Abstract
Purpose
Surgeons conventionally assume the optimal viewing position during 3D laparoscopic surgery and may not be aware of the potential hazards to team members positioned across different suboptimal viewing positions. The first aim of this study was to map the viewing positions within a standard operating theatre where individuals may experience visual ghosting (i.e. double vision images) from crosstalk. The second aim was to characterize the standard viewing positions adopted by instrument nurses and surgical assistants during laparoscopic pelvic surgery and report the associated levels of visual ghosting and discomfort.
Methods
In experiment 1, 15 participants viewed a laparoscopic 3D display from 176 different viewing positions around the screen. In experiment 2, 12 participants (randomly assigned to four clinically relevant viewing positions) viewed laparoscopic suturing in a simulation laboratory. In both experiments, we measured the intensity of visual ghosting. In experiment 2, participants also completed the Simulator Sickness Questionnaire.
Results
We mapped locations within the dimensions of a standard operating theatre at which visual ghosting may result during 3D laparoscopy. Head height relative to the bottom of the image and large horizontal eccentricities away from the surface normal were important contributors to high levels of visual ghosting. Conventional viewing positions adopted by instrument nurses yielded high levels of visual ghosting and severe discomfort.
Conclusions
The conventional viewing positions adopted by surgical team members during laparoscopic pelvic operations are suboptimal for viewing 3D laparoscopic displays, and even short periods of viewing can yield high levels of discomfort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
All current generation 3D laparoscopy systems rely on passive polarization, in which surgical team members wear polarized glasses that complement horizontal rows of pixels shown on the display monitor, resulting in dedicated images for their right and left eyes [1]. Optimally, left eye images are completely blocked by the right eye lens and vice versa [2]. However, passive polarization systems are prone to crosstalk when viewed from suboptimal positions [2]. Crosstalk in a 3D display system occurs when each eye sees a mixture of the image intended for that eye and parts of the image intended for the other eye and manifests to the viewer as visual ghosting (i.e. visible double images). As well as impairing stereo vision, ghosting may result in motion sickness, headache, disorientation and fatigue [3, 4].
During laparoscopic surgery, it is common for team members to share a display viewed from different positions within an operating theatre (Fig. 1). The primary surgeon conventionally assumes the optimal viewing position, in which the viewer’s line of sight is perpendicular to and at the centre of the plane of the display [2]. In contrast, the viewing positions used by instrument nurses and surgical assistants include a range of horizontal (left/right) deviations (termed eccentricities) and vertical (up/down) deviations (termed elevations) from the optimal viewing position (Fig. 1) [5, 6]. Suboptimal viewing positions increase crosstalk by incorrect orientation of the polarized glasses relative to the display monitor [2]. Although well described in the vision science and display engineering literature, crosstalk is not widely appreciated in surgical community [1], and surgeons may not be aware of the potential hazards to their team members from suboptimal viewing during 3D laparoscopic surgery.
Compared to 2D displays, 3D displays provide direct stereoscopic depth cues which may improve both speed and technical performance in laparoscopic surgeons [1], as well as the training time of basic laparoscopic skills in novices [7]. In the context of colonoscopy, 3D viewing conditions have also been used to immediately improve the detection of diminutive, minimally elevated lesions in endoscopists [8]. However with all forms of 3D technology, individual differences among viewers can result in substantially different experiences with respect to visual comfort [9–11]. Despite the rising popularity of 3D displays amongst laparoscopic surgeons, neither surgical societies nor manufacturers have yet released recommendations on the safe use of this technology for surgical teams. To achieve this, the critical first step is to better understand how susceptibility to visual ghosting varies from individual to individual and across a range of viewing positions.
