Abstract
Background and aims
Submucosal tunneling endoscopic resection (STER) has been proved to be effective and safe for esophageal submucosal tumors (SMTs) originating from the muscularis propria (MP) layer. This study was aimed to further evaluate the effectiveness, safety, and influencing factors especially the types of mucosal incision of STER in a larger population.
Methods
A total of 89 patients undergoing STER with esophageal SMTs were retrospectively enrolled in this study from May 2012 to November 2016. Clinicopathological, endoscopic, and adverse events (AEs) data were collected and analyzed. Different incision methods were compared to evaluate the optimum incision method.
Results
There were 27 females and 62 males with mean age of 46.5 ± 10.3 years. The medium size of the tumors was 16.0 mm (ranging 10.0–60.0 mm). Inverted T incisions were made in 29 (32.6%) patients, transverse incisions in 12 (13.5%) while longitudinal incisions in 48 (53.9%). En bloc resection was achieved in 70 (78.7%) patients. The residual rate was 1.1% (1/89), and no recurrence was noted even after piecemeal resection. The rate of AEs was 21.3% (19/89), and all of the AEs were cured without intervention or treated conservatively without the need for surgery. The en bloc resection rate was comparable among the three incision groups (P = 0.868); however, the incidence of AEs in the inverted T incision was lower than that in the longitudinal incision (P = 0.003). Fewer clips were used in the inverted T incision group than in the transverse incision group (P = 0.003).
Conclusions
Although STER failed to achieve en bloc resection in 21.3% patients, it was still an effective therapy owing to low residual rate and no recurrence rate after piecemeal resection. STER was safe with no severe AEs; however, minor AEs were common. Inverted T incision seems to be the optimum entry point.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With the development of imaging techniques, the detection rate of gastrointestinal submucosal tumors (SMTs), which are usually asymptomatic, has become increasingly high [1]. SMTs covered with normal mucosa have a broad differential diagnosis and are mainly divided into leiomyomas, gastrointestinal stromal tumors (GISTs), and lipomas. GISTs less than 2 cm and leiomyomas most of which are benign can be treated by resection or surveillance [2, 3]. However, some of SMTs have the possibility of being malignant, especially those originating from the muscularis propria (MP) or those with a large diameter [1, 4,5,6]. Treatments vary with the types of SMTs. An endoscopic fine-needle biopsy is not necessary, especially when SMTs are easily resected and the accuracy of biopsy seems low [2, 7]. The elimination of malignancy seems difficult without resection. Long-term surveillance may increase the financial burden and psychological stress for patients and delay the diagnosis of malignancy and treatment. Therefore, early removal of SMTs is necessary.
Surgery and endoscopic resection are current therapies for SMTs [8]. Surgery, no matter open or laparoscopic, seems more invasive, less cost-effective and more time-consuming, with longer hospital stay, compared with endoscopic resection [9, 10]. Endoscopic techniques, such as endoscopic submucosal dissection (ESD), endoscopic submucosal excavation (ESE), and endoscopic full-thickness resection (EFR), are reported as feasible, effective, and safe methods for SMTs arising from MP [10,11,12,13,14]. The resection of MP tissue in two pigs was reported in 2011 [15]. Submucosal tunneling endoscopic resection (STER) is a novel technique, named by Xu et al., used to resect SMTs in 2012 [7]. STER was preliminarily proved to be more advantageous than ESD, ESE, and EFR in treating SMTs because it could maintain the integrity of digestive tract mucosa by establishing a tunnel between submucosal and MP [16,17,18]. The aim of this retrospective study was to further evaluate the effectiveness and safety of STER for esophageal SMTs originating from the MP layer in a larger population and the factors especially the methods of mucosal incision which might affect the effectiveness and safety of STER.
Materials and methods
Patients
From May 2012 to November 2016, endoscopic resection was conducted on 104 consecutive patients diagnosed with esophageal SMTs originating from the MP layer in our Gastrointestinal Endoscopic Center. A total of 89 patients undergoing STER were included after excluding 15 patients undergoing ESD. Patients undergoing STER met the following inclusion criteria: (1) diagnosis with esophageal SMTs originating from the MP layer; (2) age ≥18 years old; (3) no possibility of malignancy; (4) no signs of metastasis or invasion outside the digestive tract; (5) SMTs ≥10.0 mm; and (6) signing informed consent. Exclusion criteria were as follows: (1) reluctance to undergo STER or inability to sign informed consent; (2) inability to tolerate anesthesia; (3) high risk of operation or pregnancy; and (4) coagulopathy (international normalized ratio>1.5, platelets <50,000). This study was approved by the Committee of Medical Ethics of Chinese People’s Liberation Army General Hospital.
