Abstract
Background
The prevalence of stereo blindness in the general population varies greatly within a range of 1–30 %. Stereo vision adds an extra dimension to aid depth perception and gives a binocular advantage in task completion. Lack of depth perception may lower surgical performance, potentially affecting surgical outcome. 3D laparoscopy offers stereoscopic vision of the operative field to improve depth perception and is being introduced to several surgical specialties; however, a normal stereo vision is a prerequisite. The aim of this study was to establish the prevalence of stereo blindness among surgeons in the field of general surgery, gynecology, and urology as these are potential users of 3D laparoscopy.
Methods
The study was conducted according to the STROBE guidelines for cross-sectional studies. Medical doctors from the department of general surgery, gynecology, and urology were recruited and stereo tested by the use of the Random Dot E stereo test. Upon stereo testing, a demographic questionnaire was completed. Multivariate logistic regression analysis was employed to assess the association between stereo blindness and the variables resulting from the univariate analysis.
Results
Three hundred medical doctors completed the study. Of these 9.7 % were stereo blind. There were 47 % women and 53 % men, aged 25–71 years. General surgery was represented with 64 % of the participants, gynecology with 26 %, and urology with 10 %. Age (OR 5.6; CI 1.7–18.9; P = 0.005) and not being aware of having any vision anomaly in need for correction (OR 4; CI 1.4–11.4; P = 0.010) were significantly associated with stereo blindness.
Conclusion
Approximately one in ten medical doctors in general surgery, gynecology, and urology were stereo blind with an increasing prevalence with age. This is relevant since stereo blind surgeons will not benefit from the implementation of 3D laparoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic technique is standard in many surgical procedures today although it may be compromised by lack of depth perception and the mechanical constraint when operating with elongated instruments through small incision points [1]. In particular converting a two-dimensional image on a monitor to a three-dimensional (3D) perception may involve a long learning curve for novice surgeons [2]. Introducing 3D laparoscopy in both experimental and clinical settings has been a way to address this aspect as it mimics the human stereopsis with the use of two adjacent laparoscopic cameras, resulting in shorter duration of surgery [3, 4] and a reduction of errors [1, 2].
Stereopsis is the 3D percept achieved from the fusion of the separate images from each eye, which only differ in the relative horizontal disparity [5]. This effect is integrated in robotic-assisted surgery where the images from each camera is presented separately to each eye and thus exploiting the natural stereopsis [6]. This means that individuals not aware of their stereo blindness can operate on the robot without discovering this disadvantage. In 3D laparoscopy, the images from two cameras are fused and presented as a single 3D image by a special monitor and viewed through polarized glasses [1]. The definition and prevalence of stereo blindness vary according to the methods used to assess or confirm binocular vision, thus rendering different results as to what constitutes the presence of stereo blindness, particularly in the general population [7, 8]. The prevalence in the general population of complete stereo blindness is reported to be 1–30 % [9–12]. Stereopsis is a prerequisite for 3D laparoscopy [1, 13], indicating that stereo blind surgeons will not benefit or potentially experience discomfort from this modality. Hence, the prevalence of stereo blindness among surgeons is important in order to evaluate the potential value of 3D laparoscopy.
This study aimed to assess the prevalence of stereo blindness in medical doctors in the fields of general surgery, gynecology and urology, as these are potential users of 3D laparoscopy.
Materials and methods
This cross-sectional study was conducted between March 2015 and June 2015 in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement [14].
The study population comprised medical doctors from the departments of general surgery, gynecology and urology from eight hospitals in Denmark. Following stereo testing, all participants completed a short questionnaire with baseline characteristics (demographic information, assessment of visual attributes, discomfort during transportation or while viewing a 3D movie). The participants were allowed to use their corrective lenses, if any, and were neither screened nor excluded on the basis of any known visual anomaly as we wished to assess the prevalence of stereo blindness, as a lack of stereo vision, in the general study population and not in a study population devoid of any such visual abnormality.
The stereo test used was the validated Random Dot E (RDE) stereo test [15–17] (Stereo Optical Co., Inc., Chicago, IL), which consists of two hand-held 8 × 11 cm test plates, seemingly similar, but when viewing through polarized filters (glasses) one test plate is “blank” containing an array of random dots, while the other test plate reveals a stereoscopic “E”.
