Abstract
Purpose
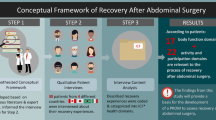
The content validity of patient-reported outcomes (PROs) commonly used to measure postoperative recovery is unknown. The objective of this study was to develop a conceptual framework for recovery after abdominal surgery and to analyze the content of PRO instruments against this conceptual framework.
Methods
Qualitative methods were used to develop a conceptual framework for recovery. Patients undergoing abdominal surgery and healthcare professionals were interviewed. Recovery-related concepts were identified using a thematic analysis, and concepts were then linked to the International Classification of Functioning, Disability and Health (ICF). The contents of eight PRO instruments that have been used to measure recovery were then examined using this conceptual framework.
Results
A total of 17 patients and 15 healthcare professionals were interviewed. A total of 22 important recovery-related concepts were identified and linked to the ICF. The four most important concepts were “Energy level,” “Sensation of pain,” “General physical endurance,” and “Carrying out daily routine.” The number of important recovery-related concepts covered by each instrument ranged from 1 to 22 (mean 7.3 concepts). The SF36 (n = 22), European Organization for the Treatment and Research of Cancer Quality-of-Life Questionnaire-C30 (n = 20), and the Gastrointestinal Quality-of-Life Index (n = 19) covered the greatest number of important recovery concepts. No instrument covered all of the important concepts.
Conclusions
The comparison of the contents of PRO instruments commonly used to measure postoperative recovery after abdominal surgery demonstrated major gaps in the representation of concepts that are important to patients and healthcare professionals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative recovery is a complex construct involving dimensions of physical, emotional and social health [1]. Many innovations in abdominal surgery such as enhanced recovery pathways (ERPs) and laparoscopic surgery aim to improve recovery, but much of the data on the effectiveness of these interventions have focused on traditional clinical and audit measures (e.g., postoperative complications and hospital length of stay) [2]. Although these measures are of interest for clinicians, they do not capture the complexity of the construct “recovery” or the perspective of patients, i.e., those who are actually recovering. Taking this into account, recent literature has advocated that recovery be measured using patient-reported outcomes [1–4] (PROs; any report of the status of a patients’ health condition that comes directly from the patient [5]). Using PROs in the context of recovery provides the opportunity to monitor perioperative health status across various domains of health, engaging patients as the key stakeholders in the postoperative recovery process.
Accumulated evidence indicates that ERPs and laparoscopic surgery improve clinical outcomes postoperatively; however, initial studies evaluating the effect of these interventions on recovery in terms of PROs had equivocal results [6, 7]. It is unclear whether these results are related to issues regarding the methodological quality and power of the exiting studies [7, 8] or whether, in fact, the clinical benefit of ERP and laparoscopic surgery does not translate into improvement in PROs. A potential methodological limitation of the existing literature is that PRO data were generally obtained using generic health-related quality-of-life (HRQL) questionnaires [2, 6] which were not previously tested for content validity in the context of postoperative recovery. Therefore, it is unknown whether the content of these questionnaires reflects concepts that are relevant for patients recovering from abdominal surgery.
The objectives of this study were (1) to develop a conceptual framework of postoperative recovery after abdominal surgery from the standpoint of patients and healthcare professionals and (2) to compare the content of PRO instruments commonly used in the context of postoperative recovery against this conceptual framework.
Methods
This study was performed in two parts. In the first part, we used qualitative methods to develop a conceptual framework for postoperative recovery after abdominal surgery. In the second part, we used this framework to analyze the content of PRO instruments that have been used to measure recovery. The local ethics review board approved the study protocol (11-736-SDR).
Part I—Qualitative study methods
To develop our conceptual framework, detailed one-on-one semi-structured interviews were conducted to identify relevant concepts related to postoperative recovery from the perspective of patients and healthcare professionals. Adult subjects who had undergone elective abdominal surgery at a single university-affiliated institution from September 2013 onwards were eligible for this study. Potential subjects were identified from the operating room database and were contacted by telephone three to four weeks after surgery to determine eligibility and obtain consent. Subjects were excluded if they did not speak English or French or if they had preexisting neuropsychiatric conditions that prevented the conduct of the interview. We also interviewed healthcare professionals (including surgeons, anesthesiologists, and nurses) from multiple North American institutions with an interest in ERAS and/or postoperative recovery (excluding the authors). Most of these professionals were recruited during an international workshop (Implementation of ERAS for Colorectal Resection: Theory into Practice, Montreal, QC, Canada, November 23, 2013).
