Abstract
Background
Postoperative fatigue (POF) significantly impacts well-being after major surgery. However, this topic has received little emphasis.
Methods
We conducted a comprehensive search on major databases with a focus on studies relevant to assessment and etiology of POF.
Results
POF has been measured by a number of different and inadequate instruments. It has a complicated etiology, with a number of biological and psychological factors implicated. However, the etiology of this condition has not been fully explained.
Conclusions
The role of local inflammation in the development of POF requires further research. Multimodal interventions should be conducted with a focus on addressing various factors that contribute to the development and progression of POF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of a feeling of debilitating tiredness, loss of energy, or malaise is a well-described medical complaint known as “fatigue.” Several medical and psychological conditions, such as multiple sclerosis, chronic fatigue syndrome, sleep apnea, glucocorticoid withdrawal syndrome, and depression, have been associated with fatigue. Additionally, as well as being an indicator of disease, fatigue also may result from medical therapy, such as treatment for cancer with radio- or chemotherapy [1–4]. Fatigue also is a well-recognized condition after surgery, and this “postoperative fatigue” can be present in patients for up to a month after abdominal operations and continues to resolve for up to 3 months after uncomplicated gastrointestinal surgery [5, 6].
In this review of postoperative fatigue (POF), we discuss its significance, objective and subjective assessment tools, and review possible etiological factors that may influence POF. This is not a systematic review on this topic but an up-to-date overview of POF.
Methods
A database search was conducted of MEDLINE, Embase, PsychInfo, PubMed, and the Cochrane Collaboration library from inception to December 2006 for English-language papers containing surgery-related MeSH or free-text terms and combined with fatigue-related MeSH or free text. Papers were reviewed with respect to relevance to this article, in particular focusing on subjective and objective assessment as well as etiology. The reference sections of all reviewed papers were checked for further relevant studies.
Why is POF important?
Postoperative fatigue is an unpleasant and distressing symptom and frequently has a major impact on the patient’s quality of life [7]. Not surprisingly, POF may be one of the main complaints after surgery and may last much longer than pain. It prevents return to normal function and activity, including housekeeping, family, and child care. Fatigue contributes substantially to feelings of frustration, depression, or hopelessness and to difficulty concentrating or being attentive. Some patients describe fatigue as a “change in emotional state” [8].
POF may prevent otherwise fit patients from returning to work. Large numbers of patients report loss of wages as a result of this prolonged surgical recovery time. Patients miss an average of 6 weeks of work after uncomplicated abdominal operations. It also has a similar impact on caregivers [8, 9].
A higher degree of POF is followed by worse emotional, physical, and functional outcomes [10]. POF may be a source of increased costs to the health service, with patients who suffer from fatigue placing significantly greater demands on their primary health care teams compared with those who feel less tired [7–9].
Despite the severe impact of POF on overall recovery, POF has been largely ignored as an objective for prevention or treatment after surgery. It is obvious that POF has major consequences on patients’ well being, and thus there is considerable rationale for a proper understanding of the etiology, pathophysiology, prevention, and treatment of this condition.
Assessment of fatigue
A significant factor that has hindered understanding of POF has been that there is no “gold standard” for fatigue assessment, and clear objective correlates for fatigue have not been identified.
Questionnaires, in particular, have been shown to be an effective tool for measuring subjective feelings of fatigue, and there are a number of different instruments that have been developed for this purpose (Table 1). These range from single-item scales of intensity, such as Visual Analogue Scales, to multidimensional measures. Variations between these scales are based on theoretical classifications of fatigue into different dimensions. Examples include assigning different mental and physical aspects to fatigue or assessing fatigue on the basis of severity, circumstances, consequences, and responsiveness to rest/sleep [11, 12].
When investigating POF, the most commonly used scales are Christensen’s Visual Analogue Scales (VAS) and the fatigue-inertia and vigor-activity subscales of the Profile of Mood States (POMS).
Christensen’s VAS was first described in 1982 and since has been used widely to measure POF. This has been a valuable instrument in POF research because it is simple and takes little time and effort to complete. However, it is not able to provide a comprehensive expression of patients’ fatigue experience because it does not recognize that there are different physical, mental, and behavioral components to POF [12, 13].
