Abstract
This is the first study to explore the effects of crosstalk from 3D laparoscopic displays on technical performance and workload. We studied crosstalk at magnitudes that may have been tolerated during laparoscopic surgery. Participants were 36 voluntary doctors. To minimize floor effects, participants completed their surgery rotations, and a laparoscopic suturing course for surgical trainees. We used a counterbalanced, within-subjects design in which participants were randomly assigned to complete laparoscopic tasks in one of six unique testing sequences. In a simulation laboratory, participants were randomly assigned to complete laparoscopic ‘navigation in space’ and suturing tasks in three viewing conditions: 2D, 3D without ghosting and 3D with ghosting. Participants calibrated their exposure to crosstalk as the maximum level of ghosting that they could tolerate without discomfort. The Randot® Stereotest was used to verify stereoacuity. The study performance metric was time to completion. The NASA TLX was used to measure workload. Normal threshold stereoacuity (40-20 second of arc) was verified in all participants. Comparing optimal 3D with 2D viewing conditions, mean performance times were 2.8 and 1.6 times faster in laparoscopic navigation in space and suturing tasks respectively (p< .001). Comparing optimal 3D with suboptimal 3D viewing conditions, mean performance times were 2.9 times faster in both tasks (p< .001). Mean workload in 2D was 1.5 and 1.3 times greater than in optimal 3D viewing, for navigation in space and suturing tasks respectively (p< .001). Mean workload associated with suboptimal 3D was 1.3 times greater than optimal 3D in both laparoscopic tasks (p< .001). There was no significant relationship between the magnitude of ghosting score, laparoscopic performance and workload. Our findings highlight the advantages of 3D displays when used optimally, and their shortcomings when used sub-optimally, on both laparoscopic performance and workload.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
During three-dimensional (3D) laparoscopy, surgeons wear lightweight glasses that polarize horizontal rows of pixels displayed on a 3D monitor, with each row alternating between images captured by individual right and left cameras. As left-camera images are blocked by right-eye glasses and vice versa, each eye ideally receives a complete image from its respective camera. Crosstalk refers to the leakage of visual information from the 3D glasses, whereby each eye sees a mixture of the image intended for that eye, and some of the image intended for the other eye [1]. Crosstalk is precipitated by suboptimal viewing positions including head tilt from display elevation (looking up or down at the screen) and acute eccentric viewing angles (looking sideways at the screen). Depending on the severity of suboptimal viewing, crosstalk may manifest as subtle visual ghosting of images, or, in severe cases, images will appear similar to viewing the 3D display without 3D glasses. The effects of crosstalk include reduced stereovision, headache and fatigue [1, 2].
Despite the rising popularity of 3D laparoscopic technologies,[1–4] crosstalk is not widely appreciated in the surgical community. The impact of crosstalk on 3D laparoscopic performance has not been previously reported. The primary aim of this study was to systematically evaluate the effects of crosstalk by comparing the technical performance and workload from using 2D and 3D laparoscopic displays in optimal and suboptimal viewing conditions. In this study, participants calibrated their exposure to crosstalk such that in the optimal 3D condition, no ghosting was perceived. In the suboptimal viewing condition, crosstalk was calibrated by each participant to the maximum level of ghosting that could be tolerated without discomfort during laparoscopy. As tolerable levels may vary between participants, our secondary aim was to explore the relationship between the magnitude of perceived ghosting and laparoscopic performance.
Methods
Study design
We used a counterbalanced, within-subjects design in which participants were randomly assigned to complete laparoscopic tasks in one of six unique testing sequences. Three viewing conditions were evaluated: 2D, 3D with/without ghosting.