Detailed one-on-one semi-structured interviews were conducted by a single author (L.L.), who was not involved in the medical care of the participating patients, either by phone or in person (according to the participant’s preference). Patients were asked about their recovery process since discharge from hospital, focusing on disabilities or any setbacks that they experienced. Patients were also asked whether they felt 100 % recovered and their reasons if they felt otherwise. Healthcare professionals were asked about what they considered to be important elements for postoperative recovery, focusing on recovery after discharge from hospital. All interviews were recorded and transcribed verbatim and then analyzed using the grounded theory approach [9, 10]. The goal of the grounded theory approach is to establish the conceptual framework of a specific social phenomenon through inductive analyses. Two authors (L.L. and T. D.) independently examined the transcripts line by line, and important themes (concepts) were identified. Interviews were conducted until thematic saturation was achieved [10].
The recovery-related concepts identified in the interviews were linked to the World Health Organization’s International Classification of Functioning, Disability and Health (ICF), a universal framework for describing the health and functioning of an individual [11]. In the ICF, function and disability are organized into three main components, body functions and structures, activities and participation, and contextual factors, which are arranged in a hierarchical manner in their most granular form. ICF category codes are preceded by the letters “b” for body functions, “s” for structures, “d” for activities or participation, and “e” for environmental factors, followed by the chapter number (one digit), followed by the second level (two digits), and the third and fourth level (one digit each), representing the level of detail captured. For example, d450 is the second level category code for walking, while d4501 is the third level category code for walking short distances. The ICF was designed to document and organize health in a standardized terminology, thereby facilitating communication and comparisons of health in different disciplines. Therefore, it can be used to evaluate the content validity of PRO instruments [12]. Indeed, previous studies have used the ICF to evaluate the contents of PROs for a wide ranges of health conditions, including osteoarthritis [13], stroke [14], and head and neck cancer [15].
We linked recovery-related concepts to the ICF, based on established linking rules [16, 17]. First, each item was examined for meaningful items, which were then linked to the most specific ICF category. For example, the following statement from a patient participant, “I am usually someone who is physically active, but now I barely have enough endurance to walk for more than 15 min,” is linked to ICF categories “d9201 Sports,” “d4500 Walking short distances,” and “b4550 General physical endurance.” Concepts that are not categorized in the ICF are linked as “not covered,” and those that are too imprecise are linked as “not defined” (e.g., general health). This analysis was performed independently by two authors (L.L. and T. D.). Disagreements were resolved by consensus or by a third reviewer (L.S.F).
Part II—HRQOL instrument content analysis
In the second part of this study, we performed a content analysis of PRO instruments commonly used to evaluate recovery using the ICF-linked recovery concepts identified through qualitative methods. The set of PRO instruments were previously identified in a systematic review of outcome measures used in studies comparing ERPs and conventional care in abdominal surgery [2]. These instruments included the Spitzer Quality-of-Life Index [18], Quality of Recovery score [19], Cleveland Clinic Global Quality-of-Life questionnaire [20], SF36 [21], Gastrointestinal Quality-of-Life Index [22], EQ-5D [23], European Organization for Research and Treatment of Cancer (EORTC) Quality-of-Life Questionnaire-C30 [24], and the Surgical Recovery score [25]. This analysis was also performed independently by two authors (L.L. and T. D.), and disagreements were resolved by consensus or by a third reviewer (L.S.F.).
Individual items of each instrument were linked to the ICF using the linking rules previously described. For example, item 3a on the SF36, “Does your health limit you in vigorous activities, such as running, lifting heavy objects, or participating in strenuous sports?”, is linked to ICF categories “d4552 Running,” “d4300 Lifting,” and “d9201 Sports.” Content density (number of meaningful concepts/total number of items) and content diversity (number of ICF categories/number of meaningful concepts) were calculated for each instrument [14]. A content density value of one signifies that each item of an instrument contains only one meaningful concept. Higher values represent that more meaningful concepts are contained within a single item on average and vice versa. A content diversity value of one signifies that each ICF category corresponds to a single meaningful concept. A value closer to zero represents that each ICF category is represented through multiple concepts (i.e., in more detail) and vice versa. In addition, the number and the specific representation of important recovery-related concepts covered by each instrument were also evaluated.
