are appropriate and comprehensive in relation to the intended measurement concept, use, and targeted population. The lack of a conceptual framework may, in part, explain the impressive variety of health domains covered by the different PROMs in the study [11]. Some PROMs covered domains that are potentially irrelevant to the process of recovery (e.g., temperament functions such as extraversion and agreeableness), while others failed to address domains that are likely to be important (e.g., gastrointestinal function). Previous research suggests that the latter issue is often observed when generic PROMs are used to measure postoperative recovery [e.g., Short-Form 36 (SF-36) and EUROQOL-5D (EQ-5D)] [48]. This finding supports that PRO measurement in abdominal surgery should be underpinned by a condition-specific framework.
Three previous studies specifically outlined conceptual frameworks of recovery after abdominal surgery [26, 29, 48], but the development process was poorly reported and did not follow current standards by FDA and ISPOR. Furthermore, results were somewhat conflicting; e.g., postoperative fatigue is a widely recognized symptom experience after abdominal surgery [49] that was included in some [48], but not all conceptual frameworks of recovery [26, 29]. The framework hypothesized in the current study resonates with domains that have been included in previous frameworks and will be further refined based on patient input. It is important to emphasize that the PROM to be developed will focus on recovery outcomes related to impairments (i.e., problems with body functions), activity limitations and participation restrictions; therefore, issues classified by the ICF under the umbrella ‘environmental factors’ were not included in the Delphi study surveys and will not be addressed in future steps of PRO development.
Some limitations of the study need to be acknowledged. Firstly, in light of the Delphi process timeline, only PROMs identified up to October 2014 were assessed in the present study. In an update search conducted in August 2016 another three relevant PROMs were identified (Cleveland Global Quality of Life, PROMIS 10 and WHO Disability Assessment Schedule 2.0) [11]; however, content analysis of these PROMs supports that they would not have contributed new relevant health domains to our framework [11]. Three authors of this paper (JF, LL and LF) are members of one of the surgical societies involved in this study (SAGES), hence, they also responded to the Delphi questionnaires. However, risk of ‘researcher bias’ (i.e., study results being intentionally or unintentionally skewed towards the authors’ opinion) was minimized by using an independent survey platform to collect data and produce summary reports. Another important limitation of our Delphi study was that our panel comprised mostly surgeons (87%). Consequently, the perspectives of clinicians from other disciplines may have been underrepresented. For example, our Delphi process missed the viewpoint of primary care clinicians (i.e., family physicians) and gastroenterologists who may have important insights about the long-term recovery of patients undergoing abdominal surgery. Lack of information regarding further participant characteristics (e.g., subspecialty of interest, years of experience in research and/or clinical practice) is another limitation. Also, the panel was only comprised of experts from Europe and North America. As perceptions of postoperative recovery may be sensitive to differences in culture and health-systems, this may limit the generalizability of the framework proposed in this study. This limitation will be addressed in the next steps of PROM development (Fig. 1) as this framework is refined through international qualitative interviews with patients from a wider variety of settings, which will also underpin the generation of items for the new PROM. This framework may also be further revised as we conduct cognitive interviews to ensure that domains and items are comprehensive and well understood by patients [13]. Modern psychometrical methods (Rasch measurement theory) will be used to optimize item selection and inform scoring algorithms, determining the viability of producing an overall ‘recovery score’ or the need to score different domains of recovery separately [50].
The lack of PROMs with sound content validity is a major knowledge gap that limits patient-centered research and quality improvement initiatives in abdominal surgery. In this study, we propose a hypothesized conceptual framework of recovery after abdominal surgery based on information from previous literature and expert input. This framework is an important first step in our research program and will be further refined in future stages of PRO development. The sound methodological approach used to derive this hypothesized framework may be valuable for studies aimed to develop PROMs according to FDA and ISPOR standards.
