Abstract
Background
Submucosal tunneling endoscopic resection (STER) has been proved to be safe and effective for removal of esophageal leiomyoma originating from the muscularis propria (MP) layer. However, there are still technical challenges for tumors ≥35 mm due to the limited space of the submucosal tunnel. The aim of the study was to estimate the safety and efficacy of STER for large esophageal leiomyoma originating from the MP layer as well as compare its efficacy with video-assisted thoracoscopic surgery (VATS), which is a standard procedure for treating esophageal leiomyoma.
Methods
We retrospectively collected the clinical data of the patients with esophageal leiomyoma of 35–55 mm who underwent STER or VATS at our hospital between January 2010 and December 2014. Epidemiological data (gender, age), tumor location, tumor size, procedure-related parameters, complications, length of stay and cost were compared between STER and VATS.
Results
A total of 31 patients were enrolled, and 18 patients underwent STER and the other 13 received VATS. There was no significant difference between the two groups in gender, age, tumor location, tumor size, complications and rate of en bloc resection (P > 0.05). However, patients in the STER groups had a shorter operation time, a less decrease in hemoglobin level, a shorter length of hospital stay and a decreased cost (P < 0.05). No recurrence was noted in the STER and VATS groups during a mean follow-up of 10.9 and 30.8 months, respectively.
Conclusions
The treatment efficacy was comparable between the STER and VATS for esophageal leiomyoma of 35–55 mm. However, STER is superior to VATS in a shorter operation time, a less decrease in hemoglobin level, a shorter length of hospital stay and a decreased cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal leiomyoma is one of the most common submucosal tumors (SMTs) and is usually benign and asymptomatic, but it should be resected if the tumor is too large or symptomatic [1]. Current methods to remove a leiomyoma include surgery and endoscopic resection [2]. Surgery via thoracoscopic approach is usually recommended because it has a shorter hospital stay and less invasive compared with thoracotomy [3]. Although endoscopic resection such as endoscopic submucosal dissection (ESD), endoscopic submucosal excavation (ESE) and endoscopic full-thickness resection (EFR) has been regarded as minimally invasive resection methods for leiomyoma [4, 5], they can be unsatisfactory sometimes due to incomplete resection or risk of perforation during procedure.
STER, also called submucosal endoscopic tumor resection (SET) or tunneling endoscopic muscularis dissection (tEMD), has emerged as a new technique for treating esophageal leiomyoma and shown exciting results [6–13]. This new endoscopic technique has advantages over ESD in terms of maintaining the integrity of the digestive tract mucosa, promoting rapid wound healing and reducing the operating time without any compromise in success rate or increase in complications [11]. For SMTs >10 mm, STER is a preferable choice in terms of preventing air leakage symptoms compared with ESE [12]. However, due to the limited space of the submucosal tunnel, most researchers recommended a maximum resectable lesion size of 35 mm [7–9]. What is more, little is known about the comparison between STER and surgical methods. We report our preliminary experience of STER for esophageal leiomyoma of 35–55 mm as well as compare its efficacy with video-assisted thoracoscopic surgery (VATS) in this study.
Patients and methods
Patients
This is a single center, retrospective study conducted in China. The study was approved by the ethics committee of the Second Xiangya Hospital of Central South University. The inclusion criteria for enrollment in the study were as follows: (a) The presence of an esophageal SMT originating from the MP layer confirmed by computerized tomography (CT) and EUS (UM-2R, 12 MHz; UM-3R, 20 MHz; Olympus, Tokyo, Japan), and diagnosed of leiomyoma histologically; (b) the diameter of the leiomyoma was 35–55 mm; (c) a Zubrod–ECOG performance status 0 or 1; and (d) patients consent to undergo an STER or VATS procedure at our hospital. Informed consent was obtained from all patients before the procedure was performed. All patients were informed of possible adverse events (pneumothorax, subcutaneous emphysema, massive bleeding, incomplete resection, postoperative leaks, etc.) and other possible treatment options.