Participants
Thirty-six voluntary individuals with a mean age of 30.5 years took part in the study. Participants were junior doctors from The University of Queensland Surgical Interest Group, and were the first 36 respondents from advertisements placed on the Surgical Interest Group webpage. All participants had previously completed a laparoscopic suturing course for surgical trainees taught by a surgeon instructor at the Clinical Skills and Development Centre (CSDS), Brisbane, Australia. All participants had completed their surgical rotations and were also experienced in laparoscopic assisting. A recent cross-sectional study of surgeons suggests that 10% may be stereoblind [5]. We therefore verified normal threshold stereoacuity (40 − 20 s of arc) in all participants using the Randot® Stereotest (Stereo Optical, Chicago, IL, USA).
Testing laparoscopic performance with 2 simulation tasks
Navigating in space (Fig. 1)
We used a custom apparatus developed to test fine levels of laparoscopic depth perception. This task tests fine instrument control with a needle in 3D space, under time pressure. Participants were required to hold a laparoscopic needle holder with their dominant hand, and pass a curved needle fixed in its jaws through a 2 mm loop at the tip of a monofilament suture. The apparatus incorporated five such loops that participants were required to complete in a predetermined sequence. The time taken for the needle to pass through all five loops was recorded with a stopwatch.
Laparoscopic suturing
We used a standard Fundamentals of Laparoscopic Surgery Suturing task module. This task tests fine instrument control with a needle and suture, as well as suturing technique in 3D space, under time pressure. Participants were required to handle one laparoscopic needle holder with each hand, and manipulate a curved needle on a 12-cm-long 3.0 Prolene suture to repair a defect in a rubber tube. A black dot on the edge of each defect indicated where the suture must enter and exit. The time taken for a complete and flat laparoscopic knot (two, then one and then one throw) was recorded with a stopwatch.
For each viewing condition (2D, 3D with/without ghosting), participants had to perform three repetitions of each simulation task before moving on to the next predetermined viewing condition. For each participant, the mean time for each simulation task was used for data analysis.
The national aeronautics and space administration task load index (NASA TLX)
Workload is a term used in human factors science to describe the cost incurred by an individual during work activity. The NASA TLX questionnaire was initially developed to analyse the workload of pilots with the aim of redesigning processes to reduce technical errors, and has become the gold standard of workload assessment owing to its extensive validation in different industries. The NASA TLX has also been used to measure the workload of surgeons and physicians trialling new procedures and technologies designed to improve work efficiency and performance [6–9].
Laparoscopy display systems
Target images were captured by the Olympus Endoeye Flex 3D laparoscope with left and right images relayed to individual Olympus CV-190 processors. The Olympus 3DV-190 visualization unit integrates these images to display a 3D image on a compatible Sony LMD-2451MT LCD HDTV monitor. (Olympus Co, Tokyo, Japan; Sony Corporation, Tokyo, Japan). The LCD panel has a high resolution (1900 × 1200 dots) and the monitor dimensions are 23 ¾ × 15 ¼ inches. The monitor is intended for medical use only. Target images can be displayed in both 2D and 3D with the same set-up.
Grading of visual ghosting
We used magnitude estimation, a standard psychophysical procedure in which participants graded the intensity of visual ghosting on a scale of 0 to 100 [2]. Participants were instructed that 0 = no ghosting and 100 = ghosting identical to viewing the 3D display without 3D glasses.
Viewing positions
During testing in the 2D and 3D (without ghosting) conditions, each participant was tested in the optimal viewing position in which the centre of the plane of the display was adjusted perpendicular to the viewer’s line of sight. Participants confirmed the absence of visual ghosting in the 3D (without ghosting) condition. Viewing distance was 1 m and was taken as the straight distance from the back of the participant’s heels to the mid-point of a horizontal line on the floor parallel to the plane of the display monitor.