The first aim of this study was therefore to map the locations of viewpoint-specific failure of a passive polarizing laparoscopic 3D display within the dimensions of a standard operating theatre. We varied screen height (elevation), horizontal viewing angle (eccentricity) and viewing distance in order to map the locations at which individuals may experience visual ghosting from crosstalk when sharing a 3D laparoscopic display. The second aim was to demonstrate the clinical relevance of our map. We characterized the standard viewing positions adopted by instrument nurses and surgical assistants during laparoscopic pelvic ventral rectopexy and anterior resection (in terms of elevation, eccentricity and viewing distance) and reported the level of visual ghosting and discomfort associated with suboptimal viewing from these positions.
Experiment 1: viewpoint-specific failure of a laparoscopic 3D display
Methods
Participants
Participants were junior doctors from the University of Queensland (UQ) Surgical Interest Group and were the first 15 respondents to an advertisement placed on the medical school’s webpage. Participation was voluntary. All participants reported normal visual acuity and denied eye disease. Participants had normal stereoacuity (20″–50″) according to the Randot® Stereotest (Stereo Optical, Chicago, IL, USA) [12].
Viewing positions
To capture the relationships between ghosting and different aspects of viewing, each participant was tested in 176 experimental viewing positions, representing a combination of (a) four screen heights, (b) four horizontal standing eccentricities and (c) 11 distances from the monitor.
Screen height
In the four display elevation conditions, the screen was adjusted so that the participant’s eye level was either (a) equal to the top of the image (high condition), (b) equal to the middle of the image (middle condition; 16 cm below high condition), (c) equal to the bottom of the image (low condition; 16 cm below middle condition) or (d) 16 cm below the bottom of the image (ultralow condition). These elevations were chosen as they correspond to typical positions adopted by team members during laparoscopic surgery (Fig. 1).
Horizontal standing eccentricities and viewing distance
We defined horizontal standing eccentricity as the intersection angle between the surface normal of the display (represented by a tape line on the floor perpendicular to the midpoint of the horizontal plane of the display monitor) and a tape line on the floor between the viewer’s legs when facing the display. To investigate the various potential (scrubbed and unscrubbed) viewing positions within a standard 6 × 6 m operating theatre, we marked floor lines defining four horizontal standing eccentricities (0°, 30°, 45° and 60°) with distance markers added at 11 intervals (from 1 to 6 m away from the monitor in 50-cm gradations). We did not measure horizontal standing eccentricities greater than 60° as surgical team members rarely adopt this viewing position (viewers standing these areas are not able to visualize the full width of the screen). In the high, medium and low elevation conditions, viewing distance was taken as the straight distance from the back of the participant’s heels to the midpoint of a horizontal line on the floor parallel to the plane of the display monitor. In the ultralow condition, viewing distance was taken from the point on the floor directly below the participant’s back whilst sitting upright.
Laparoscopic display systems and experiment images
Target images depicted an array of objects commonly encountered during suturing in laparoscopic surgery. These included a laparoscopic needle holder, curved needles and blue 3.0 monofilament sutures against a textured, well-lit background. Live 3D images were displayed at the centre of the screen on an arm-mounted Sony LMD-2451MT LCD HDTV monitor (Sony Corporation, Tokyo, Japan). Images were captured using an Olympus Endoeye Flex 3D laparoscope, with left and right images relayed via individual Olympus CV-190 processors and integrated into 3D images by an Olympus 3DV-190 visualization unit (Olympus Co., Tokyo, Japan; Sony Corporation, Tokyo, Japan).
Grading of visual ghosting
We used magnitude estimation, a standard psychophysical procedure in which participants graded the intensity of visual ghosting on a scale of 0 to 100 [13]. Participants were instructed that 0 = no double image and 100 = a complete double image identical to viewing the 3D display without 3D glasses.