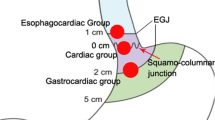
Epidemiological data (gender, age), tumor location, tumor size, procedure-related parameters (operative time, en bloc resection rate), complications, decrease in hemoglobin level, length of stay and cost were recorded and analyzed between the two methods. Tumors were classified according to their location along the esophagus, relative to the incisor teeth: Upper esophageal lesions were defined as those 15–23 cm from the incisors, middle esophageal lesions as those 24–32 cm from the incisors and lower esophageal lesions as those >32 cm from the incisors.
STER procedure
STER was performed under general anesthesia via tracheal intubation using a single-channel endoscopy (GIF-Q260 J; Olympus, Tokyo, Japan) with a transparent cap (D-201-11802, Olympus, Japan) attached to the front. Carbon dioxide insufflator (UCR; Olympus, Japan) was used. STER was performed the same as in our previous reports [14]. Briefly, the procedure was as follows: (1) A fluid cushion was made by submucosal injection (a mix solution of 100 ml saline + 2 ml indigo carmine + 1 ml epinephrine) at about 3–5 cm proximal to the SMT; (2) to create tunnel entry, a longitudinal mucosal incision over 2 cm was made using a dual knife or a hybrid knife and then a following submucosal dissection for at least 0.5 cm along both sides of the longitudinal incision; (3) a submucosal tunnel was made with a dual knife between the submucosal and muscular layers; (4) dissecting the tumor with a hybrid knife, a IT knife or a dual knife; and (5) close the mucosal entry with several clips after the tumor was removed. Figures 1, 2 and video 1 depict an example of STER.
Case illustration of STER. a Submucosal tumor located in the esophagus. b EUS showed a tumor originating from the muscularis propria layer. c Dissection was made along the margin of the tumor within the tunnel. d The entire exposed tumor after endoscopic dissection. e Tunnel entry was closed with several clips. f The specimen resected
VATS procedure
The VATS procedure was performed under general anesthesia with double-lumen intubation. The patient is placed in a right or left lateral decubitus position at about a 15° frontal incline. A right VATS was performed for tumors located in the upper two-thirds of esophagus and a left VATS for those of the lower thirds of the esophagus. VATS was performed as reported [3] briefly: A 3- or 4-port placement was chosen based on the preference of the operator. After localization of the tumor, the mediastinal pleura was incised longitudinally, and a myotomy was performed over the tumor. The tumor was removed gently to prevent mucosal damage. The muscle layer is re-approximated, and a 28- or 32-Fr chest tube is placed through one of the ports for postoperative drainage.
Postoperative management
For patients received STER, they were kept NPO for 24 h, a liquid diet for 3 days and returning gradually to a normal diet within 2 weeks. At Day 2 post-operation, thoracoabdominal X-ray was performed to check for the occurrence of emphysema, pneumothorax, pneumoperitoneum, pleural effusion, etc. For patients received VATS, they were kept NPO for 48 to 72 h, a liquid diet for 3 days, a soft diet for 2 weeks and then a normal diet. An esophagography was performed at 5–7 days after surgery, and the chest tube was removed once we confirmed the mucosal integrity. Intravenous proton pump inhibitor (PPI) and antibiotics were used for at least 3 days for all patients.
Pathological evaluation
The specimens were fixed, embedded with paraffin and then sectioned. Hematoxylin and eosin and immunohistochemical staining (CD34, CD117, S-100, desmin, SMA, Ki67, Dog-1) were carried out. En bloc resection was defined as the intact fibrous capsule of the resected tumor and the absence of any remnant of tumor observed on endoscopy.
Follow-up
Surveillance endoscopy or barium swallow was performed at 1, 6 and 12 months and annually thereafter to observe healing of the wound and check for any residual tumor.
Statistical analysis
SPSS 17.0 software was applied for data analysis. Continuous variables were presented as mean ± standard deviation and analyzed using Student’s t test. And qualitative data were presented as frequencies and calculated using the Chi-square test or Fisher’s exact test. A two-tailed p value <0.05 was considered as statistically significant in all cases.