References
Lee L, Tran T, Mayo NE, Carli F, Feldman LS (2014) What does it really mean to “recover” from an operation? Surgery 155(2):211–216
Shulman MA, Myles PS, Chan MTV, McIlroy DR, Wallace S, Ponsford J (2015) Measurement of disability-free survival after surgery. J Am Soc Anesthesiol 122(3):524–536
Lawrence VA, Hazuda HP, Cornell JE, Pederson T, Bradshaw PT, Mulrow CD, Page CP (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 99(5):762–772
Tran TT, Kaneva P, Mayo NE, Fried GM, Feldman LS (2014) Short-stay surgery: what really happens after discharge? Surgery 156(1):20–27
Lee L, Mata J, Ghitulescu GA, Boutros M, Charlebois P, Stein B, Liberman AS, Fried GM, Morin N, Carli F, Latimer E, Feldman LS (2015) Cost-effectiveness of enhanced recovery versus conventional perioperative management for colorectal surgery. Ann Surg 262(6):1026–1033
Squitieri L, Bozic KJ, Pusic AL (2017) The role of patient-reported outcome measures in value-based payment reform. Value Health 20(6):834–836
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM, Feldman LS (2014) Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg 101(3):159–170
Feldman LS, Lee L, Fiore J (2015) What outcomes are important in the assessment of Enhanced Recovery After Surgery (ERAS) pathways? Can J Anaesth 62(2):120–130
van Vliet DC, van der Meij E, Bouwsma EV, Vonk Noordegraaf A, van den Heuvel B, Meijerink WJ, van Baal WM, Huirne JA, Anema JR (2016) A modified Delphi method toward multidisciplinary consensus on functional convalescence recommendations after abdominal surgery. Surg Endosc 30(12):5583–5595
Griggs CL, Schneider JC, Kazis LE, Ryan CM (2017) Patient-reported outcome measures: a stethoscope for the patient history. Ann Surg 265(6):1066–1067
Fiore JF Jr, Figueiredo S, Balvardi S, Lee L, Nauche B, Landry T, Mayo NE, Feldman LS (2017) How do we value postoperative recovery? A systematic review of the measurement properties of patient-reported outcomes after abdominal surgery. Ann Surg. https://doi.org/10.1097/SLA.0000000000002415
U.S. Department of Health and Human Services Food and Drug Administration (2009) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf. Accessed 7 Feb 2018
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, Ring L (2011) Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2—assessing respondent understanding. Value Health 14(8):978–988
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, Ring L (2011) Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 1—eliciting concepts for a new PRO instrument. Value Health 14(8):967–977
World Health Organization (2001) International classification of functioning, disability and health: ICF. WHO, Geneva
Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G (2005) ICF linking rules: an update based on lessons learned. J Rehabil Med 37(4):212–218
Jones J, Hunter D (1995) Consensus methods for medical and health services research. BMJ 311(7001):376–380
Powell C (2003) The Delphi technique: myths and realities. J Adv Nurs 41(4):376–382
Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C (2011) Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE 6(6):e20476
McKenna SP, Doward LC, Whalley D (1998) The development and testing of the well-being index for surgical patients (WISP). Qual Life Res 7(2):167–173
Myles PS, Hunt JO, Nightingale CE, Fletcher H, Beh T, Tanil D, Nagy A, Rubinstein A, Ponsford JL (1999) Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesth Analg 88(1):83–90
Kleinbeck SV (2000) Self-reported at-home postoperative recovery. Res Nurs Health 23(6):461–472
Myles PS, Weitkamp B, Jones K, Melick J, Hensen S (2000) Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth 84(1):11–15
Susilahti H, Suominen T, Leino-Kilpi H (2004) Recovery of Finnish short-stay surgery patients. Medsurg Nurs 13(5):326–335