Outcome measurements
The effectiveness of STER was evaluated mainly using the following outcome measures: complete resection rate, en bloc resection rate, recurrence rate, and residual rate. The operation time, hospital time, number of clips used to close the mucosal incision, incision healing conditions during follow-up and cost were recorded as the secondary outcome measures. The safety of STER was analyzed mainly in terms of adverse events (AEs) related to the procedure, such as subcutaneous or mediastinal emphysema, pneumothorax, pleural effusion, mucosal injury, fever, severe chest pain that needed intervention and acute or delayed major bleeding.
Complete resection was defined as removal of the tumor en bloc with negative lateral and basal margins on pathologic examination. Recurrence was regarded as SMTs were revealed within 1.0 cm around primary resected lesions more than 6 months after STER, while residual meant re-detection of SMTs within 1.0 cm around primary resected lesions less than 6 months after STER. The period between submucosal injection and closure of mucosal incision was calculated as operation time while the hospital time began from operation day. Temperature more than 38 °C was recorded as fever in the present study. Temperature no more than 38 °C, mainly caused by post-procedure absorption, was pretty common without the need for additional therapy. Therefore, it was not regarded as an AE. Major bleeding was defined as consecutive bleeding for more than 1 min, bleeding more than 200 mL [19], hematemesis or hematochezia which needed blood transfusion or surgery. Upper esophageal lesions were defined as those located 15–24 cm from the incisors, middle as those located 25–32 cm from the incisors, and lower as those located 33 cm from the incisors to the gastroesophageal junction. The size of the tumor was determined by endoscopic ultrasound (EUS).
STER procedure
Patients suspected to have SMTs were examined with mediastinal-enhanced computed tomography (CT) and EUS to evaluate the size, location, shape, and depth of the tumor and eliminate metastasis or invasion outside the digestive tract prior to STER. All patients fasted for 8 h before STER. STER procedure was mainly conducted by two operators with experience of more than 100 cases of peroral endoscopic myotomy (POEM).
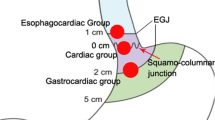
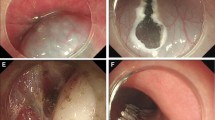
STER was conducted with patients in the left-lateral position under intravenous anesthesia. The surgical procedure was performed mainly based on the steps reported by Xu et al. [7]. with some modifications. The key steps of the STER procedure were as follows (Fig. 1). Examination under a liner-array echoendoscope (Prosound F75; Aloka, Tokyo, Japan, and GF-UCT260; Olympus, Tokyo, Japan) was done before STER to evaluate the size, location, and depth of the lesion. A single-channel gastroscope (GIF Q260 J/GIF Q290 J; Olympus) attaching a transparent cap (D-201-11802; Olympus) was used during the procedures. A high-frequency generator (VIO 200D; ERBE, Tübingen, Germany) and an argon plasma coagulation unit (APC300; ERBE) were used. A carbon dioxide (CO2) insufflator (UCR; Olympus,) was used to achieve CO2 insufflation. First, submucosal fluid cushion using an injection needle (NM-4L-1; Olympus) was made at 3–5 cm proximal to the tumor. Second, a 2-cm longitudinal mucosal incision, a 1.5–1.8-cm transverse incision, or an inverted T incision combined with a 0.5-cm transverse incision and a 1.0-cm longitudinal incision was made with a triangular knife (KD-640L; Olympus) as the entry point (Fig. 2). Third, a triangular knife was used to establish a longitudinal tunnel ending 1–2 cm distal to the tumor between the submucosal and muscular layers. Then, the tumor was resected using an insulation-tip knife (KD611L, IT2; Olympus) or a triangular knife. In some cases, a snare (ASM-1-S or ASJ-1-S; Cook, Indiana, USA) was used to resect the tumor. Finally, the incision was closed with several clips (HX-610-135; Olympus). All three kinds of incisions were closed in a longitudinal fashion. Hot biopsy forceps (FD-410LR; Olympus) were used to stop bleeding during the procedure.