The Profile of Mood States (POMS; Educational and Industrial Testing Service, San Diego) consists of a checklist of 58 adjectives that describe different mood states. The descriptive terms are related to four major states: Fatigue-Inertia, Tension-Anxiety, Depression-Dejection, and Anger-Hostility. The POMS was designed specifically to assess mood, not POF, and although the subscales of the POMS contain more than single items (unlike Christensen’s VAS), the range of these scales is too narrow to be an effective tool for research related to POF [14]. As a result, there are studies in which the fatigue and vigor subscales of POMS have failed to demonstrate any change in fatigue between preoperative levels and early and late postoperative levels [15].
Special scales have been devised to address the above issue. The Chalder fatigue scale uses a self-rating, 14 item fatigue questionnaire. It separates mental from physical fatigue [16]. This instrument is used widely for assessment of POF. However, although bidimensional, this scale focuses on the feelings of fatigue and hence is not designed to measure the impact of POF.
Recent progress and research in illness perception theory has provided different viewpoints from which conditions, such as fatigue, can be conceptualized. Within this new framework, fatigue can be seen as Identity, Consequence, Cause, Timeline, and Control (Table 2). Using concepts of cognitive representation, a new multidimensional fatigue scale has been developed and validated, consisting of 28 questions and five subscales, and is called the Identity-Consequence Fatigue Scale. This scale measures the mental and physical feeling, as well as impact, of fatigue [14].
Objective correlates with POF
Cardiovascular fitness
One of the first objective measures of fatigue was demonstration of a correlation between fatigue and an increase in pulse rate, secondary to orthostatic stress, which was present for up to 30 days after surgery [5]. Also, postoperatively, exercise-induced heart rate is higher than during the preoperative period, and this increase is associated with POF [17]. After surgery, there is a reduction in bicycle ergometer work capacity and an increase in the cardiorespiratory effort required to perform a given task and the decline in these indicators of cardiorespiratory fitness also are associated with POF [5, 17–19]. Therefore, both light and heavy work capacities are reduced postoperatively with a demonstrable association with fatigue.
Fatigue and nutrition
It has been observed that patients who have more pronounced POF have experienced significantly greater postoperative weight loss as well as greater loss of triceps skin-fold thickness [20]. Additionally, further correlations have been demonstrated between development of POF and preoperative weight, total body protein, decline in plasma transferrin levels, and grip strength [20–22].
Fatigue and musculoskeletal changes
Development of POF has been shown to correlate with a reduction in the maximum force that a muscle can generate as well as a decline in muscle endurance (the ability of a muscle to maintain sustained contraction) [23]. Electromyographic studies have shown objectively that throughout the early postoperative period fewer muscle fiber units are activated during voluntary movements, whereas during the late postoperative course the decline in muscle performance is primarily due to weakness in individual muscle fibers [23]. During the immediate postoperative period and for up to 10 days after surgery, objective measures of muscle function (as measured by electromyographic studies) remain unchanged despite a measurable decline in voluntary muscle force and endurance in both small and large muscle groups [19, 24–27]. Therefore, it has been argued that early fatigue is “central” in origin but late fatigue is “peripheral” [19].
Postoperatively, there are a number of other physiological changes observed within muscle fibers, although these have not been shown to correlate with development of POF [17, 18, 28–31]. However, a postoperative increase in muscle glycogen stores inversely correlates with POF [17]. Based on these findings, grip strength is a commonly used objective measure in assessment of fatigue in clinical research.
Fatigue and biochemical markers
Development of POF correlates significantly to increased heart rate, and a positive relationship also is observed to an exercise-induced increase in plasma levels of noradrenaline, growth hormone, and alanine [18]. There is some correlation between fatigue and low serum transferrin at day 30 but not earlier [20]. A larger noradrenaline response in the early postoperative course is associated with more fatigue and less vigor [32]. In one study, increases in POF were accompanied by decreased serum zinc and increased serum magnesium [33].
Fatigue and type of operation
It has been demonstrated that the type of the operation can influence the extent of POF with significant differences in fatigue after middle-ear surgery and abdominal surgery of similar duration [22]. Generally, major abdominal and cardiac surgeries are associated with greater POF than minor surgery [34]. In addition, significant POF has not been observed after joint arthroplasty [10]. It has been observed that the diagnosis, particularly cancer, has some influence on the development of POF [21].