Procedure
The testing procedure was approved by the UQ Human Ethics Committee and the Program Director of the UQ School of Medicine. Participants were tested individually. Testing was conducted one horizontal standing eccentricity at a time, with a random sequence of eccentricities generated for each individual participant (e.g. 45, 0, 60, 35). For each eccentricity in the assigned sequence, the participant was tested at screen elevations in the high, middle, low and ultralow conditions, in that order. For each combination of horizontal standing eccentricity and height, the participant was asked to rate the prevalence of visual ghosting first at 1 m and then at each 50-cm interval away from the monitor up to 6 m (five times at each distance). After this, the participant rated the prevalence of visual ghosting at 6 m and then at each 50-cm interval towards the monitor back to 1 m (again, five times at each distance). Ratings were averaged over the 10 responses for each combination of horizontal standing eccentricity, screen elevation and distance. At the end of the experiment, participants also indicated the minimum magnitude of visual ghosting that they felt would not cause visual discomfort.
Statistics
The primary aim of this experiment was to assess the viewpoint-specific failure of a laparoscopic 3D display within the dimensions of a standard operating theatre (sampled at 176 different viewing positions, as described above). We achieved this by assessing the individual variation in susceptibility to visual ghosting at each viewing position and mapping the locations at which some or all individuals may experience it. Data are presented using descriptive statistics (as opposed to inferential statistics that treat variations due to individual differences as noise rather than important data).
Results
Table 1 summarizes the number and percentage of participants who reported perceived ghosting of any intensity at each viewing position. Table 1 suggests that, at all eye levels and viewing angles, fewer participants detected ghosting as they moved further away from the display. Also, ghosting tended to persist to greater viewing distances at large eccentricities (deviations in horizontal viewing angle) from the surface normal. However, even in relatively favourable viewing positions, such as the middle height condition at the surface normal, a minority of individuals still perceived visual ghosting as far as 6 m away.
When asked to specify the maximum tolerable visual ghosting magnitude, participants’ responses ranged from 10 to 30 out of 100 (M = 16.33, SD = 6.11; median = 15, mode = 15).
Table 2 summarizes the group median and range of participants’ self-rated intensity of visual ghosting as a function of viewing eye level, viewing distance and horizontal viewing eccentricity. Images viewed from the high, middle and low viewing conditions produced similarly mild median ratings of ghosting, whereas the ultralow condition yielded high levels, especially within 1.5 m of the display. The best images (i.e. those with the least ghosting) were seen at the surface normal, and greater deviations in horizontal viewing angle away from the surface tended to yield more severe ghosting. For combinations of viewing angle and height where ghosting occurred, its intensity tended to decrease with increasing distance from the monitor.
Table 3 summarizes the number and percentage of participants who reported visual ghosting of an intensity higher than the maximum that they regarded as tolerable. When participants were positioned in the low and middle viewing elevations at horizontal eccentricities of 0° (surface normal) and 30°, none reported intolerable ghosting at any viewing distance. In the high viewing elevation, two participants reported intolerable ghosting at the surface normal at 1 m and one participant reported intolerable ghosting from 1 to 3 m. Compared to the other height conditions, the ultralow condition consistently yielded ghosting in the greatest number of participants at all horizontal eccentricities, but the number of participants affected tended to increase with eccentricity and decrease with increasing viewing distance.
Figures 2 and 3 summarize the standing areas within the dimensions of a standard operating theatre that may induce visual ghosting. In each illustration, the darker shading represents the area in which all participants were affected. The lighter shading represents the area in which one or more participants were affected. These figures show that there are some positions in the operating theatre that are likely to be suboptimal for all surgical team members sharing a 3D display and others that may affect some individual team members.
Viewing locations that induced visual ghosting of any intensity in participants, mirrored and arranged by viewing height: top of image (a), middle of image (b), bottom of image (c) and 16 cm below the image (d). Dark shading indicates that all participants were affected, and light shading indicates that one or more participants were affected
Viewing locations that induced visual ghosting of an intensity that exceeded participants’ self-reported maximum tolerable thresholds, mirrored and arranged by viewing height: top of image (a), middle of image (b), bottom of image (c) and 16 cm below the image (d). Dark shading indicates that all participants were affected, and light shading indicates that one or more participants were affected
Experiment 2: the potential hazards of 3D laparoscopic displays
Having examined and mapped the physical locations where visual ghosting may occur for some or all surgical team members when sharing a 3D display in experiment 1, the aim of experiment 2 was to demonstrate the practical implications of these results. We characterized our standard viewing positions adopted by our instrument nurses and surgical assistants during 3D laparoscopic ventral rectopexy and anterior resection (in terms of elevation, eccentricity and viewing distance). We assessed the level of perceived visual ghosting (as in experiment 1) and discomfort (as measured by the Simulator Sickness Questionnaire [14]) associated with suboptimal viewing from these working positions during a simulated procedure in a simulation laboratory.