Results
Clinical characteristics and therapeutic outcome
A total of 31 patients were enrolled in this study from January 2010 to December 2014, of whom the mean age was 42.6 years (range 22–64 years), and the male/female ratio was 21:10. Of the 31 SMTs, 4 were located in the upper esophagus, 16 in the middle esophagus and 11 in the lower esophagus. The mean tumor size was 40.6 mm (range 35–53 mm), and all of them were diagnosed of leiomyoma. Eighteen cases received STER and the other 13 cases received VATS. There was no significant difference between the two groups in gender, age, tumor location and tumor size (P > 0.05, Table 1). However, patients in the STER groups had a shorter operation time, a shorter length of hospital stay and a decreased cost (P < 0.05, Table 1). En bloc resection was achieved in 88.9 % (16/18) of the cases in the STER group and 100 % (13/13) in the VATS group, and there was no significance (P > 0.05). In case 2 and case 15 of STER, en bloc resection was failed because the tumor was too large (53 × 30 × 18 mm and 43 × 25 × 12 mm, respectively), tumor fragmentation was needed for successful extraction of the two tumors. A total of 22 cases (13 in the STER group and 9 in the VATS group) had paired blood text before and within 48 h after surgery, and the decrease in hemoglobin level was greater in the VATS group (P < 0.05, Table 1).
Complications and follow-up
Three patients (16.7 %) in the STER group and 2 patients (15.4 %) in the VATS group had complications, and there was no significant difference (P > 0.05, Table 1). In the STER group, case 3 suffered from subcutaneous emphysema and it absorbed spontaneously within 3 days; case 7 suffered chest pain and it remitted within 3 days; case 14 encountered mucosa laceration while extracting the tumor and a metal stent was inserted. Repeated endoscopy and removal of the stent 7 days later revealed closure of the mucosal injury. In the VATS group, two cases suffered from mucosal injury intraoperatively and the mucosa were repaired with interrupted sutures. No esophageal leaks, delayed bleeding or other severe complications occurred during or after the procedure. No recurrence was noted during periodical follow-up.
Discussion
In the present study, we successfully managed 18 cases with esophageal leiomyoma of 35–55 mm by the STER technique without major complication. This indicates that STER is feasible, safe and effective for large esophageal leiomyoma originating from the MP layer. What is more, we demonstrated that STER takes advantages to VATS in a shorter operation time, a less decrease in hemoglobin level, a shorter length of hospital stay and a decreased cost, although their efficacy was the same. As far as we know, this is the first study about comparison between STER and VATS.
However, concerning that some of the SMTs do have malignant potential, especially when they originate from the MP layer or with a large diameter [15], a comprehensive preoperative assessment is necessary for STER. In the present study, all the 18 patients underwent preoperative esophagogastroscopy (EGD), EUS and CT. Because imagery, EGD and clinical examination suggested a benign tumor in all the 18 cases, we did not perform fine-needle aspiration in any of the cases [15–17]. In our experience, STER can be an alternative for large leiomyoma only when they adhere to the following characteristics: (a) EGD reveals an intact mucosal surface without ulceration or erosion at the site of tumor location; (b) EUS examination shows no high-risk features, such as irregular border, internal heterogeneity including anechoic area (i.e., necrosis) and echogenic loci (i.e., bleeding), heterogeneous enhancement and regional lymph node swelling; (c) no signs of metastasis are noted during a CT examination; and (d) patients consent to undergo a STER procedure and sign an informed consent. Those who are unwilling to do or intolerable to an open/laparoscopic surgery may have an attempt to STER as well.