Results
A total of seventeen patients and fifteen healthcare professionals were interviewed until thematic saturation. Patient characteristics are demonstrated in Table 1. Only a minority of patients experienced a postoperative complication, all of which were considered minor (Clavien grade I or II [26]). Among healthcare professionals, eleven surgeons (five colorectal, three minimally invasive, one hepatopancreaticobiliary, one urology, and one surgical oncology specialists), two anesthesiologists, and two nurses participated.
A total of 34 concepts were identified through patient interviews and 38 through healthcare professional interviews. Each concept was identified in a median of 3 (IQR 1–6) patient interviews, and a median of 4 (IQR 2–5) healthcare professional interviews. Important concepts were defined as those concepts that were identified in at least three patient interviews and four healthcare professional interviews (corresponding to the median number of times that each concept was identified). A total of were 22 important concepts were defined as important (Table 2), of which ten were linked to the ICF category body functions and twelve to activities and participation. There were no concepts linked to body structures or environmental factors. Table 2 also demonstrates the comparison of important concepts for patients and healthcare professionals. There were nine concepts that exhibited discordance between patients and healthcare professionals. In addition, there were eight concepts that were not classifiable by the ICF, and healthcare professionals expressed them all. Important non-classifiable concepts included postoperative complications (n = 5), “overall well-being” (n = 5), and preoperative baseline status (n = 5). However, given that these concepts were not considered as health-related functions or disabilities as defined by the ICF, they were excluded from the content analysis.
ICF content analyses of the PRO instruments are summarized in Table 3. The Cleveland Clinic Global Quality-of-Life questionnaire had the fewest items (n = 3), and the SF36 had the most (n = 36). The mean number of meaningful concepts that were identified in each instrument was 26.1 (range 3–54), although only a mean of 14.8 different ICF categories was covered for each instrument. The mean content density was 1.6 meaningful concepts per item. Instruments with fewer items (except the Cleveland Clinic Global Quality-of-Life questionnaire) generally had a higher content density and vice versa. The SF36, EORTC Quality-of-Life Questionnaire-C30, and the Gastrointestinal Quality-of-Life Index had the lowest content diversity indexes, suggesting that each ICF category was covered many times. For example, the SF36 contains three items that are linked to “d450 Walking”: Does your health limit you in 3 g) walking more than a mile; 3 h) walking several blocks; and 3i) walking one block? Table 4 demonstrates which important recovery concepts are represented in each instrument. Each instrument covered a mean of 7.3 important recovery concepts, with the EORTC Quality-of-Life Questionnaire-C30 covering the most concepts (n = 18), and the Cleveland Clinic Global Quality-of-Life questionnaire covering the fewest (n = 1). Three concepts, “b1300 Energy level,” “b280 Sensation of pain,” and “d230 Carrying out daily routine,” were the most commonly covered. Two concepts, “b1102 Quality of consciousness” and “d660 Assisting others,” were not covered by any instrument. The ratio of relevant items (i.e., items covering the important recovery concepts) to total number of items was poor (Table 4).
Discussion
The use of PRO instruments is becoming increasingly important in the evaluation of new and existing health technologies. However, it is essential that these instruments reflect the underlying construct under investigation. Generic HRQOL are commonly used to measure recovery after abdominal surgery, but these instruments may cover a wide range of concepts that may not be relevant, or omit important concepts for patients recovering from surgery. Content analysis of these instruments is an essential first step in choosing an appropriate one [27]. This study identified important concepts relevant for postoperative recovery through qualitative methods, and performed content analyses of PROs that are commonly used in studies evaluating interventions aimed to improve recovery, using the ICF framework.
The qualitative analysis identified 22 important recovery concepts. Of these, the most commonly reported by patients and healthcare professionals alike were “b1300 Energy level,” “b280 Sensation of pain,” “4550 General physical endurance,” and “d230 Carrying out daily routine.” The majority of the instruments analyzed in this study covered these concepts, with the exception of “d4550 General physical endurance,” which was only covered by the Gastrointestinal Quality-of-Life Index and the Surgical Recovery score, two instruments that were more specifically developed for abdominal surgery. Interestingly, concepts related to psychological state were not mentioned in the interviews. This suggests that, from the point of view of the participating patients and healthcare professionals, psychological issues after surgery (e.g., anxiety and depression) are either uncommon or not relevant to the postoperative recovery process. There were no concepts linked to body structures, suggesting that, to the participants, postoperative recovery is related to functional rather than to anatomical charges to body organs. No concepts were linked to environmental factors, possibly because these are not expected to be influenced by the surgery.