The stereo testing was conducted fronto-parallel to the subject’s line of sight and under bright lighting conditions with respect to averting any glare or reflections. All participants wore polarized glasses. These were placed over their visual corrective lenses, if they used any. They were given careful instructions to be honest and not guess in which plate, they could locate a letter [7]. The participants did not know the letter in question beforehand and was instructed to specifically identifying the location and which letter they saw [18]. The test plates were shuffled out of sight of the subject before each presentation to minimize the risk of merely guessing the correct test plate [18]. This was done four consecutive times when identifying the correct letter, five times in total, which minimizes the probability of passing by chance alone to 3 % (0.55). The subjects were allowed unlimited time to identify the letter [9].
To avoid any depth perception signs that can be perceived through the use of one eye (monocular cues) such as motion parallax (when closer objects appear to move faster than objects further away), enabling the participants to pass the test without stereo vision, they were instructed to hold their head completely still [10]. The relative disparity and thus the stereo acuity of the stereo E target vary as a function of the viewing distance at which the target E is presented [19]. The test plates were presented at the following viewing distances: 50, 100, 150 cm [20], and the correct distances were ensured by tape strips on a mat. However, the large disparities of the RDE stereo test make it unsuitable for accurate threshold determination [19] and in this study, it is used as a pass/fail stereo test. Thus, the test is used to determine the presence or absence of stereo vision and not the degree of stereo vision, which is known as stereo acuity. Participants failing to correctly identify the stereoscopic E at 50 cm (504 arcsec) viewing distance five times in a row, despite demonstrating understanding of the test, were designated stereo blind. Failing only at viewing distances of 100 cm (252 arcsec) and 150 cm (168 arcsec), but passing at 50 cm, classified the participants as stereo deficient, but not stereo blind [15, 21, 22].
All volunteers received a complete explanation of the purpose and procedure of stereo testing and gave their informed consent. The study was approved by The Regional Committee on Health Research Ethics (H-15004147).
Statistical analyses were conducted with the Statistical Package for Social Sciences (SPSS) version 22 (IBM, Armonk, NY). The prevalence and the univariate associations between a categorical outcome and the variables under consideration were evaluated using Pearson’s Chi-square test. Variables that were significantly associated with stereo blindness in the univariate analysis with P < 0.2 were included in the multivariate logistic regression analysis. Using the Enter method the odds ratios (OR) with 95 % confidence intervals (CI) were calculated to determine whether these variables were significantly associated with the presence of stereo blindness. The accepted level of significance was set at P < 0.05. The sample size estimation required 300 participants, calculated from a conservative assumption of a prevalence of stereo blindness of 2 % [9, 10, 22] with a defined power of 80 % and a significance level of 5 % that would yield a reasonable confidence interval 95 % CI (0.7–4.3).
Results
A total of 305 medical doctors were approached and 300 were included. Five doctors refused to participate. Of the 300 included doctors, 9.7 % (n = 29) were stereo blind and 38.7 % (116) were stereo deficient. None of the stereo blind subjects were able to detect the stereoscopic E at a closer distance than 50 cm. The demographic distribution is shown in Table 1. Five persons refused to participate (three male consultant surgeons from general surgery and two female chief surgeons from urology), which gave a response rate of 98 %. There were 141 (47 %) females and 159 (53 %) male participants aged 25–71 years with varying seniority categorized as post graduation years (PGY). Almost half of the study population was past 10 PGY. General surgery, gynecology, and urology were represented by 192 (64 %), 79 (26 %), and 29 (10 %) participants, respectively. The majority (91 %) was non-smokers and 80 % reported not having experienced discomfort while watching a 3D movie. Vision correction was found in 182 (61 %) participants, while 31 (11 %) reported having a visual abnormality that was not yet corrected.
The prevalence of stereo blindness was significantly associated with age over 50 years, gender, PGY, surgical specialty, smoking, motion sickness, and with no awareness of having any visual anomaly which was not yet corrected (Table 1). Of these variables, only age (OR 5.6; CI 1.7–18.9; P = 0.005) and not being aware of having any vision anomaly in need for correction (OR 4; CI 1.4–11.4, P = 0.010) were significantly associated with the presence of stereo blindness in the adjusted analysis.
Discussion
A total of 300 medical doctors were included in this cross-sectional study investigating the prevalence of stereo blindness among medical doctors in the field of general surgery, gynecology, and urology. Overall, the prevalence of stereo blindness was 9.7 % with almost 6 times higher odds for being stereo blind for doctors over 50 years of age and 4 times higher odds when not being aware of having any vision anomaly that would need correction.