The feasibility of STER for leiomyoma ≥35 mm was also reported by a few researchers. Kumbhari et al. [18] resected a giant esophageal leiomyoma (60 × 28 × 22 mm) by STER; fragmentation was needed for successful extraction of the lesion. Inoue et al. [6] failed to remove two large SMTs (75 × 42 × 35 mm and 60 × 55 × 45 mm, respectively), and conversion to surgery was necessary. Gong et al. [10] reported a maximum diameter of 40 mm in their retrospective study; en bloc resection was failed. Wang et al. [11] reported a maximum diameter of 45 mm in their retrospective study. Tan et al. [19] reported a case of 52-mm esophageal leiomyoma en bloc resected by STER. In the present study, the mean size of the lesion was 40.6 mm (range 35–53 mm), and en bloc resection was achieved in 16 of the 18 cases, and no recurrence was noted during periodical follow-up. In our opinion, there are several points that may facilitate an en bloc resection: (a) General anesthesia via tracheal intubation with muscle relaxants are recommended, as it can suppress the contraction of muscle and reduce the resistance of the upper esophagus, which may be helpful for removal of large SMTs through the narrow upper esophagus and esophagopharyngeal junction. (b) The tunnel orifice should be at least 2 cm and increased to the size of the short dimension of the tumor, after mucosal incision; a following submucosal dissection for at least 0.5 cm along both sides of the longitudinal incision is recommended to provide an ample submucosal space for tumor extraction as well as gas diffusion [20]. (c) We recommend a minimum tunnel width of 3 cm. The width of tunnel should expand according to the diameter of SMTs, which facilitates submucosal dissection and gas diffusion. (d) The tumor should be exposed clearly. The tunnel should extend at least 2 cm beyond the tumor, to ensure a satisfactory endoscopic view of the SMT and enough working space for resection. (e) Complete resection without interruption of the tumor capsule is recommended. For a SMT originates from deep MP layer or has a tight connection with the underlying MP or serosal layer, a full-thickness resection including the lesion, its underlying MP and serosa is generally performed. f) After removal of SMTs, the wound surface should be washed repeatedly to reduce the chance of residual tumor cells. (g) While removing the tumor, the tumor is grasped in a fashion as to have its long dimension parallel to the long axis of the esophagus and its short dimension transversely and extract it from the tunnel through the tunnel orifice and the UES in a straightforward way as possible as we could. (h) If preoperative imagery, EGD and clinical examination suggested a benign tumor, we can use a snare after completion of the resection to cut the tumor in 2 or more pieces (while in the tunnel) so that it could then be easily extracted from the tunnel. (i) Another approach is to create a second “window” either in the area of tumor or by a distal mucosal incision to may facilitate en bloc extraction for large leiomyoma [21, 22].
Limitations of the present study include its retrospective design and relative small sample, thus warranting a prospective, large and randomized study. In conclusion, this preliminary study has shown that the STER technique is feasible and appears to be safe and effective for esophageal leiomyoma of 35–55 mm. The treatment efficacy was comparable between the STER and VATS for esophageal leiomyoma of 35–55 mm. However, STER is superior to VATS in a shorter operation time, a less decrease in hemoglobin level, a shorter length of hospital stay and a decreased cost.