Submucosal tunneling endoscopic resection (STER) for an esophageal submucosal tumor (SMT). A Endoscopic view of a submucosal tumor located in middle esophagus. B Endoscopic ultrasound (EUS) view of the same lesion, showing the tumor originating from the muscularis propria. C Inverted T mucosal incision 5 cm proximal to the submucosal tumor. D Creating a submucosal tunnel to the lesion. E Dissection along the margin of the tumor within the tunnel. F En bloc resection of the tumor. G The mucosal entry incision. H Closure of tunnel entry with clips. I The resected specimen. J Endoscopic follow-up 6 months after operation, showing a small scar on the mucosal entry
Postoperative treatment and follow-up
The complete blood count was examined on the morning after STER. Any discomforts, such as fever, chest pain, hematemesis, and hematochezia, were closely monitored. Oral intake of food was restarted 3 days after STER. All patients were intravenously administered a proton pump inhibitor (PPI) for 3 days, after which oral PPI therapy was continued for 4 weeks. Post-procedure intravenous antibiotics were stopped after 2–3 days if no signs of infection were noted. Prophylactic intravenous antibiotics were not administered before the procedure in current study. Patients underwent gastroscopy and (or) EUS at 1, 3, 6, and 12 months after the operation and then annually.
Statistical analysis
All calculations were performed by using SPSS17.0. Quantitative data, like patients’ age, SMTs’ size, operation time, hospital time, and cost, were expressed as mean ± standard deviation or median (minimum and maximum values) and assessed by t test, nonparametric test, or variance analysis according to distribution characteristics and number of groups. Enumeration data, such as number of clips, complete resection rate, en bloc resection, recurrence, and residual, were expressed as frequencies and assessed using the Fisher’s exact test or the χ 2 test. A P value <0.05 was considered significant.
Results
From May 2012 to November 2016, endoscopic resection was conducted on 104 consecutive patients diagnosed with upper esophageal SMTs originating from the MP layer in our Gastrointestinal Endoscopic Center. A total of 89 patients undergoing STER were included after excluding 15 patients undergoing ESD. Baseline characteristics are described in Table 1. The study included 27 females and 62 males with mean age of 46.5 ± 10.3 years. About 10 tumors were localized in the upper esophagus, 37 in the middle esophagus, and 42 in the lower esophagus. The median size of the tumors and median length of the tunnel were 16.0 mm (range 10.0–60.0 mm) and 7.0 cm (range 5.0–11.0 cm), respectively. Inverted T incisions were made in 29 (32.6%) patients, transverse incisions in 12 (20.3%) patients, and longitudinal incisions in 48 (53.9%) patients. Follow-up gastroscopy was performed in a median time duration of 6 months (ranging 1–48 months). The final pathological diagnosis was as follows: 87 (97.8%) leiomyomas,1 (1.1%) fibrous tumor, and 1 (1.1%) lipoma.
Effectiveness of STER
STER was successfully performed in all of 89 patients. En bloc resection was achieved in 70 (78.7%) patients. The margins of all en bloc resected SMTs were negative. Therefore, the complete resection rate was 70 (78.7%). One SMT was not resected with residual owing to the big size and deep invasion, which caused great difficulty during operation and high risk to the patient. No other residual lesions were found except that one with the residual rate of 1.1% (1/89). No recurrence was noted during the follow-up, and incisions of all patients healed well. The median operation time and hospital time were 40 min (range 12–142 min) and 7 days (range 5–18 days), respectively. The medium number of clips used to close the incision was 6 (range 3–22). Patients spent a median of 4590.20 USD (range 2927.38–11931.91 USD). The outcomes are shown in Table 2.
Safety of STER
All of 19 patients had AEs intraoperatively and postoperatively with the rate of 21.3% (19/89) (Table 3). Patients might have several kinds of discomfort simultaneously. Gas-related symptoms and fever were the most common AEs, followed by postprocedural pain. Gas-related AEs with or without other discomfort occurred in eight patients with an incidence of 9.0% (8/89). Fever alone or with others occurred in 9.0% (8/89) patients, while the incidence of pain and mucosal injury with or without other discomforts was 4.5% (4/89) and 3.4% (3/89), respectively. No severe AEs occurred, and all of the AEs were cured without intervention or treated conservatively without the need for surgery.