Methods
Participants
Six nurses and six surgical assistants voluntarily participated in the study. The nurses (four female, two male), who comprised the entire colorectal surgery nursing team of a major tertiary hospital, had a mean age of 38.6 years (range 27–55) and a mean of 14 years of surgical nursing experience (range 7–30). Their mean height was 163 cm (range 154–172). The surgical assistants were junior doctors who had completed their surgical rotations and were regularly involved in laparoscopic assisting. The assistants (three female, three male) had a mean age of 24.3 years (range 21–29) and a mean height of 176 cm (range 166–180 cm). All participants reported normal visual acuity and denied eye disease. All participants had normal stereoacuity (20″–50″) as measured by the Randot® Stereotest (Stereo Optical, Chicago, IL, USA) [12].
Simulated operation and viewing positions
The experiment was conducted in a simulation operating theatre and was designed to simulate intracorporal suturing during laparoscopic ventral rectopexy. Having examined in experiment 1 the physical locations where visual ghosting may occur in surgical team members, we found that intolerable ghosting would not be perceived by conventional position of the primary surgeon, in which the surgeon’s line of sight is perpendicular to and at the centre of the plane of the display. We therefore used experiment 2 to demonstrate the practical implications of experiment 1. Based on the clinical expertise of our participants, we chose to simulate 3D laparoscopic ventral rectopexy (LVR) and characterize the standard viewing positions adopted by instrument nurses and surgical assistants during LVR. Figure 4a shows the 3D display system and the operative set-up. Various horizontal eccentric viewing angles are represented by yellow measuring tapes. We used four viewing positions which we regularly used in LVR (Fig. 4b). These positions were the camera assistant (surgical assistant position 1), second assistant or passive viewer (surgical assistant position 2), the primary position of the instrument nurse (scrub nurse position 1; which, for this operation, is standing between the patient’s legs for the majority of the operating time) and the secondary position of the instrument nurse (scrub nurse position 2; which, for this operation, is standing beside the instrument table).
a Surgical simulation of a laparoscopic ventral rectopexy operation. Various horizontal eccentric viewing angles are represented by yellow measuring tapes. b The different horizontal eccentric viewing angles and viewing distances adopted by participants in the simulated laparoscopic ventral rectopexy operation (experiment 2). Positions: camera assistant (surgical assistant 1), second assistant or passive viewer (surgical assistant 2), the primary position of the instrument nurse (scrub nurse position 1) and the secondary position of the instrument nurse (scrub nurse position 2). The position of the primary surgeon is also detailed here
We used our clinical experience with LVR and pilot testing to determine the specific eccentricities and viewing distances used in experiment 2. We are confident of the face and construct validity of the outlying positions as surgeon investigators and all nurses who participated in the study (who were experienced in colorectal surgery) unanimously agreed with the appropriateness of the simulation set-up. In terms of viewing distance, we used a pilot group of three individuals who stood side by side whilst viewing a 3D display monitor. From a practical perspective, we found that it was not possible for the test group to adequately view the 52 cm (width) × 32 cm (height) picture size at the manufacturer’s typical viewing distance of 64 cm (see Operation Manual: LMD-2451MT; http://pro.sony.com.au/pro/support/operation-manual/1237492997971) without overlapping their standing positions and therefore risking surgical contamination during an actual operation. We found that the test group could collectively view the 3D display from a standing distance of 1.5 m. This viewing distance also allowed us to comfortably fit in our operating and instrument tables into the simulation shown in Fig. 4a. The experimental horizontal eccentric viewing angles, viewing distances and elevations are described further in the following paragraph and in the Results section.