A potential criticism of our conceptual framework of postoperative recovery is that the concept of “postoperative complications” was not included. For many, it may be counterintuitive to exclude complications from any measurement of postoperative recovery because of their impact [28]. Rather, complications are indirectly included, as their impact on patients is reflected. For example, a patient who experienced a surgical site infection may not be able to return to usual activities as quickly as a patient without the same complications. Certainly, valid patient-reported outcome measures should be able to discriminate between patients with and without complications, even if the occurrence of a postoperative complication is not specifically included [1].
The results of the qualitative process identified important concepts in keeping with previous studies [29, 30]. Urbach et al. [29] interviewed inpatients that had undergone abdominal surgery a mean of four days prior. At this timepoint, the majority of the identified themes related to symptoms and basic bodily functions, compared with the present study, which reported that patients largely cited impairments in activities and participation at four weeks after surgery. Similarly, Allvin et al. [30] also reported that the core experiences of postoperative recovery could be summarized into unpleasant physical symptoms, disturbances in emotional well-being, regaining functions, and reestablishing activities. No previous studies have linked their conceptual frameworks to the ICF.
Based on the number of important recovery concepts represented, the EORTC Quality-of-Life Questionnaire-C30 would appear to be the most appropriate instrument to measure postoperative recovery. However, other indices must also be taken into account. A higher content density, that is, more than one meaningful concept per item, may potentially cause problems for item interpretation [31]. For example, item 5 of the EORTC Quality-of-Life Questionnaire-C30, “Do you need help with eating, dressing, washing yourself or using the toilet?” contains four different meaningful concepts. It may be difficult for respondents to select the appropriate response if they have disability in only one of the four meaningful concepts. Only the Cleveland Clinic Global Quality-of-Life questionnaire had a content density value of one; however, this instrument contained only three items and covered a single important recovery concept. In particular, instruments with fewer items tended to contain a higher number of meaningful concepts, but even instruments with more items had more than one concept per item, on average. Furthermore, the ratio of relevant items (the items containing the important recovery concepts) to total items tended to be low, suggesting that many items of each questionnaire measured concepts that were not considered to be important for postoperative recovery. These findings further increase measurement “noise,” potentially obscuring the true effects of the interventions to improve postoperative recovery.
Content analysis is among the first steps in selecting the appropriate instrument to measure a certain construct. However, it must be recognized that the present study did not assess other measurement properties of these instruments (e.g., responsiveness or construct validity). Kluivers et al. [32] systematically identified twelve recovery-related PRO instruments and concluded that none were fully validated for the construct of postoperative recovery. The Quality of Recovery score was the sole instrument to be included in the present study as well as Kluivers and colleagues’ systematic review and satisfied only two of their eight quality criteria. This questionnaire was developed, however, to assess early, in-hospital recovery rather than longer-term recovery.
Given these results of the present study, it is not surprising that only a few studies comparing ERPs to conventional care in abdominal surgery have demonstrated differences in patient-reported postdischarge recovery. At the present time, it is unclear whether there is no difference in postoperative recovery between ERP and conventional care or whether inappropriate instruments were used to measure recovery, thus obscuring any potential true effects. These results may also be generalizable to other interventions advocated to improve recovery such as laparoscopic surgery. A systematic review of studies comparing laparoscopic versus open colectomy reported that few studies reported a difference in short-term HRQOL [8]. In this review, the most commonly used instruments were the EORTC Quality-of-Life Questionnaire-C30, SF36, and the Gastrointestinal Quality-of-Life Index. The content validity of all these instruments was appraised in our analysis.
This study should be interpreted in view of several limitations. The patient population that was interviewed was enrolled from a single institution in a large urban community, and a majority were patients undergoing colorectal surgery. This may limit the generalizability of our results to different settings or to other types of abdominal surgery. The incidence of postoperative complications in participating patients was also low, and none were considered severe. This may have resulted in more favorable postoperative experiences. We also did not evaluate the socioeconomic or baseline functional status of the participating patients, which may also affect their recovery experience. It is possible that relevant PRO instruments previously used in the context of recovery were omitted because we included only those identified in the ERPs literature. Finally, the important recovery concepts identified in this study may not be exhaustive, as formal development methodology of ICF core sets were not followed. However, our methods have the advantage of including the patients’ perspectives. The inclusion of patient input is an essential component if these concepts are to be used to develop new PROs, as recommended by the FDA’s guidance [33].