We have previously demonstrated that head height underneath the 3D display monitor produced a visual ghosting grade of 100 in most viewers [2]. Primary operating positions that conventionally adopt this suboptimal position include laparoscopic-assisted colorectal operations such as total mesorectal excision (taTME) and transanal minimally invasive surgery (TAMIS). In 3D (with tolerable ghosting condition), display monitor height (elevation) was raised relative to the optimal viewing position to generate increasing amounts of crosstalk. At the start of this condition, participants were instructed to calibrate the maximum level of ghosting that they could accept without discomfort. Participants were able to control the amount of crosstalk by adjusting display elevation. To provide clinical context, participants were also instructed to imagine that this was also the level of ghosting that they would allow 3D laparoscopic surgeons to operate on themselves (if the participants were patients).
Procedure
The testing procedure was approved by the University of Queensland (UQ) Human Ethics Committee and the Program Director of the UQ School of Medicine. Participants were individually tested.
To eliminate order bias, participants were randomly assigned into one of six possible combinations of viewing conditions (e.g. First: 3D without ghosting; second: 2D; last: 3D, with tolerable ghosting). Participants then completed the tasks in an order determined by random assignment to one of six counterbalanced testing sequences (6 participants per sequence). Random assignment was performed using a computerized random number generator. The 6 sequences comprised a factorial combination of three viewing mode orders (applied to each individual technical task; testing mode: 2D/3D without ghosting/3D with ghosting or 2D/3D with ghosting/3D without ghosting or 3D without ghosting/2D/3D with ghosting or 3D without ghosting /3D with ghosting/2D or 3D with ghosting/2D/3D without ghosting or 3D with ghosting/3D without ghosting/2D).
The order of laparoscopic technical tasks was predetermined by increasing difficulty: needle threading and lastly suturing. Each participant was required to complete three repetitions of the navigating in space task, and then three repetitions of laparoscopic suturing before moving on to the next viewing condition.
Statistical analysis
Data were analysed using SPSS® version 22 (IBM, Armonk, New York, USA) with alpha set at 0.05. First, a repeated measures analyses of variance (ANOVA) was conducted on performance and workload data to assess the effects of viewing mode (2D vs. 3D without ghosting vs. 3D with ghosting). For each participant, the mean performance in each simulation task was used for data analysis. Each significant interaction was followed-up with simple effects tests (paired t-tests) to compare the effects of laparoscopic task (navigation in space and laparoscopic suturing) and laparoscopic display (2D, 3D with/without ghosting). The effects of subjective intensity of tolerable ghosting on laparoscopic performance and workload were examined with Pearson correlation coefficients and alpha was adjusted using the Bonferroni correction.
Results
Stereoacuity
Normal threshold stereoacuity (60 − 20 s of arc) was verified in all participants using the Randot® Stereotest (Stereo Optical, Chicago, IL, USA).
Grading of visual ghosting
The median and modal grade of visual ghosting across all participants, in which they reported the maximum level of ghosting that they could tolerate without discomfort, were 15 and 10, respectively.
Laparoscopic performance
Using repeated measures analyses of variance on the laparoscopic performance data, we found that laparoscopic performance was significantly different between 2D, 3D without ghosting and 3D with ghosting conditions (F (1.35) = 39.5, p < .001). As expected, we also found that laparoscopic performance was significantly different between navigating in space and suturing tasks (F (1.35) = = 73.9 p < .001).
Laparoscopic performance in navigating in space and suturing tasks, using 2D, optimal 3D and 3D displays with tolerable ghosting, is presented in Fig. 2.
A–B Group performance data for participants. Y axis—time in seconds. 2D—two-dimensional laparoscopic display. 3DX—three-dimensional laparoscopic display with tolerable levels of ghosting from crosstalk. 3D—optimal three-dimensional display. X axis—three laparoscopic conditions: 2D; 3DX and 3D. 2A: Performance related to navigating in space technical task. 2B: Performance related to suturing technical task
For the navigating in space task, mean performance time was 2.8 times faster in the optimal 3D condition (36.6 s, Std. error 2.3 s) than in 2D (101.8 s, Std.error 7.1 s, p < .001) and was 2.9 times faster in optimal 3D viewing than 3D viewing with tolerable ghosting (104.69 s, Std. error 12.3 s, p < .001). There was no significant difference between 3D viewing with tolerable ghosting and 2D (p = .83).