Fatigue and psychological factors
In the past, POF was thought to be a purely physical phenomenon. This was because some early data had suggested that POF may have no association with preoperative anxiety as measured by the State-Trait Anxiety Inventory [35]. Additionally, it was shown that neither preoperative nor postoperative performance during concentration tests correlated to POF. Other studies also demonstrated that POF was not associated with preoperative anxiety, depression, hostility, or preoperative stress. Later research showed a correlation between preoperative and POF: patients who were already fatigued before surgery were those most likely to suffer from prolonged POF [21].
However, as more appropriate instruments were developed and became available to measure POF, further studies demonstrated that throughout the postoperative period, there was a measurable and significant relationship between both physical and mental aspects of fatigue and low mood [10]. It was further established that anxiety and emotional distress have a highly significant association with POF [34].
It is believed that psychological factors, such as preoperative negative mood, may be predictive of the development of POF. For example, patients who complain about negative mood preoperatively have a higher level of mental fatigue postoperatively, regardless of their preoperative level of fatigue [10, 36]. Additionally, preoperative fatigue has been shown to predict low postoperative physical and emotional states [10]. Greater preoperative expectations of fatigue also predict greater POF [34]. Positive preoperative coping strategies and optimism predict decreased physical and mental POF, whereas negative coping strategies have the opposite effect [15, 36].
Etiology of POF
The etiology of POF is most likely to be multifactorial with interactions between biological, psychological, and possibly social factors. The biological aspect of POF can be divided into a physiological response to surgical trauma (i.e., the surgical stress response), a decline in nutritional status, and a reduction in physical fitness after surgery.
Fatigue and surgical trauma
As mentioned, fatigue increases significantly after major abdominal surgery. However, no such increase in fatigue is observed after middle-ear surgery, despite the fact that the durations of anesthesia and surgery are similar [22]. General anesthesia alone does not lead to changes in whole body protein breakdown, whereas these parameters are significantly affected after surgery [37]. It has been postulated that it is the type of operation (i.e., magnitude of the trauma), rather than other factors, such as the duration of anesthesia, that may be involved in the pathogenesis of POF.
Although POF has been demonstrated after major abdominal and pelvic surgery in a number of studies, significant POF has not been observed after orthopedic operations (joint arthroplasty), despite the fact that the latter procedure has been shown to be associated with a similar magnitude of systemic hormonal response after surgery [8, 10, 32, 38–41]. Furthermore, if POF was solely related to the systemic plasma endocrine-metabolic response to surgery, it would be expected that suppression of this physiological response would significantly influence POF. However, in a controlled study, epidural analgesia and systemic nonsteroidal inflammatory drug treatment did not modify POF after major abdominal surgery, despite decreasing the endocrine response [42]. Additionally laparoscopic cholecystectomy has been shown to be associated with less POF compared with open surgery despite a similar metabolic response to surgery [43]. Therefore, the variation in fatigue measurements after different types of operations cannot be solely due to the extent of surgical trauma, as measured by plasma markers of inflammation or stress hormones. Other factors must be implicated.
Fatigue and nutrition
As previously mentioned, a number of indicators of decline in nutritional status have been linked to the development of POF. Based on these findings, it is thought that nutritional factors may be involved in the pathogenesis of POF. Abdominal surgery is followed by a decline in the quality of nutritional intake as well as loss of gastrointestinal function. This factor could partially explain the higher levels of POF after abdominal surgery compared with orthopedic or middle-ear operations. However, fasting alone cannot explain the onset of fatigue after surgery because healthy fasting people do not demonstrate the reduction in working capacity, skeletal muscle function, and fatigue that is seen after major surgery [19]. Furthermore, nutritional interventions alone have not been shown to be effective in reducing POF [44]. However, when the catabolic response to surgery is controlled by treatment with anabolic agents, such as human growth hormone, as well as nutritional support, improvements in total muscle strength and lean tissue mass are associated with a reduction in POF [45]. Hence, nutritional deficits partially, but not completely, explain the etiology of POF.