In light of the findings of the current study, several recommendations for future studies can be made. The measurement properties of remaining instruments reviewed in the present study, as well as new recovery-specific instruments, should be thoroughly investigated [34]. In particular, modern psychometric methods, such as Rasch measurement theory, should be utilized to assess the validity of these instruments [35]. In the absence of a psychometrically sound instrument that represents the important recovery-related concepts, a PRO measure of postoperative recovery should be developed, according to the accepted guidelines [33].
In summary, this study identified relevant concepts related to postoperative recovery and classified them using the ICF. The comparison of the contents of PRO instruments commonly used in the context of recovery demonstrated major gaps in the representation of important recovery-related concepts. These findings may serve as an explanation for the equivocal results observed in studies that used PROs instruments to evaluate strategies aimed to improve recovery. Future studies may use the conceptual framework developed in this study to evaluate the contents of other instruments or to develop a new instrument that would comprehensively represent all of the important concepts. Until such an instrument is identified or developed, the question of whether innovations advocated to improve recovery actually do cannot be answered.
References
Lee, L., Tran, T., Mayo, N. E., Carli, F., & Feldman, L. S. (2014). What does it really mean to “recover” from an operation? Surgery, 155(2), 211–216.
Neville, A., Lee, L., Antonescu, I., Mayo, N. E., Vassiliou, M. C., Fried, G. M., & Feldman, L. S. (2014). Systematic review of outcomes used to evaluate enhanced recovery after surgery. British Journal of Surgery, 101(3), 159–171.
Miller, T. E., Thacker, J. K., White, W. D., Mantyh, C., Migaly, J., Jin, J., et al. (2014). Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesthesia and Analgesia, 118(5), 1052–1061.
Ljungqvist, O., & Rasmussen, L. S. (2014). Recovery after anaesthesia and surgery. Acta Anaesthesiologica Scandinavica, 58(6), 639–641.
Patrick, D. L., Burke, L. B., Powers, J. H., Scott, J. A., Rock, E. P., Dawisha, S., et al. (2007). Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health, 10(Suppl 2), S125–S137.
Dowson, H. M., Cowie, A. S., Ballard, K., Gage, H., & Rockall, T. A. (2008). Systematic review of quality of life following laparoscopic and open colorectal surgery. Colorectal Disease, 10(8), 757–768.
Khan, S., Wilson, T., Ahmed, J., Owais, A., & MacFie, J. (2010). Quality of life and patient satisfaction with enhanced recovery protocols. Colorectal Disease, 12(12), 1175–1182.
Bartels, S. A., Vlug, M. S., Ubbink, D. T., & Bemelman, W. A. (2010). Quality of life after laparoscopic and open colorectal surgery: A systematic review. World Journal of Gastroenterology, 16(40), 5035–5041.
Strauss, A. L. (1987). Qualitative analysis for social scientists. New York: Cambridge University Press.
Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for qualitative research. New York: Aldine Press.
World Health Organization. (2001). International classification of functioning, disability and health: ICF. Geneva: WHO.
Stucki, G., Cieza, A., Ewert, T., Kostanjsek, N., Chatterji, S., & Ustun, T. B. (2002). Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disability and Rehabilitation, 24(5), 281–282.
Weigl, M., Cieza, A., Harder, M., Geyh, S., Amann, E., Kostanjsek, N., & Stucki, G. (2003). Linking osteoarthritis-specific health-status measures to the international classification of functioning, disability, and health (ICF). Osteoarthritis Cartilage, 11(7), 519–523.
Geyh, S., Cieza, A., Kollerits, B., Grimby, G., & Stucki, G. (2007). Content comparison of health-related quality of life measures used in stroke based on the international classification of functioning, disability and health (ICF): A systematic review. Quality of Life Research, 16(5), 833–851.
Tschiesner, U., Rogers, S. N., Harreus, U., Berghaus, A., & Cieza, A. (2008). Content comparison of quality of life questionnaires used in head and neck cancer based on the international classification of functioning, disability and health: A systematic review. European Archives of Oto-Rhino-Laryngology, 265(6), 627–637.