Factors affecting the effectiveness and safety of STER
When comparing the en bloc resection group with the piecemeal resection group in terms of baseline characteristics (Table 4), en bloc resection was more easily achieved for smaller SMTs than for the larger ones. The present univariate analysis showed no significant difference in age, sex, and location between the two groups.
The characteristics of the two groups (with AEs group vs without AEs group) are demonstrated in Table 5. Among the variables, larger size, and longer operation time were more likely to lead to AEs while age, sex and location were not the risk factors for AEs related to STER. Significant differences in cost and hospital time were found between the two groups.
Effectiveness and safety of STER among different methods of incision
Three kinds of incision methods (inverted T incision, transverse incision, and longitudinal incision) were compared with each other in terms of therapeutic outcomes (Table 6). The baseline characteristics, such as age, sex, tumor location, and tumor size, were comparable among the three groups (P ≥ 0.05). No significant differences were found in the length of tunnel, operation time, hospital time, and cost among different incision methods. En bloc resection rates achieved in different groups were similar to each other. However, the incidence of AEs in the inverted T incision group was lower than that in the longitudinal incision group (P = 0.003) and similar to that in the transverse incision group (P = 0.068). AEs among three kinds of incision methods are shown in Table 7. Fewer clips were used to close the incision in the inverted T incision group than in the transverse incision group (P = 0.003). No significant difference was observed in the number of clips between the inverted T group and the longitudinal incision group (P = 0.118).
Discussion
EMR and ESD performed well in superficial lesions originating from the mucosal and submucosal layers, such as early-stage cancer and superficial SMTs. Although, ESD was reported to be promising in treating esophageal MP tumors [20], the en-bloc resection rate was merely 64–75% for SMTs originating from the MP layer [21]. ESE and EFR were demonstrated to resect SMTs deeper than submucosa successfully [13, 22,23,24]. However, perforation and infection related to ESE and EFR were common. All of these four endoscopic methods could not maintain mucosal integrity which had the possibility of resulting in perforation, infection, and postoperative strictures [25].
POEM was clinically reported as a treatment for achalasia by creating a tunnel between the submucosal and the MP layer to maintain the integrity of the mucosal layer and decrease procedure-related AEs [26]. Inspired by POEM, STER was introduced as a new tunneling therapy in 2012 to treat SMTs originating from the MP layer [7]. Few studies on small populations have proved that STER is effective and safe [6, 9, 27, 28]. This study was designed to further evaluate the effectiveness and safety of STER for esophageal SMTs originating from the MP layer in a larger population and the factors, especially the types of mucosal incision which might affect the effectiveness and safety of STER.
A total of 89 patients with esophageal SMTs undergoing STER were retrospectively enrolled in the present study. Most of the SMTs in this study were leiomyomas confirmed by pathology. The en bloc resection rate was 83.3–100% in previous studies [29], which was higher than that in the present study (78.7%). Nearly, one-fourth SMTs were treated with a piecemeal resection in this study. However, no recurrence and residual lesions were reported, except for a residual SMT with big size and deep invasion. This lesion was as large as 45.0 mm in diameter and located in deep MP with an irregular shape. Resecting it completely was pretty difficult and risky. Only a part of the lesion was resected to avoid perforation and ensure safety. It seemed that the piecemeal resection did not affect the prognosis of STER. The reasons for low en bloc resection rate in the present study were as follows. In some patients, a snare was used to quickly resect the lesion after most of the SMTs were fully exposed except the basal margin, making it easier to resect the remaining part of the lesion. The piecemeal resection made the surgical time shorter and removal of lesions easier. It was shown that the piecemeal resection of leiomyomas did not influence long-term outcomes [30] and longer operation time would increase AEs [19]. The median operation time in the present study was 39 min, much shorter than that in previous studies (ranging from 47 to 152.4 min). The piecemeal resection might contribute to a shorter operation time. However, the piecemeal resection made the pathological evaluation difficult. Previous studies showed that it was hard to ensure en bloc resection for SMTs larger than 35 mm [31]. Therefore, operators should try to achieve en bloc resection for SMTs smaller than 35 mm. They should weigh pros and cons of piecemeal resection for large and (or) deep invasive lesions, which make the en bloc resection difficult and time-consuming.