For the laparoscopic suturing task, mean performance time was 1.6 times faster in the optimal 3D condition (118.8 s, Std. error 7.3 s) than in 2D (184.3 s, Std.error 11.6 s, p < .001) and was 2.9 times faster than 3D viewing with tolerable ghosting (212.7 s, Std. error 19.3 s, p < .001). There was no significant difference in performance time between 3D viewing with tolerable ghosting and 2D (p = .06).
Using a Pearson correlation analysis, we found no relationship between subjective intensity of tolerable ghosting on laparoscopic performance in the conditions described above.
Laparoscopic workload
Using repeated measures analyses of variance on the laparoscopic workload data, we found that the workload among participants was significantly different between 2D, 3D without ghosting and 3D with ghosting conditions (F (1.35) = 47.73, p < .001). We also found that the workload among participants was significantly different between navigating in space and suturing tasks (F (1.35) = 9.78, p = .03).
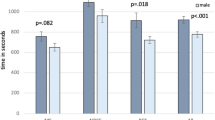
Laparoscopic workload associated with navigating in space and suturing tasks, using 2D, optimal 3D and 3D displays with tolerable ghosting, is presented in Fig. 3.
A–B. Group workload data for participants. Y axis—NASA TLX score. 2D—two-dimensional laparoscopic display. 3DX—three-dimensional laparoscopic display with tolerable levels of ghosting from crosstalk. 3D—optimal three-dimensional display. X axis—three laparoscopic conditions: 2D; 3DX and 3D. 3A: Workload related to navigating in space technical task. 3B: Workload related to suturing technical task
For the navigating in space task, mean reported workload was 1.5 times higher in 2D (65.2, Std. error 2.8) than in the optimal 3D condition (44.7, Std.error 2.8, p < .001). Mean workload was 1.3 times higher in 3D viewing with tolerable ghosting than optimal 3D viewing (63.1, Std. error 2.3, p < .001). There was no significant difference in workload between 3D viewing with tolerable ghosting and in 2D (p = .48).
For laparoscopic suturing, mean workload was 1.3 times higher in 2D (68.7, Std. error 2.9) than in the optimal 3D condition (54.3, Std.error 2.9, p < .001). Mean workload was 1.3 times higher in 3D viewing with tolerable ghosting than optimal 3D viewing (72.8, Std. error 2.0, p < .001). There was no significant difference in workload between 3D viewing with tolerable ghosting and 2D (p = .08).
Discussion
This novel simulation-based study has systematically evaluated the effects of crosstalk during 3D laparoscopy by comparing the technical performance and workload in optimal and suboptimal viewing conditions. Specifically, this study evaluated mild intensities of crosstalk that may potentially be tolerated by surgeons during real-world 3D laparoscopy.
First, this study has demonstrated that in terms of technical performance and workload, there was no significant difference between 2D displays and suboptimally used 3D displays. Our findings may help explain how prior trials may have underestimated the full benefit of modern laparoscopic 3D displays [1].
Second, this study has shown that under optimal conditions, laparoscopic 3D displays offer considerable advantages over 2D displays. When tested in optimal 3D viewing conditions, mean performance times were 2.8 and 1.6 times faster in navigating in space and suturing tasks, respectively; mean workload in the 2D viewing condition was 1.5 and 1.3 times greater than in the optimal 3D condition, for navigating in space and suturing tasks, respectively.