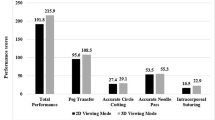
Studies evaluating the functional effect of stereopsis on task completion revealed that participants with normal stereo vision performed better with regard to hand-eye coordination and motor skills [11, 23, 24]. Correspondingly, the stereo blind managed significantly worse than both the stereo normal or stereo deficient subjects [11, 23]. Surgeons, in particular, would highly benefit from the use of stereopsis as this gives a notably binocular advantage in tasks that require fine adjustments in motor control. In laparoscopy, these tasks are numerous and include needle threading and grasping [5, 24, 25] and using tools for dissection etc. [26, 27]. It can therefore be hypothesized that surgeons can gain from the introduction of 3D laparoscopy. A previous study evaluated stereo acuity among 66 surgeons across twelve different surgical specialties and found that 20 per cent of practicing surgeons had reduced or no stereopsis [28]. The conclusion was that high-grade stereo acuity was not a prerequisite for a career in surgery, since these surgeons were actively practicing surgery. However, this study was not related to 3D laparoscopy but only to conventional laparoscopy where stereopsis is not necessarily an essential factor. Furthermore, the study did not compare stereo acuity to surgical performance. Our study found a prevalence of 9.7 % being completely stereo blind, suggesting that these surgeons would be unduly disadvantaged with the introduction of 3D laparoscopy.
An interesting aspect is the trainee selection and subsequent sub-specialization among stereo blind residents. A possible future scenario could be to screen surgical applicants as done in other high risk industries such as aviation [29]. However, surgical competence involves much more than stereo vision such as experience, ability to make a clinical judgement, anatomical knowledge, etc. Stereo blind individuals have learned techniques through monocular clues to overcome their lack of stereo vision in 2D-laparoscopy [1, 28]. Consequently, an eventual screening should be based on the overall capabilities of the surgeon. As stereo blind surgeons perform well in 2D, the possibility of being certified in minimally invasive surgery through 2D-simulators must be sustained, especially when one in ten surgeons is stereo blind. In order to evaluate the importance of stereo vision, future studies are required to assess the impact of stereo blindness on surgical performance with clinically relevant outcomes. Considering the very large sample size needed in order to observe any effect on patient safety, this may not be realistic to accomplish and surrogate endpoints may be acceptable as an alternative.
There are several causes for stereo deficiency. The main reasons are ocular conditions that disrupt the binocular function (accommodation or convergence insufficiencies) such as strabismus (“cross-eyed”), amblyopia (“lazy eye”) [9], or age-related deterioration [10, 30, 31]. Moreover, a significant correlation has been found between how accurate your stereo vision is with how accurate your binocular vision is in general [9]. Complete or partly stereo recovery with vision therapy to aid eye alignment and perceptual learning is only possible for some individuals with abnormal binocular vision due to ocular conditions [32]. Whether this also applies to stereo blind individuals without ocular conditions, is yet to be resolved.
The association between age and stereo blindness corresponds well to the overrepresentation of stereo blindness among the surgeons over 50 years in the present study. It is known that a decline in visual processing and visuospatial ability exists with increasing age [33]. However, stereo blindness is only one parameter in the age-related cognitive decline and cannot stand alone in an evaluation of surgical competence.
Interestingly, no reason is established in a third of people with poor stereo vision [10], which may explain the increased risk of stereo blindness found in this study among those reporting not being aware of having any vision anomaly in need for correction. This may indicate that people assess their vision as better than it perhaps is in reality and that the reason for stereo blindness for some possibly is a need for vision correction. A good vision in general is an important feature for a surgeon to possess, and it would be wise to have regular checks, especially when over 50 years of age, as vision correction may move some of the surgeons from the stereo blind group to the group with sufficient stereo vision.
This study holds some limitations. The object to be detected in the RDE stereo test is defined by its disparity alone, i.e., there are no edges to drive object recognition and a good vision in both eyes is required for achieving a stereoptic response on this type of stereo test [7]. Thus, some concerns have been raised that these tests are too demanding, with the risk of overestimating the results; nonetheless an optimal stereo test does not yet exist [34]. The choice and result of a stereo test depend substantially on the question in mind, hence the variation of reported prevalence and definition of stereo blindness [5]. Furthermore, the aim of this study was to find the proportion of stereo blindness and not the stereo acuity of the medical doctors, and for this purpose the RDE is a quick and easy stereo test to apply [10, 15, 35, 36]. It is regarded as an objective test for stereopsis in which monocular cues are absent [34, 37] with a good reliability [15] and a high testability [20] and is thus recommended as the best diagnostic tool for measuring stereopsis, also in the adult population [8].