The AEs rate was 21.3% (19/89) in this study. Previous studies about the safety of STER in treating upper gastrointestinal SMTs showed a AEs rate ranging from 5 to 43.75% [6, 9, 16, 17, 19, 24, 25, 28]. Gas-related AEs were reported to be the most common AEs with the incidence ranging from 3.5 to 28.1% [6, 9, 19, 25, 28], which was in accordance with the present findings. Fever and mucosal injury were found to be quite common. Prophylactic intravenous antibiotics were not administered before the procedure as a standard protocol. Therefore, the fever rate seemed to be high in the present study. It seems that the administration of prophylactic intravenous antibiotics before STER is important. More attention should be paid, and repeated injections should be given to prevent mucosal injury. The knife should be close to the MP layer when creating a submucosal tunnel. EFR could make perforations, which might be successfully closed using clips after resecting SMTs. However, infection and fistula would occur when perforation was not completely closed. A previous study showed that the efficacy of STER and EFR in treating SMTs was comparable [24]. Further studies comparing STER and EFR are warranted for a confirmed conclusion.
Age, sex, and location would not predict en bloc resection of SMTs and AEs in the present study, while it was easier to perform en bloc resection for smaller SMTs with fewer chances of AEs, which was in accordance with previous findings [17, 19, 30]. STER for SMTs with a large size and an irregular shape should be reconsidered owing to the high risk of piecemeal resection and AEs. It was reported that longer surgical time was a risk factor for STER-related AEs [19], which was consistent with the result of this study. Patients with AEs spent more money and stayed longer in hospital compared with patients without AEs.
When STER was first reported in patients by Xu et al. in 2012 [7], a longitudinal incision was used. Since then, all studies about STER followed the incision method. An inverted T incision and a transverse entry incision were created, and a previous study showed that an inverted T entry incision was the best choice for controlling the complications related to POEM compared with a transverse entry incision and a longitudinal incision [32]. This novel study used transverse entry incision and inverted T entry incision in the STER procedure. The tunnel entrance of longitudinal incision was tight, leading to a high pressure in the tunnel and difficulty in gas discharge from the tunnel. Therefore, the entry point was modified to a transverse incision, which made it easier for the gas to get out of the tunnel. However, the closure of incision seemed much difficult. Considering the advantages and disadvantages of the aforementioned incisions, a new kind of incision, inverted T, was created which was a combination of transverse and longitudinal incisions. The incidence of AEs in the inverted T incision was lower than that in the longitudinal incision in the present study. The number of clips was fewer in the inverted T incision group than in the transverse incision group. The inverted T incision made it easier for the gas to get out of the tunnel compared with the longitudinal incision. The closure of inverted T incision was much easier compared with the transverse incision. It seemed that the inverted T incision was the best among three entry points. However, further studies on a larger population were needed to validate the findings.
The present study has several limitations. First, it was designed as a single-center, retrospective study. Second, control groups were deficient; the effectiveness and safety of STER could not be compared with those of other therapies such as ESE and EFR. A comparative study is needed for a confirmed conclusion. Third, although 89 patients were enrolled, the number of patients in 3 different incision groups was relatively small, especially in the transverse incision group. Finally, the follow-up time in the present study was quite short.
In conclusion, although STER failed to achieve en bloc resection in 21.3% patients, it was still an effective therapy owing to low residual rate and no recurrence rate after piecemeal resection. The rate of AEs was relatively high (20.8%); however, all of the AEs were cured without intervention or treated conservatively without the need for surgery. Gas-related AEs and fever were the most common AEs. Large size is a risk factor for piecemeal resection and AEs. An inverted T incision seems to be the optimum method compared with transverse and longitudinal incisions. Further prospective multicenter studies involving a large population and longer follow-up are warranted.