Fatigue and physical fitness
Surgery is followed by a prolonged period of reduced activity, which can lead to significant impairment of muscle functioning, particularly endurance, similar to changes seen in volunteers undergoing bed rest [27, 34, 46]. Additionally, cardiovascular fitness also deteriorates after surgery. Objective measures of cardiovascular fitness and musculoskeletal deterioration both correlate with development of POF [5, 17–19, 21]. Therefore, as muscular endurance and cardiac fitness both decline, patients may need to use more energy to perform a given physical task, which may lead to sensations of fatigue [34]. These factors are thought to lead to reduced mobility and contribute to fatigue [19]. Patients who believe in the efficacy of postoperative physical activity for recovery, and hence may be more active after their operation, experience less POF and those with less physical fitness are more fatigued postoperatively [34]. Disappointingly, in a randomized, controlled trial, combined postoperative strength and aerobic training for patients who underwent major colorectal surgery failed to improve the decline in physical function compared with a placebo group. This intervention only moderately reduced early fatigue and did not influence late POF [47].
Fatigue and psychological theory
The psychological aspect of POF has been explained by somatization and cognitive-behavioral theories. The somatization concept is related to the response expectancy theory, which states that response expectancies are sufficient to cause nonvolitional outcomes (i.e., physiological symptoms) [48]. According to the somatization theory, patients experience negative mood after surgery but misinterpret this as fatigue. This is due to environmental factors, such as being hospitalized, and also due to the presence of preoperative fatigue. Therefore, patients continue to monitor and anticipate worsening of these feelings [49]. Cognitive-behavioral factors include patients’ interpretation of their own symptoms and the medical advice that they receive as well as their coping strategies and the course of action that they take during their recovery course. These factors are thought to influence their subjective feelings of fatigue [34].
Somatization can partially explain the difference in POF seen in orthopedic and abdominal operations [34]. In an orthopedic procedure, such as elective hip replacement, the operation precedes a waited event, such as improved mobility, whereas an abdominal procedure has little obvious immediate quality-of-life benefits for the patient. Hence, patients may feel more fatigued after an abdominal operation. Cognitive-behavioral factors, such as having a firm belief in the efficacy and benefits of postoperative activity in late postoperative course, are predictive of less POF. However, it has been shown that it is the specific expectation of fatigue and not other factors—such as the prospect of generalized disability or the risks and benefits of the operation—that relates to the development of POF [34]. Thus, the idea that postoperatively patients reinterpret any negative emotion, such as anxiety or depression as fatigue (i.e., somatization), cannot entirely explain the etiology of POF. It is thought that early symptoms of fatigue may be due to somatization and late fatigue secondary to cognitive-behavioral factors [34].
The level of social support available for patients may partly determine their postoperative activity levels. Greater social support has been linked to better emotional outcome after an operation, although more support may delay mobilization and greater support has been linked to higher levels of fatigue after viral infections [34, 46]. Nevertheless, no links have been shown between social support and POF and social factors seem to have little influence on the onset of POF [34, 50, 51].
Tryptophan is the precursor of the neurotransmitter 5-hydroxytryptamine (5-HT), known to be involved in sleep and fatigue. Free tryptophan levels in blood are increased after surgery, which is associated with an increased amount of tryptophan entering the brain [52]. This may lead to higher 5-HT concentrations in some parts of the brain, may contribute to a need for increase in sleep, and possibly an increase in central fatigue [52]. Subsequently, significant correlations have been shown between fatigue scores and plasma-free tryptophan [53]. Postoperative sleep disturbance, on its own, does not seem to correlate with the development of POF [54].
Fatigue and cytokines
More recently, associations between fatigue and inflammatory cytokines have been demonstrated. Many proinflammatory cytokines have been shown to induce fatigue after exogenous administration [55–58]. Even low levels of cytokines, which do not influence increased temperature or other physical symptoms, caused a decline in mood in healthy volunteer subjects [59]. In a study of healthy volunteers, injection of Salmonella typhi vaccine led to an increase of interleukin (IL)-6 levels in plasma, and this was associated with a significant reduction in mood in the absence of any other physical symptoms. Furthermore, this change significantly correlated with plasma IL-6 levels [59]. Further studies have demonstrated that cytokines (IL-1β and IL-6) can induce human “sickness behavior,” such as fever, malaise, pain, fatigue, low mood, and poor concentration [57, 60]. It has been shown that patients with multiple sclerosis (MS) who experience fatigue have significantly higher levels of interferon gamma and tumor necrosis factor alpha than patients with MS who do not experience fatigue, with considerable correlation between these proinflammatory cytokines and fatigue scores [1].