Talamini MA, Stanfield CL, Chang DC, Wu AW (2004) The surgical recovery index—a novel tool for measuring the advantage of laparoscopic surgery in postoperative recovery. Surg Endosc (4):596–600
Urbach DR, Harnish JL, Long G (2005) Short-term health-related quality of life after abdominal surgery: a conceptual framework. Surg Innov 12(3):243–247
Urbach DR, Harnish JL, McIlroy JH, Streiner DL (2006) A measure of quality of life after abdominal surgery. Qual Life Res 15(6):1053–1061
Chan MT, Lo CC, Lok CK, Chan TW, Choi KC, Gin T (2008) Psychometric testing of the Chinese quality of recovery score. Anesth Analg 107(4):1189–1195
Hollenbeck BK, Dunn RL, Wolf JS Jr, Sanda MG, Wood DP, Gilbert SM, Weizer AZ, Montie JE, Wei JT (2008) Development and validation of the convalescence and recovery evaluation (CARE) for measuring quality of life after surgery. Qual Life Res 17(6):915–926
Kluivers KB, Hendriks JC, Mol BW, Bongers MY, Vierhout ME, Brölmann HA, de Vet HC (2008) Clinimetric properties of 3 instruments measuring postoperative recovery in a gynecologic surgical population. Surgery 144(1):12–21
Allvin R, Ehnfors M, Rawal N, Svensson E, Idvall E (2009) Development of a questionnaire to measure patient-reported postoperative recovery: content validity and intra-patient reliability. J Eval Clin Pract 15(3):411–419
Datta I, O’Connor B, Victor JC, Urbach DR, McLeod RS (2009) Abdominal Surgery Impact Scale (ASIS) is responsive in assessing outcome following IPAA. J Gastrointest Surg 13(4):687–694
Delaney CP, Lindsetmo RO, O’Brien-Ermlich B, Cheruvu VK, Laughinghouse M, Champagne B, Marderstein E, Obias V, Reynolds H, Debanne SM (2009) Validation of a novel postoperative quality-of-life scoring system. Am J Surg 197(3):382–385
Idvall E, Berg K, Unosson M, Brudin L, Nilsson U (2009) Assessment of recovery after day surgery using a modified version of Quality of Recovery-40. Acta Anesthesiol Scand 53(5):673–677
Wong J, Tong D, De Silva Y, Abrishami A, Chung F (2009) Development of the functional recovery index for ambulatory surgery and anesthesia. Anesthesiology 110(3):596–602
Balongo Garcia R, Espinosa Guzman E, Naranjo Rodriguez P, Tejada Gomez A, Rodriguez Perez M, Abreu Sanchez A (2010) Quality of life measurement in the postoperative period in general and gastrointestinal surgery. Cir Esp 88(3):158–166
Berg K, Idvall E, Nilsson U, Arestedt KF, Unosson M (2010) Psychometric evaluation of the post-discharge surgical recovery scale. J Eval Clin Pract 16(4):794–801
Allvin R, Svensson E, Rawal N, Ehnfors M, Kling AM, Idvall E (2011) The Postoperative Recovery Profile (PRP)—a multidimensional questionnaire for evaluation of recovery profiles. J Eval Clin Pract 17(2):236–243
Paddison JS, Sammour T, Kahokehr A, Zargar-Shoshtari K, Hill AG (2011) Development and validation of the Surgical Recovery Scale (SRS). J Surg Res 167(2):e85–e91
Tanaka Y, Wakita T, Fukuhara S, Nishiwada M, Inoue S, Kawaguchi M, Furuya H (2011) Validation of the Japanese version of the quality of recovery score QoR-40. J Anesth 25(4):509–515
Butler SF, Black RA, Techner L, Fernandez KC, Brooks D, Wood M, Katz N (2012) Development and validation of the post-operative recovery index for measuring quality of recovery after surgery. J Anesth Clin Res 3(12)
Keller DS, McGee MF, Goyal S, Nobel T, O’Brien Ermlich B, Cheruvu VK, Delany CP (2013) Construct validation and comparison of a novel postoperative quality-of-life metric and the Short Form-36 in colorectal surgery patients. Surgery 154(4):690–695 (discussion 695–696)
Lee L, Elfassy N, Li C, Latimer E, Liberman AS, Charlebois P, Stein B, Carli F, Fried GM, Feldman LS (2013) Valuing postoperative recovery: validation of the SF-6D health-state utility. J Surg Res 184(1):108–114