References
Nishida T, Kawai N, Yamaguchi S, Nishida Y (2013) Submucosal tumors: comprehensive guide for the diagnosis and therapy of gastrointestinal submucosal tumors. Dig Endos 25(5):479–489. doi:10.1111/den.12149
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8(Suppl 2):S1–41 quiz S42–44
Punpale A, Rangole A, Bhambhani N, Karimundackal G, Desai N, de Souza A, Pramesh CS, Jambhekar N, Mistry RC (2007) Leiomyoma of esophagus. Ann Thorac Cardiovasc Surg 13(2):78–81
American Gastroenterological Association I (2006) American Gastroenterological Association Institute medical position statement on the management of gastric subepithelial masses. Gastroenterology 130(7):2215–2216. doi:10.1053/j.gastro.2006.04.032
Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, Kubota T, Mukai M, Kameyama K, Sugino Y, Kumai K, Kitajima M (2006) Operative indications for relatively small (2–5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery 139(4):484–492. doi:10.1016/j.surg.2005.08.011
Wang H, Tan Y, Zhou Y, Wang Y, Li C, Zhou J, Duan T, Zhang J, Liu D (2015) Submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. Eur J Gastroenterol Hepatol 27(7):776–780. doi:10.1097/MEG.0000000000000394
Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ, Yao LQ (2012) Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc 75(1):195–199. doi:10.1016/j.gie.2011.08.018
Kim GH (2012) Endoscopic resection of subepithelial tumors. Clin Endosc 45(3):240–244. doi:10.5946/ce.2012.45.3.240
Tan Y, Lv L, Duan T, Zhou J, Peng D, Tang Y, Liu D (2016) Comparison between submucosal tunneling endoscopic resection and video-assisted thoracoscopic surgery for large esophageal leiomyoma originating from the muscularis propria layer. Surg Endosc 30(7):3121–3127. doi:10.1007/s00464-015-4567-1
Meng FS, Zhang ZH, Hong YY, Li DJ, Lin JQ, Chen X, Ji F (2016) Comparison of endoscopic submucosal dissection and surgery for the treatment of gastric submucosal tumors originating from the muscularis propria layer: a single-center study (with video). Surg Endosc 30(11):5099–5107. doi:10.1007/s00464-016-4860-7
Stavropoulos SN, Modayil R, Friedel D, Brathwaite CE (2014) Endoscopic full-thickness resection for GI stromal tumors. Gastrointest Endosc 80(2):334–335. doi:10.1016/j.gie.2014.05.300
Ye LP, Zhang Y, Wang CY, He SQ, Feng XJ, Zhang JS, Ding JX (2012) Endoscopic submucosal enucleation for gastric submucosal tumors originated from muscularis propria layer: clinical analysis of 116 case. Zhonghua Wei Chang Wai Ke Za Zhi 15(11):1175–1177
Reinehr R (2015) Endoscopic submucosal excavation (ESE) is a safe and useful technique for endoscopic removal of submucosal tumors of the stomach and the esophagus in selected cases. Z Gastroenterol 53(6):573–578. doi:10.1055/s-0034-1399384
Goto O, Uraoka T, Horii J, Yahagi N (2014) Expanding indications for ESD: submucosal disease (SMT/carcinoid tumors). Gastrointest Endosc Clin N Am 24(2):169–181. doi:10.1016/j.giec.2013.11.006
Linghu EQ, Zhang YC (2011) Experimental study on resection of the esophageal muscular propria layer by endoscopic tunnel technique. Chin J Laparoscopic Surgery(Electronic Edition) 4(5):392–393
Zhou DJ, Dai ZB, Wells MM, Yu DL, Zhang J, Zhang L (2015) Submucosal tunneling and endoscopic resection of submucosal tumors at the esophagogastric junction. World J Gastroenterol 21(2):578–583. doi:10.3748/wjg.v21.i2.578
Mao XL, Ye LP, Zheng HH, Zhou XB, Zhu LH, Zhang Y (2016) Submucosal tunneling endoscopic resection using methylene-blue guidance for cardial subepithelial tumors originating from the muscularis propria layer. Dis Esophagus. doi:10.1111/dote.12536
Lu J, Jiao T, Zheng M, Lu X (2014) Endoscopic resection of submucosal tumors in muscularis propria: the choice between direct excavation and tunneling resection. Surg Endosc 28(12):3401–3407. doi:10.1007/s00464-014-3610-y
Chen T, Zhang C, Yao LQ, Zhou PH, Zhong YS, Zhang YQ, Chen WF, Li QL, Cai MY, Chu Y, Xu MD (2016) Management of the complications of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors. Endoscopy 48(2):149–155. doi:10.1055/s-0034-1393244