POF also may be linked to production of proinflammatory cytokines. After surgery, there are two possible channels of communication between the periphery and the brain. One is a hormonal route by which the cytokines produced at the site of surgery enter the blood stream and proceed through a variety of mechanisms to act directly on the brain. The second method is a neural route represented by paracrine actions of cytokines on primary afferent neurons, which innervate the body site where the injury has taken place [61]. In the abdominal cavity, the vagus nerve plays an important role in the latter form of communication [62]. Therefore, cytokines produced at the site of surgery may act via the vagus and play a key role in production of POF.
The unique role of the vagus nerve, with its termination at nucleus tractus solitarius (NTS) may at least partly explain the etiology of POF in abdominal surgery [62]. The NTS is intensely activated and also is by far the most sensitive area, after peripheral immune stimulation [63–65]. The NTS projects monosynaptically to many regions of the brain that mediate sickness responses [62]. Subdiaphragmatic vagotomy in animals has been shown to block or reduce a broad spectrum of sickness responses to intraperitoneal administration of cytokines as well as inhibiting the neural activation of the brainstem, hypothalamus, and limbic structures in response to these stimuli [61]. It is important to note that the role of the vagus afferents is mainly to influence behavioral changes rather than affect fever or activation of hypothalamic-pituitary-adrenal axis [55]. Thus, a proinflammatory cytokine pathway with direct action on the vagus nerve is a feasible partial explanation for POF [66]. New data demonstrate that POF is significantly related to the IL-6, IL-10, and tumor necrosis factor alpha concentrations present within the peritoneal cavity during the initial 24-h period after surgery [67].
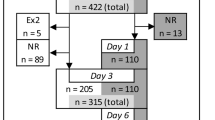
Another relevant factor may be the concentration of various cytokines at the site of surgery. Although after joint arthroplasty there is an increase in the plasma level of cytokines similar to that observed after major abdominal surgery, the local concentration of these cytokines has been shown to be much smaller after joint arthroplasty compared with abdominal procedures. Hence, the concentration of cytokines at the site of the injury may be an important determinant of the severity of injury after surgery, duration of recovery, and POF (Fig. 1) [68, 69].
Conclusions
Postoperative fatigue should be defined as a collection of physical and psychological symptoms that delay return to normal activity after surgery. This definition recognizes the fact that POF has a multimodal etiology and disrupts normal function after surgery and hence is clinically significant.
POF has a multimodal etiology, and therefore, single-modality interventions seem to have little influence on the progression of POF. A meta-analysis has assessed various interventions used to modify POF, and there may be no single intervention to effectively eliminate POF. However, with the implementation of multimodal enhanced care pathways, combining strategies, such as psychological intervention, thoracic epidural, early nutrition, minimal access surgery, and early mobilization, there is evidence that significant and clinically measurable improvements in POF may be achieved [44, 70–72].