Cieza, A., Brockow, T., Ewert, T., Amman, E., Kollerits, B., Chatterji, S., et al. (2002). Linking health-status measurements to the international classification of functioning, disability and health. Journal of Rehabilitation Medicine, 34(5), 205–210.
Cieza, A., Geyh, S., Chatterji, S., Kostanjsek, N., Ustun, B., & Stucki, G. (2005). ICF linking rules: An update based on lessons learned. Journal of Rehabilitation Medicine, 37(4), 212–218.
Spitzer, W. O., Dobson, A. J., Hall, J., Chesterman, E., Levi, J., Shepherd, R., et al. (1981). Measuring the quality of life of cancer patients: A concise QL-index for use by physicians. Journal of Chronic Diseases, 34(12), 585–597.
Myles, P. S., Hunt, J. O., Nightingale, C. E., Fletcher, H., Beh, T., Tanil, D., et al. (1999). Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesthesia and Analgesia, 88(1), 83–90.
Fazio, V. W., O’Riordain, M. G., Lavery, I. C., Church, J. M., Lau, P., Strong, S. A., & Hull, T. (1999). Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Annals of Surgery, 230(4), 575–584.
Ware, J. E, Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Eypasch, E., Williams, J. I., Wood-Dauphinee, S., Ure, B. M., Schmulling, C., Neugebauer, E., & Troidl, H. (1995). Gastrointestinal quality of life index: Development, validation and application of a new instrument. British Journal of Surgery, 82(2), 216–222.
EuroQol Group. (1990). EuroQol—A new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European organization for research and treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365–376.
Paddison, J. S., Sammour, T., Kahokehr, A., Zargar-Shoshtari, K., & Hill, A. G. (2011). Development and validation of the surgical recovery scale (SRS). Journal of Surgical Research, 167(2), e85–e91.
Dindo, D., Demartines, N., & Clavien, P. A. (2004). Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery, 240(2), 205–213.
Rothman, M., Burke, L., Erickson, P., Leidy, N. K., Patrick, D. L., & Petrie, C. D. (2009). Use of existing patient-reported outcome (PRO) instruments and their modification: The ISPOR good research practices for evaluating and documenting content validity for the use of existing instruments and their modification PRO task force report. Value Health, 12(8), 1075–1083.
Lee, L., Elfassy, N., Li, C., Latimer, E., Liberman, A. S., Charlebois, P., et al. (2013). Valuing postoperative recovery: Validation of the SF-6D health-state utility. Journal of Surgical Research, 184(1), 108–114.
Urbach, D. R., Harnish, J. L., & Long, G. (2005). Short-term health-related quality of life after abdominal surgery: A conceptual framework. Surgical Innovation, 12(3), 243–247.
Allvin, R., Berg, K., Idvall, E., & Nilsson, U. (2007). Postoperative recovery: A concept analysis. Journal of Advanced Nursing, 57(5), 552–558.
Mayo, N. E., Moriello, C., Asano, M., van der Spuy, S., & Finch, L. (2011). The extent to which common health-related quality of life indices capture constructs beyond symptoms and function. Quality of Life Research, 20(5), 621–627.
Kluivers, K. B., Riphagen, I., Vierhout, M. E., Brolmann, H. A., & de Vet, H. C. (2008). Systematic review on recovery specific quality-of-life instruments. Surgery, 143(2), 206–215.
Food and Drug Administration. (2009). Guidance for industry—Patient-reported outcome measures: Use in medical product development to support labeling claims. U.S. Department of Health and Human Services. http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf. Accessed October 11, 2013.
Lee, L., Mata, J., Augustin, B. R., Carli, F., Morin, N., Latimer, E., & Feldman, L. S. (2014). A comparison of the validity of two indirect utility instruments as measures of postoperative recovery. Journal of Surgical Research, 190(1), 79–86.
Hobart, J. C., Cano, S. J., Zajicek, J. P., & Thompson, A. J. (2007). Rating scales as outcome measures for clinical trials in neurology: Problems, solutions, and recommendations. Lancet Neurology, 6(12), 1094–1105.
Acknowledgments
LL is supported by the Quebec Health Sciences Research Fund (FRQS) and the Fast Foundation.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, L., Dumitra, T., Fiore, J.F. et al. How well are we measuring postoperative “recovery” after abdominal surgery?. Qual Life Res 24, 2583–2590 (2015). https://doi.org/10.1007/s11136-015-1008-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1008-5