Third, this study has shown that 3D displays in optimal conditions offer significant and considerable performance, and workload improvements over suboptimally used 3D displays, even though the calibrated levels of ghosting were mild, and not perceived as unsafe or uncomfortable. The majority of participants could tolerate a visual ghosting grade of 10 without any discomfort, where a grade of 100 consisted of an image identical to viewing the 3D display without 3D glasses. In the optimal 3D viewing condition, mean performance time was 2.9 times faster in optimal than suboptimal 3D conditions, in both navigating in space and suturing tasks. Mean workload in the suboptimal 3D condition was 1.3 times greater than the optimal 3D condition, in both laparoscopic tasks. We could not find a significant relationship between the magnitude of ghosting score, laparoscopic performance and workload. Put together, these results suggest that any level of ghosting, if encountered, should not be accepted.
The ideal position to view a 3D display is where the viewer’s line of sight is perpendicular to, and at the centre of, the plane of the display [2]. However, this position is not always adopted by surgeons during laparoscopic surgery, in which viewing locations often change according to the stage and physical constraints of an operation. Members of a surgical team usually share visual information from a common display monitor, and primary surgeons may compromise the ideal viewing position so that the camera assistant, assisting surgeons and scrub nurses (all having unique heights, elevations and horizontal (left/right) deviations) may also visualize the screen [2]. The operating positions that conventionally adopt variations of the suboptimal position used in our study include laparoscopic-assisted colorectal operations such as transanal total mesorectal excision (taTME) and transanal minimally invasive surgery (TAMIS). In all of the above operations, surgeon crosstalk exposure during 3D laparoscopy can be avoided by raising the operating table such that the surgeon stands in the optimal position whilst working. Surgeons may elect to tilt the screen downwards (directly facing the seated surgeon) to minimize the crosstalk that they experience. However, this orientation will only exaggerate the crosstalk experienced by other standing team members due to the incorrect orientation of their polarizing glasses to the display. The use of platforms and separate displays for team members grouped in outlying positions should also be actively encouraged.
This study has limitations. We could not purposefully evaluate the negative effects of crosstalk during actual operations as surgeons and patients would be purposefully exposed to suboptimal conditions. We were thus unable to conduct a clinical study and used patient-centred metrics of laparoscopic performance. Instead, we conducted our study in a simulation laboratory, in which study variables were systematically and strictly controlled. However, we acknowledge that there is yet no simulation task specifically validated for 3D laparoscopy. This is due to the absence of performance metrics among participants with different stereoscopic abilities controlled for laparoscopic experience, viewing distance, viewing elevation and horizontal viewing eccentricity [1]. Another limitation of this study was that the crosstalk encountered in our experiment was produced exclusively from differences in screen height (and not from differences in horizontal viewing angles which may also produce crosstalk [2]). Furthermore, in the 3D with crosstalk condition, display height was not the same as the 2D and 3D conditions. However, the increase of elevation needed to produce the mild levels of crosstalk in our study was only small (about 5 cm) and may have had a minimal adverse effect on performance. There was no significant difference between 2D and 3D with crosstalk conditions despite their different elevations. Finally, we acknowledge that expert laparoscopic surgeons were not tested in this study, and our results are representative of those that are still in training. We actively minimized floor effects through strict inclusion criteria which included standardized training and experience. Our study specifically targeted trainees because of the high risk of intraoperative complications during procedures performed by inexperienced laparoscopists,[10–13] and our findings highlight the large and immediate impact of 3D displays in terms of laparoscopic performance and workload. In the context of 3D colonoscopy, optimized 3D viewing conditions have been previously shown in training endoscopists to immediately improve the detection of diminutive, minimally elevated lesions by 25% [14].
In conclusion, this is the first study to characterize the negative effects from crosstalk in terms of laparoscopic performance and workload. This study has demonstrated that under optimal conditions, laparoscopic 3D displays offer considerable advantages over 2D displays. We acknowledge that we used a 3D laparoscopic system from a single manufacturer and could not ascertain if different passive-polarizing systems produce different amounts of crosstalk. Nevertheless, this study demonstrates that any level of ghosting, if encountered, should not be accepted. Preoperative ghosting checks, adjusting bed height, as well as using platforms and separate displays for team members grouped in outlying positions should be actively encouraged.