Shi Q, Zhong YS, Yao LQ, Zhou PH, Xu MD, Wang P (2011) Endoscopic submucosal dissection for treatment of esophageal submucosal tumors originating from the muscularis propria layer. Gastrointest Endosc 74(6):1194–1200. doi:10.1016/j.gie.2011.07.039
Abe N, Takeuchi H, Ooki A, Nagao G, Masaki T, Mori T, Sugiyama M (2013) Recent developments in gastric endoscopic submucosal dissection: towards the era of endoscopic resection of layers deeper than the submucosa. Dig Endosc 25(Suppl 1):64–70. doi:10.1111/j.1443-1661.2012.01387.x
Walz B, von Renteln D, Schmidt A, Caca K (2011) Endoscopic full-thickness resection of subepithelial tumors with the use of resorbable sutures (with video). Gastrointest Endosc 73(6):1288–1291. doi:10.1016/j.gie.2011.01.052
Zhou PH, Yao LQ, Qin XY, Cai MY, Xu MD, Zhong YS, Chen WF, Zhang YQ, Qin WZ, Hu JW, Liu JZ (2011) Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surg Endosc 25(9):2926–2931. doi:10.1007/s00464-011-1644-y
Tan Y, Tang X, Guo T, Peng D, Tang Y, Duan T, Wang X, Lv L, Huo J, Liu D (2016) Comparison between submucosal tunneling endoscopic resection and endoscopic full-thickness resection for gastric stromal tumors originating from the muscularis propria layer. Surg Endosc. doi:10.1007/s00464-016-5350-7
Li QL, Chen WF, Zhang C, Hu JW, Zhou PH, Zhang YQ, Zhong YS, Yao LQ, Xu MD (2015) Clinical impact of submucosal tunneling endoscopic resection for the treatment of gastric submucosal tumors originating from the muscularis propria layer (with video). Surg Endosc 29(12):3640–3646. doi:10.1007/s00464-015-4120-2
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271. doi:10.1055/s-0029-1244080
Liu H, Wei LL, Zhang YZ, Sha QM, Huang Y, Qin CY, Xu HW (2015) Submucosal tunnelling endoscopic resection (STER) for the treatment of a case of huge esophageal tumor arising in the muscularis propria: a case report and review of literature. Int J Clin Exp Med 8(9):15846–15851
Zhang C, Hu JW, Chen T, Zhou PH, Zhong YS, Zhang YQ, Chen WF, Li QL, Yao LQ, Xu MD (2015) Submucosal tunneling endoscopic resection for upper gastrointestinal multiple submucosal tumors originating from the muscular propria layer: a feasibility study. Indian J Cancer 51(Suppl 2):e52–55. doi:10.4103/0019-509X.151989
Liu BR, Song JT (2016) Submucosal tunneling endoscopic resection (STER) and other novel applications of submucosal tunneling in humans. Gastrointest Endosc Clin N Am 26(2):271–282. doi:10.1016/j.giec.2015.12.003
Chen T, Zhou PH, Chu Y, Zhang YQ, Chen WF, Ji Y, Yao LQ, Xu MD (2017) Long-term outcomes of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors. Ann Surg 265(2):363–369. doi:10.1097/SLA.0000000000001650
Wang XY, Xu MD, Yao LQ, Zhou PH, Pleskow D, Li QL, Zhang YQ, Chen WF, Zhong YS (2014) Submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a feasibility study (with videos). Surg Endosc 28(6):1971–1977. doi:10.1007/s00464-014-3420-2
Ma XB, Linghu EQ, Li HK, Zhai YQ, Chai NL, Peng LH, Wang XD, Du H, Meng JY, Wang HB, Zhu J, Guo MZ, Wang XX, Lu ZS (2016) Factors affecting the safety and efficacy of peroral endoscopic myotomy for achalasia. Nan Fang Yi Ke Da Xue Xue Bao 36(7):892–897
Acknowledgements
This study was supported by research grants from two Chinese People’s Liberation Army General Hospital Clinical Researches (2012FC-TSYS-3035 and YS201404).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chen Du, Lianjun Ma, Ningli Chai, Ying Gao, Xiaotong Niu, Yaqi Zhai, Zhenjuan Li, Jiangyun Meng, Ping Tang and Enqiang Linghu have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Du, C., Ma, L., Chai, N. et al. Factors affecting the effectiveness and safety of submucosal tunneling endoscopic resection for esophageal submucosal tumors originating from the muscularis propria layer. Surg Endosc 32, 1255–1264 (2018). https://doi.org/10.1007/s00464-017-5800-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5800-x