Stark PA, Myles PS, Burke JA (2013) Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology 118(6):1332–1340
Antonescu I, Carli F, Mayo NE, Feldman LS (2014) Validation of the SF-36 as a measure of post-operative recovery after colorectal surgery. Surg Endosc 28:434
Karaman S, Arici S, Dogru S, Karaman T, Tapar H, Kaya Z, Suren M, Gurler Balta M (2014) Validation of the Turkish version of the Quality of Recovery-40 questionnaire. Health Qual Life Outcomes 12:8
Lee L, Mata J, Augustin BR, Carli F, Morin N, Latimer E, Feldman LS (2014) A comparison of the validity of two indirect utility instruments as measures of postoperative recovery. J Surg Res 190(1):79–86
Lee L, Dumitra T, Fiore JF Jr, Mayo NE, Feldman LS (2015) How well are we measuring postoperative “recovery” after abdominal surgery? Qual Life Res 24(11):2583–2590
Zargar-Shoshtari K, Hill AG (2009) Postoperative fatigue: a review. World J Surg 33(4):738–747
Hobart JC, Cano SJ, Zajicek JP, Thompson AJ (2007) Rating scales as outcome measures for clinical trials in neurology: problems, solutions, and recommendations. Lancet Neurol 6(12):1094–1105
Acknowledgements
The Delphi panel in our study was comprised of the following experts who we would like to acknowledge for their time, commitment and valuable input: Dr Rajesh Aggarwal (McGill University, Montreal, Canada), Dr Thomas Aloia (University of Texas MD Anderson Cancer Center, Houston, USA), Dr Franco Carli (McGill University, Montreal, Canada), Dr Diana Diesen (UT Southwestern Medical Center, Dallas, USA), Dr Justin Dimick (University of Michigan, Ann Harbor, USA), Dr Liane Feldman (McGill University, Montreal, Canada), Dr Lorenzo Ferri (McGill University, Montreal, Canada), Dr Julio Fiore Jr (McGill University, Montreal, Canada), Dr Gerald Fried (McGill University, Montreal, Canada), Pascal Fuchshuber (University of California San Francisco, San Francisco, USA), Dr Alexis Grucela (NYU Langone Medical Center, New York, USA), Mr Dorthe Hjort (Rigshospitalet, Copenhagen, Denmark), Dr Rohan Joseph (Capital Regional Surgical Associates, Tallahassee, USA), Dr Henrik Kehlet (Rigshospitalet, Copenhagen, Denmark), Dr Deborah Keller (Colorectal Surgical Associates, Huston, USA), Dr Lawrence Lee (McGill University, Montreal, Canada), Dr Anne Lidor (University of Wisconsin, Madison, USA), Dr Benjamin Poulose (Vanderbilt University Medical Center, Nashville, USA), Dr José Ramírez (Hospital Clinico Universitario, Zaragoza, Spain), Dr Michele Riordon (The Methodist Hospital, Houston, USA), Dr Anthony Senagore (University of Texas Medical Branch at Galveston, Galveston, USA) Dr Vadim Sherman (Houston Methodist Hospital, Houston, USA), Dr Tonia Young-Fadok (Mayo Clinic College of Medicine, Phoenix, USA).
Funding
This work was supported by the 2015 SAGES Surgical Multimodal Accelerated Recovery Trajectory (SMART) Grant and by a non-competitive donation offered by SAGES. The Steinberg-Bernstein Centre for Minimally Invasive Surgery (McGill University Health Centre, Montreal, Canada) is supported in part by an unrestricted education grant from Medtronic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Julio F. Fiore Jr and Liane S. Feldman report a grant from SAGES during the conduct of the study. Lawrence Lee reports a grant from Johnson & Johnson outside the submitted work. Roshni Alam, Saba Balvardi, Bénédicte Nauche, Tara Landry, Sabrina M. Figueiredo, and Nancy E. Mayo have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Alam, R., Figueiredo, S.M., Balvardi, S. et al. Development of a patient-reported outcome measure of recovery after abdominal surgery: a hypothesized conceptual framework. Surg Endosc 32, 4874–4885 (2018). https://doi.org/10.1007/s00464-018-6242-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6242-9