Participants were asked to stand in their predefined, randomly assigned viewing positions (toes on an X marked on the floor) with their feet either side of a yellow line marker that indicated the horizontal eccentricity of the position from surface normal. Viewing distances were measured from the X to a point on the floor directly below the centre of the screen. As in real operations, screen height during the experiment was set so that the surgeon’s eye level was to the centre of screen. The primary surgeon (SS) is 178 cm tall and stood at a viewing distance of 1.5 m (Fig. 4b). From a practical perspective, it may be difficult for members of a surgical team to stand by side at a manufacturer’s typical standing distance of 64 cm without risking surgical contamination during an operation. We suggest that the ideal group viewing distance is 2 m from the display monitor allowing for individual differences in the majority of height and horizontal viewing angles. The head level of each participant, relative to the bottom of the image (either above or below), was used to classify viewing elevation. Participants who stood beneath the bottom of the monitor display panel were classified as being in the ultralow viewing elevation.
Laparoscopic display systems and target images
The display system was identical to that used in experiment 1. Images shown on the 3D display were live motion images captured from a box trainer built into the pelvis of a simulation manikin (Fundamentals of Laparoscopic Surgery) [15]. Laparoscopic needle holders, curved needles and looped threads were displayed against a textured, well-lit background. Using the above instruments, normally used in laparoscopic ventral rectopexy, the role of the surgeon was to continuously create moving 3D images by suturing for the duration of the experiment.
Grading of visual ghosting
The same method was used as in experiment 1.
The Simulator Sickness Questionnaire
The Simulator Sickness Questionnaire (SSQ) is a standard questionnaire used in vision science research to assess the effect of 3D images on visually induced discomfort. Total SSQ scores higher than 10 indicate significant symptoms, and scores greater than 20 indicate severe discomfort from a ‘problem simulator’ [14, 16, 17].
Procedure
The testing procedure was approved by the UQ Human Ethics Committee. Each nurse was randomly assigned to one of the two instrument nurse positions, and each assistant was randomly assigned to either the camera assistant or surgical observer position. The simulation was repeated three times to test all 12 participants. The viewing time for all participants was 15 min. To ensure that the participants were focusing on the 3D display during the entire exercise, they were instructed to silently count the number of times that the surgeon made needle drops. Following the simulation, participants were asked to individually complete the SSQ.
Statistics
We conducted this experiment to describe the symptoms experienced by individual participants located in clinically relevant viewing positions. This experiment is a practical example of the potential hazards associated with the viewpoint-specific failure 3D laparoscopic displays. We therefore analysed data using descriptive statistics to capture individual variation.
Results
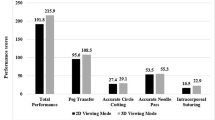
Figure 4b summarizes the different horizontal eccentric viewing angles, viewing distances and elevations adopted by surgical nurses and assistants. The results below are presented separately for each viewing position.
Instrument nurses (primary position)
Instrument nurses standing in the primary position (between the patient’s legs) viewed the screen at an eccentricity of 60° (right of surface normal) and a distance of 1 m. All nurses in this position viewed the 3D display in the ultralow elevation. Their mean visual ghosting rating was 93.3/100 (range 80–100), and mean SSQ score was 43.8 (range 11.7–59.8).
Instrument nurses (secondary position beside the instrument table)
Instrument nurses standing in the secondary position (beside the instrument table) viewed the screen at an eccentricity of 45° (right of surface normal) and a distance of 1.5 m. All nurses in this position viewed the 3D display in the ultralow elevation. Their mean visual ghosting rating was 46.7/100 (range 45–50), and mean SSQ score was 82.3 (range 67.3–93.5).