This cross-sectional study was conducted in accordance with the STROBE statement [14]. Furthermore, the study investigated an extensive number of subjects. The subjects worked in several hospitals in Denmark, thus increasing external validity. Another positive aspect is the use of a stereo test devoid of monocular clues which limits the risk of underestimating the prevalence of stereo blindness within this study population.
Overall, approximately one in ten medical doctors in the surgical departments evaluated was stereo blind. Without the enhancing effect of stereopsis, there is a risk of misjudging distances and thereby worsening surgical performance, potentially leading to serious clinical complications. 3D laparoscopy can ameliorate this scenario for surgeons with normal stereo vision; however, the stereo blind surgeons will not gain from the implementation of 3D laparoscopy or potentially feel discomfort. Considering the high prevalence of stereo blindness, especially within the older consultant surgeons in this study population, who typically perform most of the complicated laparoscopic procedures, the rationale in implementing 3D laparoscopy can be discussed. The same considerations are equally evident in robotic surgery. Stereo blind surgeons will be stereo blind in the robot as well with the risk of performing similarly imprecise as stereo blind surgeons working with 2D-laparoscopy. In our study, we found that some stereo blind surgeons overestimated their vision and did not realize that they lacked stereo vision. These stereo blind surgeons will be able to operate the robot without discovering that their inability to judge distances is compromised.
If the future technique becomes 3D laparoscopy, the possibility of viewing the operative field in 2D should be maintained as this may be essential for the surgical performance of the stereo blind surgeons since they do not perform similarly worse in 2D-viewing [27, 38]. Likewise, having the vision regularly examined and using proper vision correction can for some surgeons possibly improve their stereo vision. Furthermore, it would be reasonable to apply a test for stereopsis when conducting comparative studies evaluating the effect of 3D displays in minimally invasive surgery.
In conclusion, the prevalence of stereo blindness among medical doctors in the field of general surgery, gynecology, and urology was 9.7 % and increasing with age. These surgeons will not have any effect of 3D laparoscopy with a potential risk of performing worse during surgery than their stereo normal counterparts. However, the majority of surgeons can likely benefit from the introduction of 3D laparoscopy.
References
Taffinder N, Smith SGT, Huber J, Russell RCG, Darzi A (1999) The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13(11):1087–1092
Smith R, Day A, Rockall T, Ballard K, Bailey M, Jourdan I (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26(6):1522–1527
Sahu D, Mathew MJ, Reddy PK (2014) 3D Laparoscopy-help or hype; initial experience of a tertiary health centre. J Clin Diagn Res 8(7):NC01–NC03
Bilgen K, Üstün M, Karakahya M, Isik S, Sengül S, Çetinkünar S, Küçükpinar TH (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23(2):180–183
Richards Whitman (1970) Stereopsis and stereoblindness. Exp Brain Res 10(4):380–388
Blavier A, Nyssen AS (2014) The effect of 2D and 3D visual modes on surgical task performance: role of expertise and adaptation processes. Cogn Technol Work 16(4):509–518
Read JC (2015) Stereo vision and strabismus. Eye 229(2):214–224
Heron S, Lages M (2012) Screening and sampling in studies of binocular vision. Vis Res 62:228–234
Bosten JM, Goodbourn PT, Lawrance-Owen AJ, Bargary G, Hogg RE, Mollon JD (2015) A population study of binocular function. Vis Res 110:34–50
Bohr I, Read JCA (2013) Stereoacuity with frisby and revised FD2 stereo tests. PLoS One 8(12):e82999
Schiller PH, Kendall GL, Kwak MC, Slocum WM (2012) Depth perception, binocular integration and hand-eye coordination in intact and stereo impaired human subjects. J Clin Exp Ophthalmol 3:210