References
Sakata S, Watson MO, Grove PM, Stevenson AR (2016) The conflicting evidence of three-dimensional displays in laparoscopy: a review of systems old and new. Ann Surg 263:234–239
Sakata S, Grove PM, Hill A, Watson MO, Stevenson ARL (2016) The viewpoint-specific failure of modern 3D displays in laparoscopic surgery. Langenbecks Arch Surg 401:1007–1018
Sorensen SM, Savran MM, Konge L, Bjerrum F (2016) Three-dimensional versus two-dimensional vision in laparoscopy: a systematic review. Surg Endosc 30:11–23
Sakata S, Grove PM, Stevenson AR (2016) Effect of 3-dimensional vision on surgeons using the da vinci robot for laparoscopy: more than meets the eye. JAMA Surg 151: 793–794
Fergo C, Burcharth J, Pommergaard HC, Rosenberg J (2016) Age is highly associated with stereo blindness among surgeons: a cross-sectional study. Surg Endosc 30:4889–4894
Caldiroli D, Molteni F, Sommariva A, Frittoli S, Guanziroli E, Cortellazzi P, Orena EF (2014) Upper limb muscular activity and perceived workload during laryngoscopy: comparison of Glidescope(R) and Macintosh laryngoscopy in manikin: an observational study. Br J Anaesth 112:563–569
France DJ, Levin S, Hemphill R, Chen K, Rickard D, Makowski R, Jones I, Aronsky D (2005) Emergency physicians’ behaviors and workload in the presence of an electronic whiteboard. Int J Med Inform 74:827–837
Hubert N, Gilles M, Desbrosses K, Meyer JP, Felblinger J, Hubert J (2013) Ergonomic assessment of the surgeon’s physical workload during standard and robotic assisted laparoscopic procedures. The international journal of medical robotics + computer assisted surgery MRCAS 9: 142–147
Mohamed R, Raman M, Anderson J, McLaughlin K, Rostom A, Coderre S (2014) Validation of the National Aeronautics and Space Administration Task Load Index as a tool to evaluate the learning curve for endoscopy training. Can J Gastroenterol Hepatol 28:155–159
Smith R, Schwab K, Day A, Rockall T, Ballard K, Bailey M, Jourdan I (2014) Effect of passive polarizing three-dimensional displays on surgical performance for experienced laparoscopic surgeons. Br J Surg 101:1453–1459
Smith R, Day A, Rockall T, Ballard K, Bailey M, Jourdan I (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26:1522–1527
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, Greco F, Carvalho-Dias E, Mota P, Nogueira C, Pinho P, Mirone V, Correia-Pinto J, Rassweiler J, Lima E (2013) Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82:1444–1450
Lusch A, Bucur PL, Menhadji AD, Okhunov Z, Liss MA, Perez-Lanzac A, McDougall EM, Landman J (2014) Evaluation of the impact of three-dimensional vision on laparoscopic performance. J Endourol 28:261–266
Sakata S, Grove PM, Stevenson ARL, Hewett DG (2016) The impact of three-dimensional imaging on polyp detection during colonoscopy: a proof of concept study. Gut 65:730–731
Acknowledgements
Laparoscopic displays were lent to us by Olympus Australia for the purpose of independent research. Dr Sakata gratefully acknowledges the financial assistance from the Australian Postgraduate Award PhD and The Royal Australasian College of Surgeons Foundation for Surgery PhD Scholarships.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Shinichiro Sakata, Philip M. Grove, Marcus O. Watson and Andrew R. L. Stevenson declare no conflict of interest. There are no financial disclosures.
Rights and permissions
About this article
Cite this article
Sakata, S., Grove, P.M., Watson, M.O. et al. The impact of crosstalk on three-dimensional laparoscopic performance and workload. Surg Endosc 31, 4044–4050 (2017). https://doi.org/10.1007/s00464-017-5449-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5449-5