References
Punpale A, Rangole A, Bhambhani N, Karimundackal G, Desai N, de Souza A, Pramesh CS, Jambhekar N, Mistry RC (2007) Leiomyoma of esophagus. Ann Thorac Cardiovasc Surg 13(2):78–81
Kim GH (2012) Endoscopic resection of subepithelial tumors. Clin Endosc 45(3):240–244
Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J (2014) Enucleation of esophageal submucosal tumors: a single institution’s experience. Ann Thorac Surg 97(2):454–459
Shi Q, Zhong YS, Yao LQ, Zhou PH, Xu MD, Wang P (2011) Endoscopic submucosal dissection for treatment of esophageal submucosal tumors originating from the muscularis propria layer. Gastrointest Endosc 74(6):1194–1200
Lu J, Lu X, Jiao T, Zheng M (2014) Endoscopic management of upper gastrointestinal submucosal tumors arising from muscularis propria. J Clin Gastroenterol 48(8):667–673
Inoue H, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, Maselli R, Kudo S (2012) Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy 44(3):225–230
Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ, Yao LQ (2012) Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc 75(1):195–199
Liu BR, Song JT, Kong LJ, Pei FH, Wang XH, Du YJ (2013) Tunneling endoscopic muscularis dissection for subepithelial tumors originating from the muscularis propria of the esophagus and gastric cardia. Surg Endosc 27(11):4354–4359
Ye LP, Zhang Y, Mao XL, Zhu LH, Zhou X, Chen JY (2014) Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg Endosc 28(2):524–530
Gong W, Xiong Y, Zhi F, Liu S, Wang A, Jiang B (2012) Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy 44(3):231–235
Wang L, Ren W, Zhang Z, Yu J, Li Y, Song Y (2013) Retrospective study of endoscopic submucosal tunnel dissection (ESTD) for surgical resection of esophageal leiomyoma. Surg Endosc 27(11):4259–4266
Lu J, Jiao T, Zheng M, Lu X (2014) Endoscopic resection of submucosal tumors in muscularis propria: the choice between direct excavation and tunneling resection. Surg Endosc 28(12):3401–3407
Wang H, Tan Y, Zhou Y, Wang Y, Li C, Zhou J, Duan T, Zhang J, Liu D (2015) Submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. Eur J Gastroenterol Hepatol 27(7):776–780
Chen H, Xu Z, Huo J, Liu D (2015) Submucosal tunneling endoscopic resection for simultaneous esophageal and cardia submucosal tumors originating from the muscularis propria layer (with video). Dig Endosc 27(1):155–158
Nishida T, Kawai N, Yamaguchi S, Nishida Y (2013) Submucosal tumors: comprehensive guide for the diagnosis and therapy of gastrointestinal submucosal tumors. Dig Endosc 25(5):479–489
Tsai SJ, Lin CC, Chang CW, Hung CY, Shieh TY, Wang HY, Shih SC, Chen MJ (2015) Benign esophageal lesions: endoscopic and pathologic features. World J Gastroenterol 21(4):1091–1098
Salah W, Faigel DO (2014) When to puncture, when not to puncture: submucosal tumors. Endosc Ultrasound 3(2):98–108
Kumbhari V, Saxena P, Azola A, Messallam AA, El ZMH, Khashab MA (2015) Submucosal tunneling endoscopic resection of a giant esophageal leiomyoma. Gastrointest Endosc 81(1):219–220
Tan Y, Liu D (2015) En bloc submucosal tunneling endoscopic resection for a giant esophageal leiomyoma. Gastrointest Endosc 82(2):399
Wang X, Tan Y, Zhang J, Liu D (2015) Risk factors for gas-related complications of peroral endoscopic myotomy in achalasia. Neth J Med 73(2):27–32
Tan Y, Zhu H, Lv L, Liu D (2015) Enlarging an accidental mucosotomy to facilitate tumor extraction during submucosal tunneling endoscopic resection for a giant esophageal leiomyoma. Gastrointest Endosc. doi:10.1016/j.gie.2015.07.024
Ng JJ, Chiu PW, Shabbir A, So JB (2015) Removal of a large, 40-mm, submucosal leiomyoma using submucosal tunneling endoscopic resection and extraction of specimen using a distal mucosal incision. Endoscopy 47(Suppl 1):E232-3
Acknowledgments
This study was funded by Development and Reform Commission of Hunan Province (XFGTZ2014713).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Deliang Liu, Yuyong Tan, Liang Lv, Tianying Duan, Junfeng Zhou, Yao Tang and Dongzi Peng declare no conflict of interests for this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 137288 kb)
Rights and permissions
About this article
Cite this article
Tan, Y., Lv, L., Duan, T. et al. Comparison between submucosal tunneling endoscopic resection and video-assisted thoracoscopic surgery for large esophageal leiomyoma originating from the muscularis propria layer. Surg Endosc 30, 3121–3127 (2016). https://doi.org/10.1007/s00464-015-4567-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4567-1