Camera assistant
Medical students standing in the camera assistant position viewed the screen at an eccentricity of 30° (left of surface normal) and a distance of 1.5 m. These participants viewed the screen with their eye level in either the middle or bottom half of the image. Their mean visual ghosting rating was 6.7/100 (range 5–10), and all had SSQ scores of 3.7.
Second assistant
Medical students in the surgical observer position viewed the screen at an eccentricity of 45° (left of surface normal) and 1.5 m respectively. These participants viewed the screen with their eye level in either the middle or bottom half of the image. Their mean visual ghosting rating was 11.5/100 (range 10–12), and mean SSQ score was 13.6 (range 11.2–14.9).
Effect of platform to elevate viewing position
The horizontal eccentricities and viewing distances of the instrument nurses in the secondary position (beside the instrument table) were equivalent to those of the medical students in the second assistant position. To explore the possibility that the apparent difference in visual ghosting ratings between these two groups could be attributed to differences in height relative to the screen (the only spatial variable that differed between the groups), we subsequently invited the three nurses in the secondary position to return to the theatre and view the 3D images whilst standing on a platform that raised their eye level to approximately the middle of the image. Viewing from this new position, their mean visual ghosting rating improved from 46.7/100 (range 45–50) to 13.5/100 (range 10–15).
Discussion
In the present study, we identified and mapped the positions within a standard operating theatre where individuals may experience visual ghosting when using a passive polarizing 3D display (experiment 1) and went on to demonstrate the practical implications of these findings using simulated laparoscopic ventral rectopexy surgery (experiment 2).
When viewers were positioned in suboptimal viewing positions, we observed that they reported higher intensity ghosting at shorter viewing distances. In experiment 1, we found that viewing the 3D display with an eye level below the bottom of the image (the ultralow viewing position) yielded the most severe ghosting. Looking up at the screen from this elevation at a viewing distance of 1 m, all participants reported visual ghosting of magnitude 100, which is equivalent to viewing the 3D image without wearing polarizing glasses (i.e. no stereopsis). Substantial visual ghosting was also reported by some participants at greater distances. The subjective ratings of visual ghosting at this elevation were greatest at horizontal eccentricities of 45° and 60°.
Elevations similar to the ultralow viewing condition are commonly adopted by surgical nurses when they are seated, crouched in ergonomically difficult positions during retraction or standing but sharing the 3D display with taller primary surgeons. Primary surgeons also routinely adopt ultralow viewing elevations whilst seated during laparoscopic-assisted transanal operations such as total mesorectal excision (taTME) and transanal minimally invasive surgery (TAMIS). Surgeons may elect to tilt the screen downwards (directly facing the seated surgeon) to minimize the crosstalk that they experience. However, this orientation will only exaggerate the crosstalk experienced by other standing team members due to the incorrect orientation of their polarizing glasses to the display. Conventional 2D working positions may need to be modified for 3D laparoscopy to avoid potential harm to members of the surgical team, and we emphasize that optimal surgeon comfort should not come at the expense of suboptimal viewing positions for other team members. In all of the above operations, visual discomfort can be avoided by raising the operating table such that the surgeon stands whilst working and viewing the display. We found that, when their eyes aligned with the middle of the screen, participants gave relatively low ratings of crosstalk at all horizontal viewing eccentricities and at all viewing distances. We recommend that primary surgeons have their eyes aligned to the middle of the picture image for maximum viewing comfort. For team members in the ultralow viewing positions, it may be possible to reduce or remedy visual ghosting through physical accommodations, such as giving shorter team members platforms to stand on (as illustrated in the coda to experiment 2) or using multiple 3D monitors (where there is currently no standard for the number of displays that should be used).