Coutant BE, Westheimer G (1993) Population distribution of stereoscopic ability. Ophthalmic Physiol Opt 13(1):3–7
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26(5):1454–1460
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative Strobe (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med 45(4):247–251
Schmidt PP (1994) Vision screening with the RDE stereotest in pediatric populations. Optom Vis Sci 71(4):273–281
Hammond RS, Schmidt PP (1986) A random dot E stereogram for the vision screening of children. Arch Ophthalmol 104(1):54–60
Shallo-Hoffmann J, Coulter R, Oliver P, Hardigan P, Blavo C (2004) A study of pre-school vision screening tests’ testability, validity and duration: do group differences matter? Strabismus 12(2):65–73
Fricke T, Siderov J (1997) Non-stereoscopic cues in the random-dot E stereotest: results for adult observers. Ophthalmic Physiol Opt 17(2):122–127
Heron G, Dholakia S, Collins DE, McLaughlan H (1985) Stereoscopic threshold in children and adults. Am J Optom Physiol Opt 62(8):505–515
Vision in Preschoolers Study Group, Schmidt P, Maguire M, Kulp MT, Dobson V, Quinn G (2006) Random dot E stereotest: testability and reliability in 3-to 5-year-old children. JAAPOS 10(6):507–514
Ruttum MS, Nelson DB (1990) Stereopsis testing to reduce overreferral in preschool vision screening. J Pediatr Ophthalmol Strabismus 28(3):131–133
Fielder AR, Moseley MJ (1996) Does stereopsis matter in humans? Eye 10(2):233–238
O’Connor AR, Birch EE, Anderson S, Draper H (2009) The functional significance of stereopsis. Invest Ophthalmol Vis Sci 51(4):2019–2023
Levi DM, Knill DC, Bavelier D (2015) Stereopsis and amblyopia: a mini-review. Vis Res 114:17–30
Melmoth DR, Finlay AL, Morgan MJ, Grant S (2009) Grasping deficits and adaptations in adults with stereo vision losses. Invest Ophthalmol Vis Sci 50(8):3711–3720
Read JC, Begum SF, McDonald A, Trowbridge J (2013) The binocular advantage in visuomotor tasks involving tools. Iperception 4(2):101–110
Bloch E, Uddin N, Gannon L, Rantell K, Jain S (2015) The effects of absence of stereopsis on performance of a simulated surgical task in two-dimensional and three-dimensional viewing conditions. Br J Ophthalmol 99(2):240–245
Biddle M, Hamid S, Ali N (2014) An evaluation of stereoacuity in practising surgeons across a range of surgical specialities. Surgeon 12(1):7–10
Nakagawara V, Wood KJ (1998) Clinical application of the new civil airman vision standards and certification procedures. J Am Optom Assoc 69(3):144–150
Zaroff CM, Knutelska M, Frumkes TE (2003) Variation in stereoacuity: normative description, fixation disparity, and the roles of aging and gender. Invest Ophthalmol Vis Sci 44(2):891–900
Lee SY, Koo NK (2005) Change of stereoacuity with aging in normal eyes. Korean J Ophthalmol 19(2):136–139
Ding J, Levi DM (2011) Recovery of stereopsis through perceptual learning in human adults with abnormal binocular vision. Proc Natl Acad Sci USA 108(37):E733–E741
Bhatt NR, Morris M, O’Neil A, Gillis A, Ridgway PF (2016) When should surgeons retire? Br J Surg 103(1):35–42
Westheimer G (2013) Clinical evaluation of stereopsis. Vis Res 90:38–42
Kurt Simons (1981) A comparison of the frisby, random-dot E, TNO, and randot circles stereotests in screening and office use. Arch Ophthalmol 99(3):446–452
Wong BPH, Woods RL, Peli E (2002) Stereoacuity at distance and near. Optom Vis Sci 79(12):771–778
Ruttum MS (1988) Visual screening with random dot stereograms. Semin Ophthalmol 3(3):175–180
Hoffmann H, Ruiz-Schirinzi R, Goldblum D, Dell-Kuster S, Oertli D, Hahnloser D, Rosenthal R (2014) Impact of examinees’ stereopsis and near visual acuity on laparoscopic virtual reality performance. Surg Today 45(10):1280–1290
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Charlotte Fergo, Dr. Jakob Burcharth, Dr. Hans-Christian Pommergaard and Dr. Jacob Rosenberg have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Fergo, C., Burcharth, J., Pommergaard, HC. et al. Age is highly associated with stereo blindness among surgeons: a cross-sectional study. Surg Endosc 30, 4889–4894 (2016). https://doi.org/10.1007/s00464-016-4826-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4826-9