References
Heesen C, Nawrath L, Reich C et al (2006) Fatigue in multiple sclerosis: an example of cytokine mediated sickness behaviour? J Neurol Neurosurg Psychiatr 77:34–39
Papanicolaou DA, Amsterdam JD, Levine S et al (2004) Neuroendocrine aspects of chronic fatigue syndrome. Neuroimmunomodulation 11:65–74
Smets EM, Garssen B, Schuster-Uitterhoeve AL et al (1993) Fatigue in cancer patients. Br J Cancer 68:220–224
Lee BN, Dantzer R, Langley KE et al (2004) A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. Neuroimmunomodulation 11:279–292
Christensen T, Bendix T, Kehlet H (1982) Fatigue and cardiorespiratory function following abdominal surgery. Br J Surg 69:417–419
Schroeder D, Hill GL (1991) Postoperative fatigue: a prospective physiological study of patients undergoing major abdominal surgery. Aust N Z J Surg 61:774–779
Rubin GJ, Hardy R, Hotopf M (2004) A systematic review and meta-analysis of the incidence and severity of postoperative fatigue. J Psychosom Res 57:317–326
DeCherney AH, Bachmann G, Isaacson K et al (2002) Postoperative fatigue negatively impacts the daily lives of patients recovering from hysterectomy. Obstet Gynecol 99:51–57
Bisgaard T, Klarskov B, Rosenberg J et al (2001) Factors determining convalescence after uncomplicated laparoscopic cholecystectomy. Arch Surg 136:917–921
Aarons H, Forester A, Hall G et al (1996) Fatigue after major joint arthroplasty: relationship to preoperative fatigue and postoperative emotional state. J Psychosom Res 41:225–233
Wessely S, Powell R (1989) Fatigue syndromes: a comparison of chronic “postviral” fatigue with neuromuscular and affective disorders. J Neurol Neurosurg Psychiatr 52:940–948
Schwartz JE, Jandorf L, Krupp LB (1993) The measurement of fatigue: a new instrument. J Psychosom Res 37:753–762
Smets EM, Garssen B, Bonke B et al (1995) The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 39:315–325
Paddison JS, Booth RJ, Hill AG et al (2006) Comprehensive assessment of peri-operative fatigue: development of the Identity-Consequence Fatigue Scale. J Psychosom Res 60:615–622
Matsushita T, Murata H, Matsushima E et al (2007) Emotional state and coping style among gynecologic patients undergoing surgery. Psychiatry Clin Neurosci 61:84–93
Chalder T, Berelowitz G, Pawlikowska T et al (1993) Development of a fatigue scale. J Psychosom Res 37:147–153
Christensen T, Nygaard E, Stage JG et al (1990) Skeletal muscle enzyme activities and metabolic substrates during exercise in patients with postoperative fatigue. Br J Surg 77:312–315
Christensen T, Stage JG, Galbo H et al (1989) Fatigue and cardiac and endocrine metabolic response to exercise after abdominal surgery. Surgery 105:46–50
Zeiderman MR, Welchew EA, Clark RG (1990) Changes in cardiorespiratory and muscle function associated with the development of postoperative fatigue. Br J Surg 77:576–580
Christensen T, Kehlet H (1984) Postoperative fatigue and changes in nutritional status. Br J Surg 71:473–476
Schroeder D, Hill GL (1993) Predicting postoperative fatigue: importance of preoperative factors. World J Surg 17:226–231
Christensen T, Hougard F, Kehlet H (1985) Influence of pre- and intra-operative factors on the occurrence of postoperative fatigue. Br J Surg 72:63–65
Christensen T, Wulff C, Fuglsang-Frederiksen A et al (1985) Electrical activity and arm muscle force in postoperative fatigue. Acta Chir Scand 151:1–5
Brough W, Horne G, Blount A et al (1986) Effects of nutrient intake, surgery, sepsis, and long term administration of steroids on muscle function. Br Med J (Clin Res Ed) 293:983–988
Newham DJ, Harrison RA, Clark CG (1987) Skeletal muscle function after major abdominal surgery. Hum Nutr Clin Nutr 41:363–371
Maxwell A (1980) Muscle power after surgery. Lancet 1:420–421
Edwards H, Rose EA, King TC (1982) Postoperative deterioration in muscular function. Arch Surg 117:899–901
Christensen T, Nygaard E, Kehlet H (1988) Skeletal muscle fiber composition, nutritional status and subjective fatigue during surgical convalescence. Acta Chir Scand 154:335–338