At greater viewing distances, visual ghosting decreased to subjectively tolerable levels for all horizontal eccentricities and screen heights. However, one participant reported uncomfortable levels of visual ghosting at viewing distances as far as 500 cm and at a horizontal eccentricity of 60° in the high viewing condition, demonstrating the potential impact of individual differences. The individual differences demonstrated in experiment 1 indicate that there is no ‘perfect group viewing distance’ that can accommodate all surgical team members in all outlying positions. Importantly, our results demonstrate that there are viewing positions which induced intolerable levels of ghosting in all viewers. These viewing positions should be avoided completely in the design of 3D laparoscopic operations. Alternatively, an additional display producing 2D images could be used for staff who need to be in a particular location or whose extreme susceptibility to visual ghosting means that they cannot otherwise be accommodated.
Experiment 2 highlights that the conventional viewing positions adopted by instrument nurses during laparoscopic pelvic operations are suboptimal for viewing 3D laparoscopic displays. Subjective ratings of visual ghosting in experiment 2 were consistent with the results of experiment 1, that is, all participant ratings were within the equivalent ranges from experiment 1. Participants in the two instrument nurse positions experienced intense visual ghosting that far exceeded the threshold for intolerability established in experiment 1 (>15) and also experienced motion sickness falling within the ‘severe discomfort’ range of the SSQ (>20), despite only a relatively short period of viewing in suboptimal conditions. In contrast, camera assistants experienced low levels of visual ghosting and motion sickness, and second assistants experienced slightly higher (but still tolerable) levels of visual ghosting coupled with ‘significant’ (but not severe) motion sickness. Interestingly, instrument nurses positioned beside the instrument table reported almost double the level of motion sickness of instrument nurses positioned between the patient’s legs (82.6 versus 43.8), despite reporting less visual ghosting (46.7 versus 93.3). The perception of 3D imagery decreases with increasing levels of crosstalk such that, at viewing positions affected by extreme levels of crosstalk, ‘3D’ laparoscopic images appear ‘flatter’ (i.e. there is minimal stereopsis, and they appear similar to viewing the 3D display without 3D glasses). Our data suggest that, beyond a certain threshold of visual ghosting (as evidenced by the lower levels of visual ghosting and motion sickness reported by surgical assistants), moderate levels of visual ghosting in 3D may be considerably more uncomfortable than extreme levels of visual ghosting in 2D.
A limitation of this study was that we used a 3D laparoscopic system from a single manufacturer. However, with respect to crosstalk, we do not expect large variation between manufacturers as the current generation of 3D laparoscopic systems all relies on passive polarization technology [1]. Even with the single system that was used, this study highlights that, although suboptimal viewing positions may expose surgical team members to crosstalk, individual tolerances may be markedly different. Hence, in practice, individual team members’ susceptibility to crosstalk at relevant locations may need to be assessed, regardless of the brand of 3D display used. A further limitation of this study is that our four viewing positions used in experiment 2 may not be universal across all centres for LVR. This may be so, but the aim of experiment 2 was to demonstrate an example of the practical implications of the maps of visual ghosting that we reported in experiment 1. For all 3D laparoscopic operations, we recommend the use of our maps, as well as preoperative team positioning to assess individual ratings of visual ghosting, to guide the implementation of physical accommodations for optimum surgical team performance and comfort.
In conclusion, crosstalk is described in the vision science and display engineering literature [3, 4], but this information has not yet been disseminated in the surgical literature or incorporated into surgical guidelines and consensus statements. From a practical perspective, it may also be difficult for members of a surgical team to stand by side at a manufacturer’s typical standing distance of 64 cm without risking surgical contamination during an operation. This is the first study to address crosstalk within a surgical team. Laparoscopic surgeons conventionally assume the optimal viewing position and may not be aware of the potential hazards to team members positioned across different suboptimal viewing positions. Our experiments highlight that surgical nurses and surgical assistants sharing laparoscopic 3D displays may be commonly exposed to visual ghosting because of their viewing positions. Specifically, we have examined the viewpoint-specific failure of a laparoscopic 3D display and identified locations where visual ghosting may result within the dimensions of a standard operating theatre. It is plausible that nursing responsibilities related to patient safety, such as correctly preparing instruments and finalizing instrument counts, could be compromised by the discomfort caused by suboptimal 3D viewing during laparoscopic pelvic surgery. The use of platforms and separate displays for team members grouped in outlying positions should be actively encouraged to avoid unnecessary trade-offs between surgeon and nursing comfort. Although we only evaluated the suboptimal viewing positions of one common operation in experiment 2, our map in experiment 1 may assist the preoperative planning of other laparoscopic operations. Using the bottom of the image as a guide is a fast and simple heuristic to identify and avoid the worst suboptimal viewing positions.