Klausen K, Andersen LB, Pelle I (1981) Adaptive changes in work capacity, skeletal muscle capillarization and enzyme levels during training and detraining. Acta Physiol Scand 113:9–16
Petersson B, Wernerman J, Waller SO et al (1990) Elective abdominal surgery depresses muscle protein synthesis and increases subjective fatigue: effects lasting more than 30 days. Br J Surg 77:796–800
Essen P, Wernerman J, Sonnenfeld T et al (1992) Free amino acids in plasma and muscle during 24 hours postoperatively: a descriptive study. Clin Physiol 12:163–177
Hall GM, Salmon P (2002) Physiological and psychological influences on postoperative fatigue. Anesth Analg 95:1446–1450
Cordova A (1995) Variations of serum magnesium and zinc after surgery, and postoperative fatigue. Magnes Res 8:367–372
Rubin GJ, Cleare A, Hotopf M (2004) Psychological factors in postoperative fatigue. Psychosom Med 66:959–964
Christensen T, Hjortso NC, Mortensen E et al (1986) Fatigue and anxiety in surgical patients. Acta Psychiatr Scand 73:76–79
Ai AL, Peterson C, Tice TN et al (2006) Differential effects of faith-based coping on physical and mental fatigue in middle-aged and older cardiac patients. Int J Psychiatry Med 36:351–365
Carli F, Ramachandra V, Gandy J et al (1990) Effect of general anaesthesia on whole body protein turnover in patients undergoing elective surgery. Br J Anaesth 65:373–379
Carlson KJ, Miller BA, Fowler FJ Jr (1994) The Maine Women’s Health Study: I. Outcomes of hysterectomy. Obstet Gynecol 83:556–565
Gould D, Wilson-Barnett J (1985) A comparison of recovery following hysterectomy and major cardiac surgery. J Adv Nurs 10:315–323
Richards DH (1974) A post-hysterectomy syndrome. Lancet 2:983–985
Hall GM, Peerbhoy D, Shenkin A et al (2001) Relationship of the functional recovery after hip arthroplasty to the neuroendocrine and inflammatory responses. Br J Anaesth 87:537–542
Schulze S, Roikjaer O, Hasselstrom L et al (1988) Epidural bupivacaine and morphine plus systemic indomethacin eliminates pain but not systemic response and convalescence after cholecystectomy. Surgery 103:321–327
Hill AG, Finn P, Schroeder D (1993) Postoperative fatigue after laparoscopic surgery. Aust N Z J Surg 63:946–951
Rubin GJ, Hotopf M (2002) Systematic review and meta-analysis of interventions for postoperative fatigue. Br J Surg 89:971–984
Kissmeyer-Nielsen P, Jensen MB, Laurberg S (1999) Perioperative growth hormone treatment and functional outcome after major abdominal surgery: a randomized, double-blind, controlled study. Ann Surg 229:298–302
Baker CA (1989) Recovery: a phenomenon extending beyond discharge. Sch Inq Nurs Pract 3:181–197
Houborg KB, Jensen MB, Rasmussen P et al (2006) Postoperative physical training following colorectal surgery: a randomised, placebo-controlled study. Scand J Surg 95:17–22
Kirsch I (1990) Changing expectations: a key to effective psychotherapy. Brooks/Cole Publishing Co., Pacific Grove, CA
Salmon P, Hall GM (1997) A theory of postoperative fatigue: an interaction of biological, psychological, and social processes. Pharmacol Biochem Behav 56:623–628
Webb C (1986) Professional and lay social support for hysterectomy patients. J Adv Nurs 11:167–177
Borstlap M, Zant JL, van Soesbergen RM et al (1995) Quality of life assessment: a comparison of four questionnaires: for measuring improvements after total hip replacement. Clin Rheumatol 14:15–20
Yamamoto T, Castell LM, Botella J et al (1997) Changes in the albumin binding of tryptophan during postoperative recovery: a possible link with central fatigue? Brain Res Bull 43:43–46
McGuire J, Ross GL, Price H et al (2003) Biochemical markers for post-operative fatigue after major surgery. Brain Res Bull 60:125–130
Rosenberg-Adamsen S, Kehlet H, Dodds C et al (1996) Postoperative sleep disturbances: mechanisms and clinical implications. Br J Anaesth 76:552–559
Konsman JP, Parnet P, Dantzer R (2002) Cytokine-induced sickness behaviour: mechanisms and implications. Trends Neurosci 25:154–159
Cohen O, Reichenberg A, Perry C et al (2003) Endotoxin-induced changes in human working and declarative memory associate with cleavage of plasma “readthrough” acetylcholinesterase. J Mol Neurosci 21:199–212
Reichenberg A, Yirmiya R, Schuld A et al (2001) Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry 58:445–452
Krabbe KS, Reichenberg A, Yirmiya R et al (2005) Low-dose endotoxemia and human neuropsychological functions. Brain Behav Immun 19:453–460
Wright CE, Strike PC, Brydon L et al (2005) Acute inflammation and negative mood: mediation by cytokine activation. Brain Behav Immun 19:345–350
Vollmer-Conna U, Fazou C, Cameron B et al (2004) Production of pro-inflammatory cytokines correlates with the symptoms of acute sickness behaviour in humans. Psychol Med 34:1289–1297
Dantzer R, Konsman JP, Bluthe RM et al (2000) Neural and humoral pathways of communication from the immune system to the brain: parallel or convergent? Auton Neurosci 85:60–65
Maier SF, Goehler LE, Fleshner M et al (1998) The role of the vagus nerve in cytokine-to-brain communication. Ann N Y Acad Sci 840:289–300
Wan W, Wetmore L, Sorensen CM et al (1994) Neural and biochemical mediators of endotoxin and stress-induced c-fos expression in the rat brain. Brain Res Bull 34:7–14
Ericsson A, Kovacs KJ, Sawchenko PE (1994) A functional anatomical analysis of central pathways subserving the effects of interleukin-1 on stress-related neuroendocrine neurons. J Neurosci 14:897–913
Butler PD, Edwards E, Barkai AI (1989) Imipramine and tetrabenazine: effects on monoamine receptor binding sites and phosphoinositide hydrolysis. Eur J Pharmacol 160:93–100
Schulze S, Sommer P, Bigler D et al (1992) Effect of combined prednisolone, epidural analgesia, and indomethacin on the systemic response after colonic surgery. Arch Surg 127:325–331
Paddison JS, Booth RJ, Fuchs D et al (2008) Peritoneal inflammation and fatigue experiences following colorectal surgery: a pilot study. Psychoneuroendocrinology 33:446–454
Badia JM, Whawell SA, Scott-Coombes DM et al (1996) Peritoneal and systemic cytokine response to laparotomy. Br J Surg 83:347–348
Kristiansson M, Soop M, Sundqvist KG et al (1998) Local vs. systemic immune and haemostatic response to hip arthroplasty. Eur J Anaesthesiol 15:260–270
Jakobsen DH, Sonne E, Andreasen J et al (2006) Convalescence after colonic surgery with fast-track vs conventional care. Colorectal Dis 8:683–687
Hjort Jakobsen D, Sonne E, Basse L et al (2004) Convalescence after colonic resection with fast-track versus conventional care. Scand J Surg 93:24–28
Zargar-Shoshtari K, Paddison J, Booth R et al (2008) A prospective study on the influence of a fast-track programme on postoperative fatigue and functional recovery after major colonic surgery. J Surg Res [Epub ahead of print]
Krupp LB, Alvarez LA, LaRocca NG et al (1988) Fatigue in multiple sclerosis. Arch Neurol 45:435–437
Monk TH (1989) A Visual Analogue Scale technique to measure global vigor and affect. Psychiatry Res 27:89–99
Pearson PG, Byars G (1956) The development and validation of a checklist measuring subjective fatigue (report No. 56–115). School of Aviation USAF, Randolf AFB, Texas
Mendoza TR, Wang XS, Cleeland CS et al (1999) The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer 85:1186–1196
Krupp LB, LaRocca NG, Muir-Nash J et al (1989) The Fatigue Severity Scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46:1121–1123
Aaronson NK, Ahmedzai S, Bergman B et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Fawzy FI, Cousins N, Fawzy NW et al (1990) A structured psychiatric intervention for cancer patients. I. Changes over time in methods of coping and affective disturbance. Arch Gen Psychiatry 47:720–725
Piper BF, Lindsey AM, Dodd MJ, Ferketich S, Paul SM, Weller S (1989) The development of an instrument to measure the subjective dimension of fatigue. Springer, New York
Acknowledgement
The research was conducted during tenure of a Clinical Research Training Fellowship from Health Research Council of New Zealand.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zargar-Shoshtari, K., Hill, A.G. Postoperative Fatigue: A Review. World J Surg 33, 738–745 (2009). https://doi.org/10.1007/s00268-008-9906-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9906-0