References
Sakata S et al. (2016) The conflicting evidence of three-dimensional displays in laparoscopy: a review of systems old and new. Ann Surg 263(2):234–239
Woods, A.J. 2012 Crosstalk in stereoscopic displays: a review. J Electron Imaging 21(4)
Yang SN et al. (2012) Stereoscopic viewing and reported perceived immersion and symptoms. Optom Vis Sci 89(7):1068–1080
Howarth PA (2011) Potential hazards of viewing 3-D stereoscopic television, cinema and computer games: a review. Ophthalmic Physiol Opt 31(2):111–122
Grove PM (2012) In: Zhu C, Zhao Y, Yu L, Tanimoto M (eds) The psychophysics of binocular vision, in 3D-TV system with depth-image-based rendering. Springer, New York, pp. 347–373
Lee CT, Lin HY, Tsai CH (2010) Designs of broadband and wide-view patterned polarizers for stereoscopic 3D displays. Opt Express 18(26):27079–27094
Poudel, S., et al. 2016 Impact of 3D in the training of basic laparoscopic skills and its transferability to 2D environment: a prospective randomized controlled trial. Surg Endosc
Sakata S et al. (2016) The impact of three-dimensional imaging on polyp detection during colonoscopy: a proof of concept study. Gut 65(5):730–731
Jin, E.W., et al. 2005 Creating a comfortable stereoscopic viewing experience: effects of viewing distance and field of view on fusional range
Kooi FL, Toet A (2004) Visual comfort of binocular and 3D displays. Displays 25(2–3):99–108
Sakata, S., P.M. Grove, and A.L. Stevenson 2016 Effect of 3-dimensional vision on surgeons using the da vinci robot for laparoscopy: more than meets the eye. JAMA Surgery
Zaroff CM, Knutelska M, Frumkes TE (2003) Variation in stereoacuity: normative description, fixation disparity, and the roles of aging and gender. Invest Ophthalmol Vis Sci 44(2):891–900
Stevens, S.S. 1975 Psychophysics. Transaction Publishers
Kennedy RS et al. (1992) Use of a motion sickness history questionnaire for prediction of simulator sickness. Aviat Space Environ Med 63(7):588–593
Peters JH et al. (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135(1):21–27
Kennedy RS, Berbaum KS, Lilienthal MG (1997) Disorientation and postural ataxia following flight simulation. Aviat Space Environ Med 68(1):13–17
Solimini AG (2013) Are there side effects to watching 3D movies? A prospective crossover observational study on visually induced motion sickness. PLoS One 8(2):e56160
Acknowledgments
Laparoscopic displays were provided to us by Olympus Japan for the purpose of independent research. Dr. Sakata received financial assistance from the Avant Doctors in Training PhD Scholarship. The funding source had no role in study design, data collection, analysis or interpretation, report writing or the decision to submit this paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest, financial or otherwise.
Ethics approval
The study was approved by the University of Queensland (UQ) Human Research Ethics Committee.
Contributions
Dr. Sakata led the conceptualization, planning, execution of this research, analysis and writing the manuscript; Drs. Grove, Hill, Watson and Stevenson contributed to the planning, analysis and manuscript writing.
Rights and permissions
About this article
Cite this article
Sakata, S., Grove, P.M., Hill, A. et al. The viewpoint-specific failure of modern 3D displays in laparoscopic surgery. Langenbecks Arch Surg 401, 1007–1018 (2016). https://doi.org/10.1007/s00423-016-1495-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1495-z